1. Introduction
Obesity is a major factor contributing to the development of serious medical conditions, including diabetes, hyperlipidemia, and cardiovascular disease. Obesity is also associated with other medical issues such as erectile dysfunction (ED). The prevalence of ED is higher in men with a body mass index (BMI) of 25–30 kg/m2, compared to men with a BMI below 25 kg/m2, and higher still in men with a BMI over 30 kg/m2 [1]. This association is related to both pathophysiological and psychological factors. Pathophysiological factors include reduced synthesis of nitric oxide (NO), lower plasma testosterone levels, endothelial dysfunction, and dyslipidaemia [2]. Psychological factors include low self esteem, stress, and anxiety associated with excessive weight.
Bariatric surgery is a highly effective approach towards the treatment of patients with severe obesity. Significant and long-lasting weight loss is achieved in many cases, as well as the resolution of related comorbidities. As of 2023, there are several bariatric surgery procedures commonly performed, including sleeve gastrectomy (SG), one-anastomosis gastric bypass (OAGB), and Roux-en-Y gastric bypass (RYGB). Bariatric surgery was also shown to have a positive effect on sexual satisfaction and erectile function [3,4,5,6]. This may be related to weight loss [7,8] and overall improved body image [9,10]. However, in many cases, erectile dysfunction may still be a problem after these surgeries.
The first line and most common treatment of erectile dysfunction nowadays is oral phosphodiesterase-5 inhibitors (PDE5i), with attributes of high safety, rapid efficacy and noninvasiveness [11,12]. Following sexual stimulation, NO is released from endothelial cells. NO interacts with guanylyl cyclase in smooth muscle cells, resulting in the synthesis of cGMP from GMP. PDE5i prevents the hydrolysis of cGMP by PDE5, thus allowing penile smooth muscle relaxation, leading to increased arterial blood flow and erection [13]. However, to be effective, these drugs require satisfactory absorption from the gastrointestinal tract (GIT) into the bloodstream, a process dependent upon various factors related to the drug properties, the drug product (formulation, excipients), and the GIT physiology [14,15].
Following bariatric surgery, the GIT anatomy/physiology is significantly altered. 80–90% of the stomach is excised, resulting in decreased gastric volume, acidity, contractility, and residence time [16,17]. These changes may severely hamper the dissolution of the drug dose, a prerequisite for drug absorption [18,19]. Some drugs, including those with limited water solubility, high dose, and a weakly basic nature, are more prone and may be more sensitive to these postbariatric changes than others [20,21].
Sildenafil is the first and main PDE5i, approved for ED treatment, as well as for pulmonary arterial hypertension. It has a weakly basic, pH-dependent solubility nature [22]. Sildenafil is among the 200 most commonly prescribed medications in the US (2020) and the 1st among all ED drugs, with ~3 million prescriptions annually (ClinCalc.com (accesses on 15 December 2023); therefore, it is clinically relevant and significant to study the use of this drug in the growing population of bariatric patients (∼700,000 surgeries annually worldwide). The pH-dependent solubility of sildenafil was studied in vitro, as well as ex vivo, in aspirated gastric contents obtained from patients pre- vs. postbariatric surgery. Then, a recently developed biorelevant in vitro dissolution technique was used to mimic the post-SG/OAGB gastric conditions and study the sildenafil product (Viagra®) dissolution pre- vs. postbariatric surgery. Finally, advanced physiologically based pharmacokinetic (PBPK) models were developed to simulate the absorption and pharmacokinetic changes in sildenafil pre- vs. postbariatric surgery. Altogether, this mechanistic research reveals the complexity involved in pharmacotherapy management after bariatric surgery, attempting to predict potential postbariatric treatment failure in advance for the benefit of this growing patient population.
2. Materials and Methods
2.1. Materials
Sildenafil citrate powder (Carbosynth Limited, Berkshire, UK) was used for the solubility studies. Sildenafil citrate (Viagra®, Pfizer Inc., New York, NY, USA) tablets of 25, 50 and 100 mg were used in the dissolution tests. The following materials from Sigma-Aldrich (Chemie GmbH, Steinheim, Germany) were used for buffer preparation: acetic acid, maleic acid, sodium phosphate monobasic, sodium dodecyl sulfate (SDS), hydrochloric acid, sodium hydroxide, and sodium chloride. Water and acetonitrile of ultraperformance liquid chromatography (UPLC)-grade were purchased from Bio-Lab Ltd. (Ashkelon, Israel).
2.2. In Vitro Solubility
The equilibrium solubility of sildenafil was determined using the shake-flask method, described previously [23,24]. pH 1 and pH 3 (maleate 0.2 M), pH 5 (acetate 0.2 M), and pH 7 (phosphate 0.2 M) buffers were used. Quadruplets (n = 4) for each pH were produced by excess drug powder added to vials containing 500 µL of the solution medium. Vials were incubated for 24 h at 37 °C and shaken at 200 rpm (Orbital Shaker Incubator, MRC Laboratory Instruments, Holon, Israel). Next, the samples were then moved to Eppendorf tubes and centrifuged (Centrifuge 5430 R, Eppendorf®, Hamburg, Germany) at 20,817× g and 37 °C for 10 min. Then, supernatants were diluted as needed (by a factor of 10 or 40, depending on solubility) and immediately analyzed by UPLC-PDA.
2.3. Ex Vivo Solubility
The solubility of sildenafil in gastric fluid was determined using the above-mentioned shake-flask method. Excess drug powder was added to glass vials containing gastric fluid at a fasted state, aspirated from three bariatric patients (one SG, one RYGB, and one OAGB) in the perioperative time through the nasogastric tube, before and one day after surgery. The study protocol was approved by the institutional review board of the Ben-Gurion University School of Medicine (institutional board request number 0248-18-SOR) and informed consent was obtained presurgery from all patients. pH measurements and recording were done immediately after gastric content collection; the content was vortexed, and 2 mL of gastric fluid were centrifuged for 10 min at 20,817× g and 25 °C; 400 µL of supernatant fluid was used in the solubility experiment [20,21]. Samples with appropriate pH [16] and sufficient gastric fluid volume were chosen for the solubility study. The experimental process and conditions were similar to the solubility study in vitro (Section 2.2) with the additional step of sample filtering prior to UPLC analysis. Dilutions were made with an acidic buffer after the removal of any undissolved drug.
2.4. In Vitro Dissolution
The dissolution of sildenafil, 25, 50 and 100 mg whole tablets, was studied in three different conditions: (1) pH 1 maleate, 250 mL medium, using USP dissolution apparatus II (Premiere 5100, Distek®, North Brunswick, NJ, USA), and with a paddle rotated at 100 rpm [25,26]; (2) pH 5 acetate, 50 mL (+0.05% SDS) medium; and (3) pH 7 phosphate, 50 mL (+0.05% SDS) medium, using 50 mL round-bottom flask inside a water bath with a minipaddle rotated at 153 rpm. This rotation-speed calculation was previously described [20,21,27]. SDS was used to prevent precipitation of the dissolved drug. A temperature of 37 ± 0.5 °C was maintained throughout the dissolution study. These conditions mimic the intragastric parameters before and after bariatric surgery, including pH, fluid volume, temperature, and gastric contractility. Samples of 300 µL were drawn at 5, 10, 15, 20, 30, 40, 50, 60, 75, and 90 min, filtered, and centrifuged for 12 min at 20,817× g (37 °C) before UPLC analysis.
2.5. Analytical Method
Sample analysis was performed using UPLC with Waters Acquity H-Class system equipped with a PDA detector and controlled by Empower software (EMP 2 Feature release 5, Built 2154). The analytical method followed the previous publication [28], and it is detailed in . The ambient temperature of the column and samples was used. Linear (R2 = 0.999) calibration curves were obtained for each pH in the relevant drug-concentration ranges. Inter- and intraday coefficients of variation were lower than 1%. The stability of sildenafil over the experimental course was verified.
2.6. Physiologically Based Pharmacokinetic (PBPK) Modeling
Drug-specific PBPK models were constructed using GastroPlus® software (version 9.8.3012; Simulations Plus Inc., Lancaster, CA, USA). The software predicts the dissolution, absorption, and disposition of a drug based on its physicochemical and PK properties, in conjunction with the parameters describing the physiological characteristics of the human gastrointestinal (GI) tract. These physiological parameters are integrated into the software-specific advanced compartmental absorption and transit (ACAT) model of the GI tract and accounted for in a series of differential equations used to simulate the dynamic processes a drug undergoes in the body after peroral administration [29,30]. Physiological parameters describing a healthy human representative in the fasted state were kept at the software default values, except for the % fluid volumes in the small intestine (23%) and colon (0.5%), which were decreased from the default 40% and 10% to 23% and 0.5% [31], respectively, to account for the much smaller GI volumes in vivo [32,33,34]. To account for postbariatric surgery changes in physiological conditions, the ACAT model parameters were manually adjusted, i.e., gastric volume was decreased from default 50 to 10 mL, corresponding to 20% of the presurgery gastric volume [35,36], and gastric transit time was decreased from default 0.25 to 0.12 h [37,38]. The simulations were also performed for bypassed duodenum and jejunum physiology in post-OAGB patients, setting the volume, length, and transit time for the duodenum and jejunum 1 and 2 segments to zero [20,36]. Moreover, stomach pH was increased from default pH 1.3 to pH 5.0 (post-SG) and pH 7.0 (post-OAGB) to account for the influence of the different bariatric procedures and gastric pH on drug dissolution and absorption [16,39]. Intestinal pH was not altered [39].
The input values regarding properties of sildenafil were taken from the literature, in silico predicted (ADMET Predictor® module, version 10.4.0.0; Simulations Plus Inc., Lancaster, CA, USA) based on the structure of the drug or experimentally determined, as depicted in . Drug dissolution throughout the GI tract was calculated using the software default Johnson equation [40] that accounts for a drug’s solubility and particle size. In the absence of data on drug particle size in the commercial products, an approximate value of 100 µm was used for all simulations. Considering the poor aqueous solubility, the models also accounted for the effect of bile salts on drug solubility and dissolution.
Pharmacokinetic parameters describing the distribution and elimination of the tested drug were estimated from the in vivo data on drug plasma concentration over time following intravenous (i.v.) and/or peroral drug dosing, using the software integrated PKPlusTM module and, if needed, further optimized, while keeping the final values within the range reported in literature .
The predictive power of the designed models was assessed by comparing the predicted with the in vivo observed values for the maximum plasma concentration (Cmax), time to reach Cmax (tmax) and area under the plasma concentration time curve (AUC0−inf) for different drug doses given to healthy human subjects in the fasted state. The predicted values referred to a healthy human representative, and the in vivo values were digitized (DigIt software, version 1.0.4; Simulations Plus, Inc., Lancaster, CA, USA) from the mean profiles observed in clinical studies and published in the literature [41,42,43]. A comparison was performed by calculating fold errors between the observed and predicted data, whereas the fold error represents the ratio between the predicted and observed values. According to the commonly applied criteria, a 2-fold error can be considered acceptable for most drugs, although tighter boundaries in the 1.5-fold range could be more appropriate for drugs with, e.g., low variable pharmacokinetics and vice versa, less stringent 2.5-fold criterium may apply for drugs with high pharmacokinetic variability [44,45]. Additionally, the coefficient of determination (R2) was used to evaluate linearity between the observed and predicted values.
3. Results
3.1. Sildenafil Solubility
The in vitro solubility of sildenafil decreased with the increasing pH. At pH 1, the solubility was over 30 mg/mL; however, at pH 7, sildenafil had low solubility, 0.3 mg/mL, representing an over 100-fold decrease. The ex vivo solubility in intragastric contents from pre- vs. postbariatric patients was consistent with the in vitro solubility results showing a >100-fold decreased solubility for sildenafil postsurgery (Figure 1; .
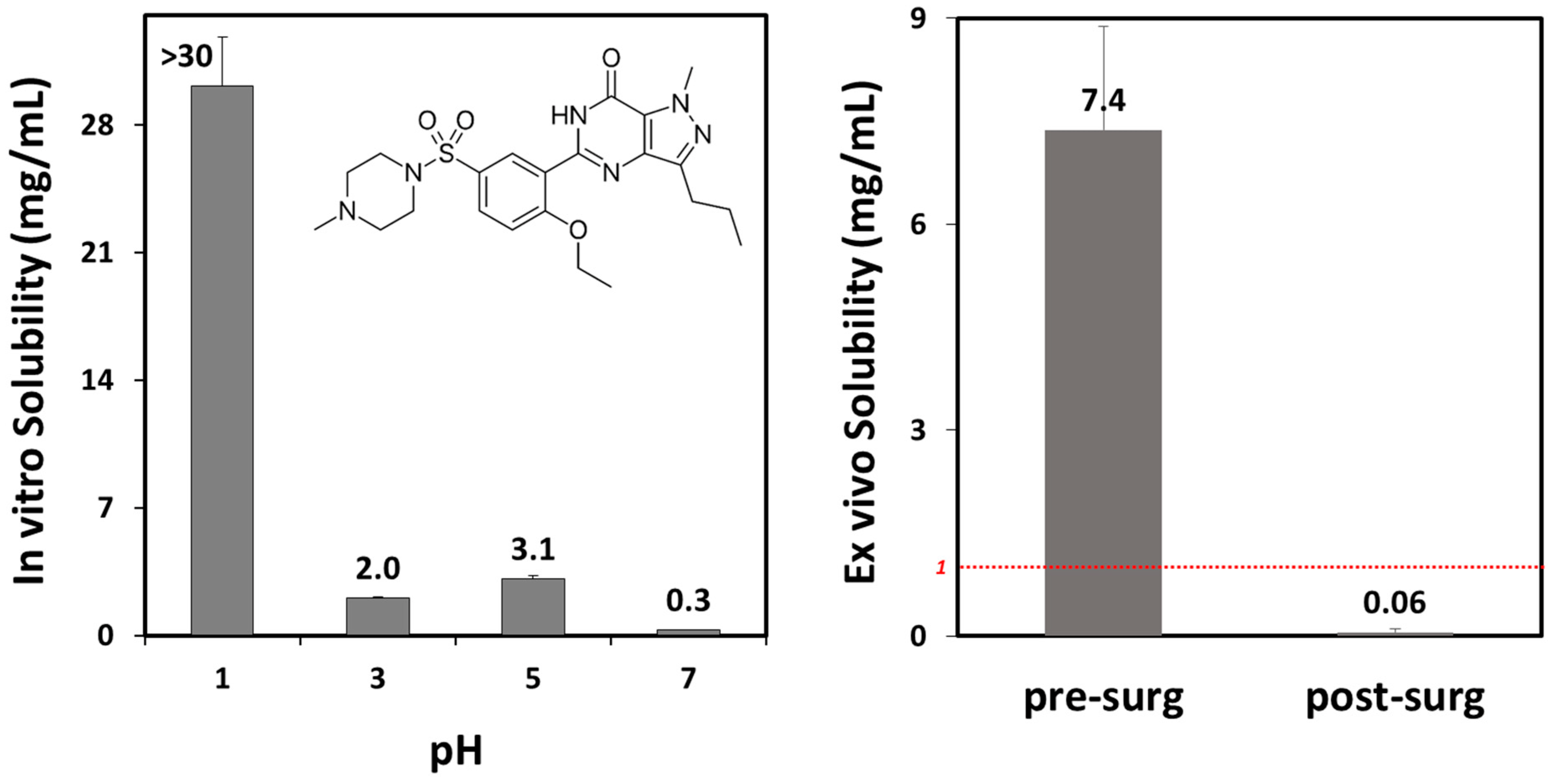
Figure 1. Sildenafil in vitro solubility as a function of pH ((left) panel) and ex vivo solubility in gastric fluid aspirated from three patients before ((left) column; mean pH 2.0) vs. after ((right) column; mean pH 7.0) bariatric surgery. The red dashed line represents the solubility threshold for complete postbariatric dose dissolution. Data presented as mean (SD); n = 4 for each pH; n = 3 for each experimental group.
3.2. In Vitro Dissolution
The dissolution of sildenafil was complete (100%) in presurgery, pH 1 conditions and in post-SG, pH 5 conditions. However, in post-OAGB, pH 7 conditions, sildenafil dissolution was severely hampered, with less than 10% of the sildenafil dissolved from its drug products (Figure 2). In other words, while in presurgery conditions, the dissolution of sildenafil is complete, in postsurgery conditions, sildenafil dissolution depends on the pH.
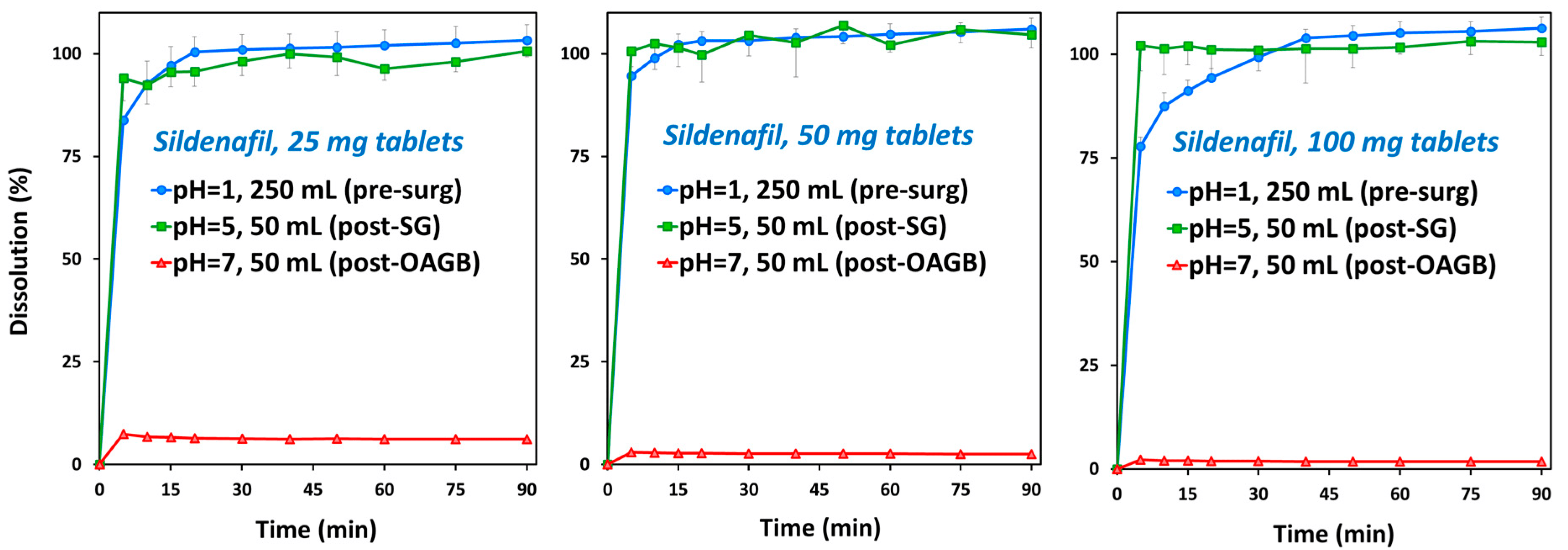
Figure 2. Sildenafil in vitro dissolution of commercially available Viagra® tablets of 25 mg ((left) panel), 50 mg ((middle) panel) and 100 mg ((right) panel). The 250 mL at pH 1 medium (blue circles) represents presurgery stomach state, 50 mL at pH 5 medium (green squares) represents post-SG conditions, and 50 mL at pH 7 medium (red triangles) represents post-OAGB gastric scenario. Average (SD); n = 4 for each experimental group.
3.3. Physiologically Based Pharmacokinetic (PBPK) Simulations
The simulated pharmacokinetic parameters (Cmax, tmax, AUC0−inf) for different oral doses of sildenafil coincide well with the mean data observed in clinical studies , demonstrating the acceptable prediction power of the designed PBPK models. The presurgery simulated plasma concentrations relate well with the available data from human studies, both for 50 mg and 100 mg sildenafil doses (Figure 3). According to the calculated R2 values , there is a linear relationship between the simulated and observed data. The predictions for sildenafil are within the 1.5-fold range (0.67–1.50), except for AUC0−inf for 100 mg sildenafil dose (fold error 0.66) which complies with the two-fold criterion (range between 0.5 and 2.0). A larger deviation of the predicted AUC0−inf from the mean in vivo data in the case of 100 mg sildenafil dose can be explained by a slightly nonproportional increase in systemic drug exposure with an increased drug dose, which was attributed to the saturation of elimination pathways [51]. However, the degree of nonproportionality for doses up to 200 mg is considered small and not clinically significant [49,51]. Moreover, sildenafil exhibits pronounced interindividual pharmacokinetic variability [50] implying that a two-fold prediction error is acceptable for this compound.
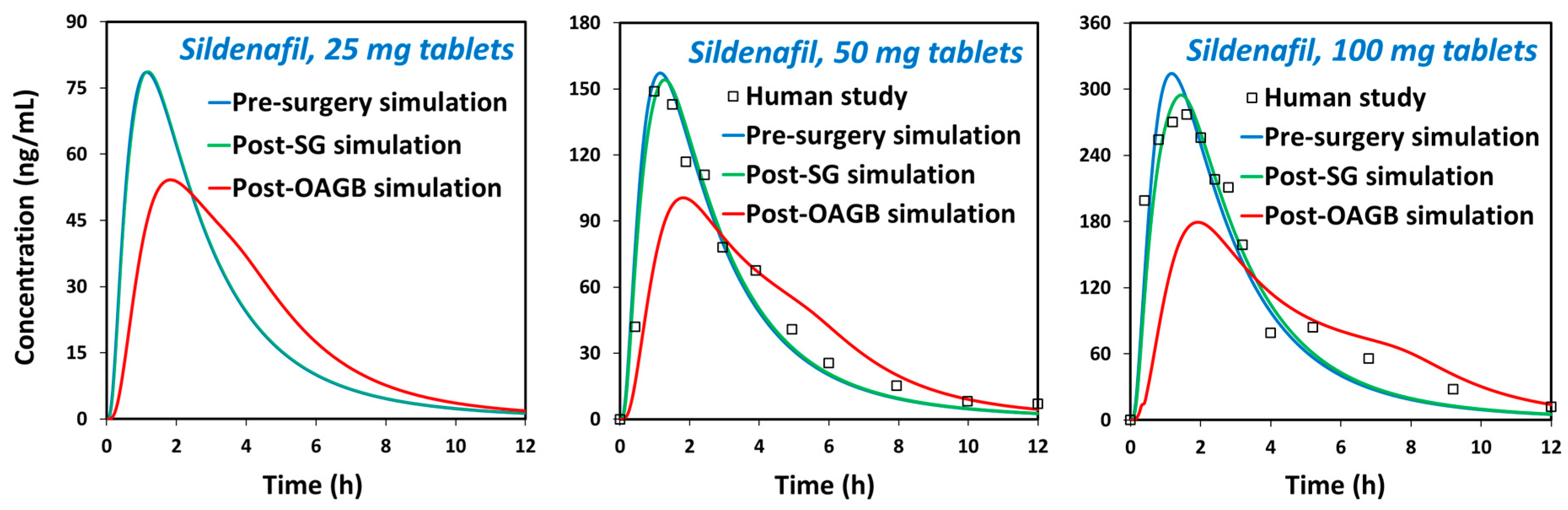
Figure 3. The predicted plasma concentration time profiles under presurgery, post-SG, and post-OAGB states for sildenafil 25 mg ((left) panel), 50 mg ((middle) panel), and 100 mg ((right) panel). Square markers represent the mean values observed in human studies (50 mg, Nichols et al.; 100 mg, Alwhaibi et al.) [41,49].
The designed drug-specific PBPK models were eventually used to estimate in vivo dissolution and absorption of sildenafil in postbariatric vs. nonoperated subjects and to mechanistically explain the combined influence of drug physicochemical and physiological factors on its systemic exposure.
The prediction results for sildenafil (Figure 3, ) indicate delayed drug absorption in postbariatric patients (increased tmax) and reduced Cmax values, especially in post-OAGB patients in comparison to a presurgery state. Moreover, the reduction in Cmax was more pronounced with an increasing drug dose, reaching a 43% reduction in a post-OAGB state for a 100 mg sildenafil dose. Another observation regarding sildenafil plasma exposure is that the increase in stomach pH from pH 5 to pH 7 reduces Cmax and prolonges tmax, which can be explained by delayed overall drug dissolution in cases of less acidic stomach pH (Figure 4, left panel). These results are in line with the experimental data showing a notable decline in drug solubility and postsurgery gastric dissolution when the pH changes from pH 5 to pH 7 (Figure 1 and Figure 2). As a consequence of reduced gastric dissolution, there is a marked drop in sildenafil absorption from the subsequent GI compartment (duodenum in post-SG patients and ileum 1 in post-OAGB patients), as visible from the simulated regional absorption distribution (Figure 4, right panel). However, the overall sildenafil plasma exposure (total percent absorbed in Figure 3 and AUC in ) does not seem to be affected by the altered GI conditions after bariatric surgery. Namely, according to the simulation results, even a 100 mg drug dose will eventually dissolve in the GI tract, and high drug permeability will enable sufficient drug absorption from the subsequent GI compartments (Figure 3 and Figure 4, right panel).
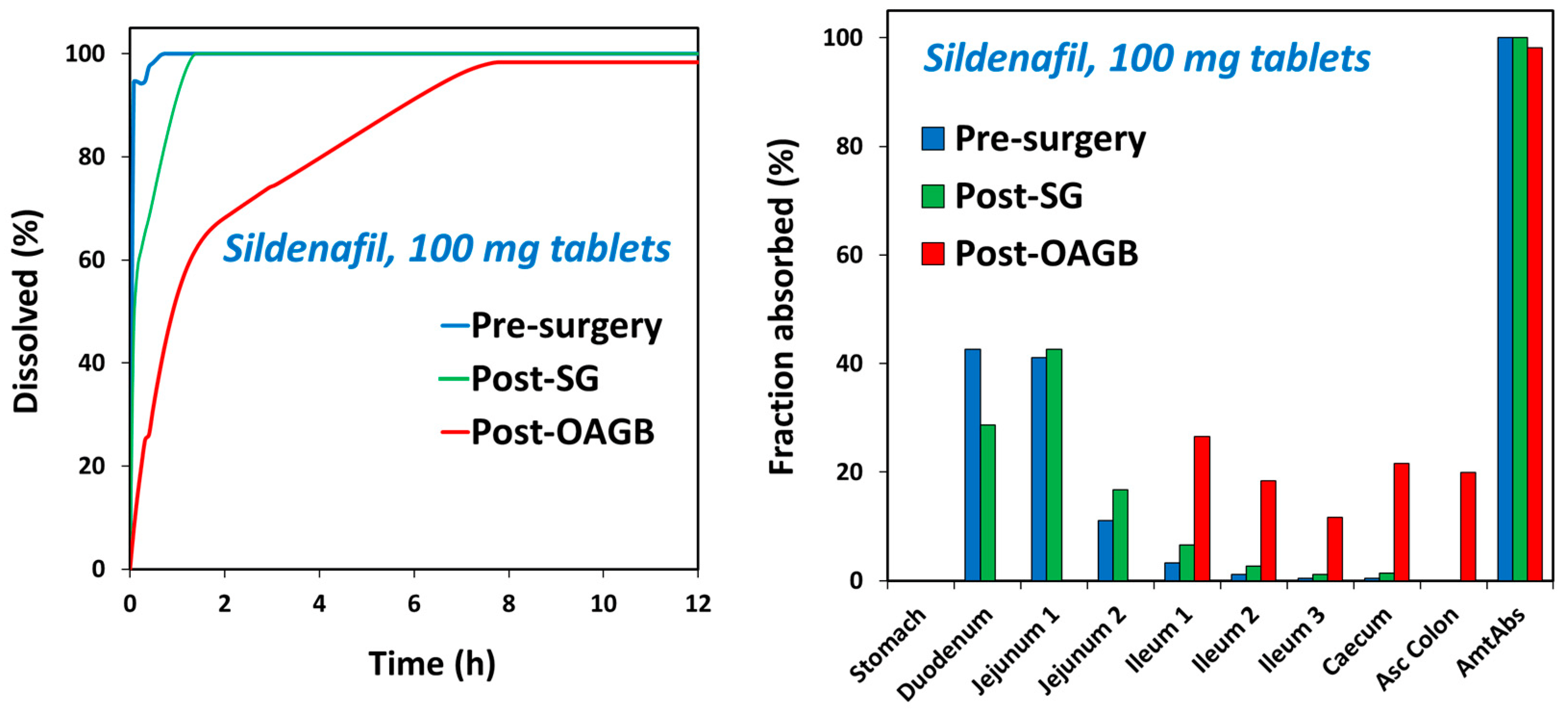
Figure 4. The predicted in vivo dissolution ((left) panel) and the predicted GI tract regional absorption ((right) panel) profiles under presurgery, post-SG, and post-OAGB states for sildenafil 100 mg tablets.
4. Discussion
This work shows that the solubility of sildenafil may be significantly lower in postbariatric conditions, resulting in potentially hampered dissolution of the drug dose. For sildenafil, the postoperative gastric pH is a crucial factor. This observation is attributed to its pKa value of ~6.7 [52], so that highly increased intragastric pH, such as that measured for some postbariatric patients (especially those undergoing bypass procedures) may result in dramatically lower solubility [16]. In fact, low solubility was observed in high pH (~7) gastric fluids from patients after different bariatric procedures. This indicates that, while some patients may have unaltered sildenafil pharmacokinetics after bariatric surgery, others may experience treatment failure related to insufficient drug absorption and exposure [20,53].
Bariatric surgery may prolong the absorption half life, especially in bypass procedures. For many orally administered drugs, absorption occurs from the upper part of the small intestine [54,55], and, when bypassed, the full drug dose may only be absorbed later, as distally as the large intestine [20,56]. It should be highlighted that, particularly with sildenafil, the onset of action is desired to be as immediate as possible, and, hence, altered/delayed absorption (with lower Cmax and longer Tmax) following gastric bypass is detrimental to treatment success, even with an unaffected AUC.
Sildenafil is increasingly popular, and, in the US as of 2020, sildenafil had ~3 million prescriptions [57]. As mentioned, people with obesity are even more likely to experience ED and be treated with PDE5i. Bariatric surgery may improve sexual function among people with obesity; however, no data is available on changes in PDE5i use after surgery [58]. It is likely that many people will still require PDE5i after bariatric surgery. For one, weight loss along with its beneficial effects is not immediate, so continuation is expected for at least the first few months [59]. Second, when the underlying cause of ED is unrelated to weight, then the surgery itself is unlikely to solve the problem. Third, drugs taken by the patients may cause ED, e.g., in psychiatry; a high percentage of people undergoing bariatric surgery have a psychiatric background [60]. In fact, one year after bariatric surgery, the prevalence of psychiatric conditions is even higher than prior to surgery [61]. Many of the most commonly prescribed psychotropic drugs are likely to cause ED, so for these patients, erectile problems may well persist [62]. Fourth, while long-term weight loss is achieved in many cases, the phenomenon of weight regain is well known and quite common [63]. For all these reasons, PDE5i use, and in particular sildenafil, is expected to be highly relevant among patients who underwent bariatric surgery.
Previous studies predicted hampered dissolution, resulting in decreased blood levels for weakly basic drugs with particularly low pKa. These drugs were lamotrigine [21] (pKa = 5.7), loratadine [20] (pKa = 4.5), and etoricoxib (pKa = 4.6) [56]. Here, we showed that a basic drug with pKa in the upper limit of the physiological range (pKa ~6.7) is also sensitive to increased intragastric pH after bariatric surgery, suggesting that multiple other drugs with similar pKa values may also have altered dissolution and absorption following these procedures. One such drug is vardenafil, another important PDE5i; given the high structural similarity and common basic nature, the postbariatric predictions for sildenafil may apply to vardenafil, as well. In this context, no reported interactions between sildenafil/vardenafil and proton pump inhibitors (PPIs) can be found in the literature. This may be so, given that bariatric surgery also involved the removal of at least 80% of the stomach volume, further contributing to the limited solubility/dissolution. This is not the case in patients not having bariatric surgery who use PPIs.
Other mechanisms involved in the pharmacokinetics of these drugs may also be affected by bariatric surgery [64,65,66,67,68]. For example, the activity of CYP3A enzymes is increased with weight loss [69,70,71], and since sildenafil is mainly metabolized by CYP3A4, its postbariatric plasma levels may be further decreased.
It is worth mentioning that another drug in this class, udenafil, is currently available in Korea, Russia, and the Philippines and is yet to be approved for use in the USA by the FDA. It is structurally close to sildenafil and vardenafil but is a stronger base and also contains a weakly acidic group. Thus, it is expected to be far less affected by altered intragastric pH after bariatric surgery. It was also found to be weight negative in mice studies [72], implying suitability for this patient population.
5. Conclusions
Delayed absorption of sildenafil after gastric bypass surgery may suggest that ingestion of this drug shortly before intercourse, as normally indicated, may fail to produce the desired effects. In fact, after gastric bypass, patients using sildenafil may need to take this drug hours in advance, which is suboptimal and impractical, to say the least. Time to effect may change from patient to patient, so predicting the proper timing for taking it may not be possible. Indeed, when PDE5i is considered, the absorption rate is as important as its extent.
The issues addressed in this work should be further elucidated in human studies of the pharmacokinetics and pharmacodynamics of the different PDE5i among patients undergoing bariatric surgery, with special emphasis on the comparison between the different bariatric procedures, most specifically sleeve gastrectomy vs. gastric bypass.
References
- Chitaley, K.; Kupelian, V.; Subak, L.; Wessells, H. Diabetes, obesity and erectile dysfunction: Field overview and research priorities. J. Urol. 2009, 182, S45–S50. [Google Scholar] [CrossRef] [PubMed]
- Akdemir, A.O.; Karabakan, M.; Aktas, B.K.; Bozkurt, A.; Ozgur, E.G.; Akdogan, N.; Yaris, M. Visceral adiposity index is useful for evaluating obesity effect on erectile dysfunction. Andrologia 2019, 51, e13282. [Google Scholar] [CrossRef] [PubMed]
- Minambres, I.; Sarda, H.; Urgell, E.; Genua, I.; Ramos, A.; Fernandez-Ananin, S.; Balague, C.; Sanchez-Quesada, J.L.; Bassas, L.; Perez, A. Obesity Surgery Improves Hypogonadism and Sexual Function in Men without Effects in Sperm Quality. J. Clin. Med. 2022, 11, 5126. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Sun, L.; Jiang, S.; Chen, X.; Zhu, J.; Zhao, X.; Yu, S.; Dong, Z.; Chen, Y.; Zhang, W.; et al. Effects of bariatric surgery on testosterone level and sexual function in men with obesity: A retrospective study. Front. Endocrinol. 2022, 13, 1036243. [Google Scholar] [CrossRef] [PubMed]
- El-Tholoth, H.S.; Bedaiwi, A.K.; Binjawhar, A.; Almulhem, A.A.; Bedaiwi, K.K.; Alshurafa, H.; Alzahrani, T.; Alhussein, R.K.; Alhussein, A.K.; Alnumi, M. Male sexual function after weight-loss surgeries in a group of Saudi population. Urol. Ann. 2021, 13, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Machado, F.P.; Rhoden, E.L.; Pioner, S.R.; Halmenschlager, G.; de Souza, L.V.B.; Lisot, B.C.; Drachler, I.P. Weight Loss Through Bariatric Surgery in Men Presents Beneficial Effects on Sexual Function, Symptoms of Testosterone Deficiency, and Hormonal Profile. Sex. Med. 2021, 9, 100400. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Xu, W.; Wang, T.; Wang, S.; Liu, J.; Jiang, H. Effect of weight loss on erectile function in men with overweight or obesity: A meta-analysis of randomised controlled trials. Andrologia 2022, 54, e14250. [Google Scholar] [CrossRef]
- Mora, M.; Aranda, G.B.; de Hollanda, A.; Flores, L.; Puig-Domingo, M.; Vidal, J. Weight loss is a major contributor to improved sexual function after bariatric surgery. Surg. Endosc. 2013, 27, 3197–3204. [Google Scholar] [CrossRef]
- Fahmy, A.; Abdeldaiem, H.; Abdelsattar, M.; Aboyoussif, T.; Assem, A.; Zahran, A.; Elgebaly, O. Impact of Bariatric Surgery on Sexual Dysfunction in Obese Men. Sex. Med. 2021, 9, 100322. [Google Scholar] [CrossRef]
- Nimbi, F.M.; Virginia, C.; Cinzia, D.M.; Michela, D.T.; Gianfranco, S.; Emanuela, P. The relation between sexuality and obesity: The role of psychological factors in a sample of obese men undergoing bariatric surgery. Int. J. Impot. Res. 2022, 34, 203–214. [Google Scholar] [CrossRef]
- Wang, C.M.; Wu, B.R.; Xiang, P.; Xiao, J.; Hu, X.C. Management of male erectile dysfunction: From the past to the future. Front. Endocrinol. 2023, 14, 1148834. [Google Scholar] [CrossRef] [PubMed]
- Mykoniatis, I.; Pyrgidis, N.; Sokolakis, I.; Ouranidis, A.; Sountoulides, P.; Haidich, A.B.; van Renterghem, K.; Hatzichristodoulou, G.; Hatzichristou, D. Assessment of Combination Therapies vs Monotherapy for Erectile Dysfunction: A Systematic Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2036337. [Google Scholar] [CrossRef] [PubMed]
- Moncada, I.; Martinez-Salamanca, J.; Ruiz-Castane, E.; Romero, J. Combination therapy for erectile dysfunction involving a PDE5 inhibitor and alprostadil. Int. J. Impot. Res. 2018, 30, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Dahan, A.; Beig, A.; Lindley, D.; Miller, J.M. The solubility-permeability interplay and oral drug formulation design: Two heads are better than one. Adv. Drug Deliv. Rev. 2016, 101, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Martinez, M.N.; Amidon, G.L. A mechanistic approach to understanding the factors affecting drug absorption: A review of fundamentals. J. Clin. Pharmacol. 2002, 42, 620–643. [Google Scholar] [CrossRef]
- Porat, D.; Vaynshtein, J.; Gibori, R.; Avramoff, O.; Shaked, G.; Dukhno, O.; Czeiger, D.; Sebbag, G.; Dahan, A. Stomach pH before vs. after different bariatric surgery procedures: Clinical implications for drug delivery. Eur. J. Pharm. Biopharm. 2021, 160, 152–157. [Google Scholar] [CrossRef]
- Steenackers, N.; Vanuytsel, T.; Augustijns, P.; Tack, J.; Mertens, A.; Lannoo, M.; Van der Schueren, B.; Matthys, C. Adaptations in gastrointestinal physiology after sleeve gastrectomy and Roux-en-Y gastric bypass. Lancet Gastroenterol. Hepatol. 2021, 6, 225–237. [Google Scholar] [CrossRef]
- Azran, C.; Wolk, O.; Zur, M.; Fine-Shamir, N.; Shaked, G.; Czeiger, D.; Sebbag, G.; Kister, O.; Langguth, P.; Dahan, A. Oral drug therapy following bariatric surgery: An overview of fundamentals, literature and clinical recommendations. Obes. Rev. 2016, 17, 1050–1066. [Google Scholar] [CrossRef]
- Porat, D.; Dahan, A. Medication Management after Bariatric Surgery: Providing Optimal Patient Care. J. Clin. Med. 2020, 9, 1511. [Google Scholar] [CrossRef]
- Porat, D.; Dukhno, O.; Vainer, E.; Cvijic, S.; Dahan, A. Antiallergic Treatment of Bariatric Patients: Potentially Hampered Solubility/Dissolution and Bioavailability of Loratadine, but Not Desloratadine, Post-Bariatric Surgery. Mol. Pharm. 2022, 19, 2922–2936. [Google Scholar] [CrossRef]
- Porat, D.; Azran, C.; Mualem, Y.; Vainer, E.; Gibori, R.; Vaynshtein, J.; Dukhno, O.; Dahan, A. Lamotrigine therapy in patients after bariatric surgery: Potentially hampered solubility and dissolution. Int. J. Pharm. 2022, 612, 121298. [Google Scholar] [CrossRef] [PubMed]
- Zucchi, A.; Costantini, E.; Scroppo, F.I.; Silvani, M.; Kopa, Z.; Illiano, E.; Petrillo, M.G.; Cari, L.; Nocentini, G. The first-generation phosphodiesterase 5 inhibitors and their pharmacokinetic issue. Andrology 2019, 7, 804–817. [Google Scholar] [CrossRef] [PubMed]
- Beig, A.; Miller, J.M.; Dahan, A. The interaction of nifedipine with selected cyclodextrins and the subsequent solubility-permeability trade-off. Eur. J. Pharm. Biopharm. 2013, 85, 1293–1299. [Google Scholar] [CrossRef] [PubMed]
- Beig, A.; Agbaria, R.; Dahan, A. The use of captisol (SBE7-beta-CD) in oral solubility-enabling formulations: Comparison to HPbetaCD and the solubility-permeability interplay. Eur. J. Pharm. Sci. 2015, 77, 73–78. [Google Scholar] [CrossRef]
- Fassihi, A.R.; Munday, D.L. Dissolution of theophylline from film-coated slow release mini-tablets in various dissolution media. J. Pharm. Pharmacol. 1989, 41, 369–372. [Google Scholar] [CrossRef]
- Silva, O.S.; Souza, C.R.; Oliveira, W.P.; Rocha, S.C. In vitro dissolution studies of sodium diclofenac granules coated with Eudragit L-30D-55 by fluidized-bed system. Drug Dev. Ind. Pharm. 2006, 32, 661–667. [Google Scholar] [CrossRef]
- Sugano, K. Biopharmaceutics Modeling and Simulations: Theory, Practice, Methods, and Applications; Wiley: Hoboken, NJ, USA, 2012. [Google Scholar]
- Beig, A.; Dahan, A. Quantification of carbamazepine and its 10,11-epoxide metabolite in rat plasma by UPLC-UV and application to pharmacokinetic study. Biomed. Chromatogr. 2014, 28, 934–938. [Google Scholar] [CrossRef]
- Agoram, B.; Woltosz, W.S.; Bolger, M.B. Predicting the impact of physiological and biochemical processes on oral drug bioavailability. Adv. Drug Deliv. Rev. 2001, 50 (Suppl. 1), S41–S67. [Google Scholar] [CrossRef]
- Lin, L.; Wong, H. Predicting Oral Drug Absorption: Mini Review on Physiologically-Based Pharmacokinetic Models. Pharmaceutics 2017, 9, 41. [Google Scholar] [CrossRef]
- Jereb, R.; Opara, J.; Bajc, A.; Petek, B. Evaluating the Impact of Physiological Properties of the Gastrointestinal Tract On Drug In Vivo Performance Using Physiologically Based Biopharmaceutics Modeling and Virtual Clinical Trials. J. Pharm. Sci. 2021, 110, 3069–3081. [Google Scholar] [CrossRef]
- Mudie, D.M.; Murray, K.; Hoad, C.L.; Pritchard, S.E.; Garnett, M.C.; Amidon, G.L.; Gowland, P.A.; Spiller, R.C.; Amidon, G.E.; Marciani, L. Quantification of gastrointestinal liquid volumes and distribution following a 240 mL dose of water in the fasted state. Mol. Pharm. 2014, 11, 3039–3047. [Google Scholar] [CrossRef] [PubMed]
- Murray, K.; Hoad, C.L.; Mudie, D.M.; Wright, J.; Heissam, K.; Abrehart, N.; Pritchard, S.E.; Al Atwah, S.; Gowland, P.A.; Garnett, M.C.; et al. Magnetic Resonance Imaging Quantification of Fasted State Colonic Liquid Pockets in Healthy Humans. Mol. Pharm. 2017, 14, 2629–2638. [Google Scholar] [CrossRef] [PubMed]
- Schiller, C.; Frohlich, C.P.; Giessmann, T.; Siegmund, W.; Monnikes, H.; Hosten, N.; Weitschies, W. Intestinal fluid volumes and transit of dosage forms as assessed by magnetic resonance imaging. Aliment. Pharmacol. Ther. 2005, 22, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Elbanna, H.; Emile, S.; El-Hawary, G.E.; Abdelsalam, N.; Zaytoun, H.A.; Elkaffas, H.; Ghanem, A. Assessment of the Correlation Between Preoperative and Immediate Postoperative Gastric Volume and Weight Loss After Sleeve Gastrectomy Using Computed Tomography Volumetry. World J. Surg. 2019, 43, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Almukainzi, M.; Lukacova, V.; Löbenberg, R. Modelling the Absorption of Metformin with Patients Post Gastric Bypass Surgery. J. Diabetes Metab. 2014, 5, 1000353. [Google Scholar] [CrossRef]
- Dahan, A.; Porat, D.; Markovic, M.; Zur, M.; Kister, O.; Langguth, P. Optimized In Silico Modeling of Drug Absorption after Gastric Bypass: The Case of Metformin. Pharmaceutics 2021, 13, 1873. [Google Scholar] [CrossRef]
- Darwich, A.S.; Pade, D.; Rowland-Yeo, K.; Jamei, M.; Asberg, A.; Christensen, H.; Ashcroft, D.M.; Rostami-Hodjegan, A. Evaluation of an In Silico PBPK Post-Bariatric Surgery Model through Simulating Oral Drug Bioavailability of Atorvastatin and Cyclosporine. CPT Pharmacomet. Syst. Pharmacol. 2013, 2, e47. [Google Scholar] [CrossRef]
- Steenackers, N.; Vanuytsel, T.; Augustijns, P.; Deleus, E.; Deckers, W.; Deroose, C.M.; Falony, G.; Lannoo, M.; Mertens, A.; Mols, R.; et al. Effect of sleeve gastrectomy and Roux-en-Y gastric bypass on gastrointestinal physiology. Eur. J. Pharm. Biopharm. 2023, 183, 92–101. [Google Scholar] [CrossRef]
- Lu, A.T.; Frisella, M.E.; Johnson, K.C. Dissolution modeling: Factors affecting the dissolution rates of polydisperse powders. Pharm. Res. 1993, 10, 1308–1314. [Google Scholar] [CrossRef]
- Alwhaibi, A.; Alsanea, S.; Alrabiah, Z.; Alanazi, F.K.; Al-Hadiya, B.M.; Abou-Auda, H.S. Pharmacokinetic profile of sildenafil citrate in healthy Middle Eastern Males: Comparison with other ethnicities. Saudi Pharm. J. 2021, 29, 1498–1505. [Google Scholar] [CrossRef]
- Food and Drug Administration, Center for Drug Evaluation and Research. Viagra (Sildenafil) “Joint Clinical Review” for NDA-20-895. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/NDA/98/viagra/sect7.PDF (accessed on 15 December 2023).
- Gao, X.; O’Gorman, M.; Cook, J.; Shi, H.; LaBadie, R.R. A Randomized, Open-Label, 3-Way Crossover Study to Demonstrate Bioequivalence of Sildenafil Powder for Oral Suspension With Tablets Used Commercially and in Clinical Studies for the Treatment of Pulmonary Arterial Hypertension. Clin. Pharmacol. Drug Dev. 2012, 1, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Abduljalil, K.; Cain, T.; Humphries, H.; Rostami-Hodjegan, A. Deciding on success criteria for predictability of pharmacokinetic parameters from in vitro studies: An analysis based on in vivo observations. Drug Metab. Dispos. 2014, 42, 1478–1484. [Google Scholar] [CrossRef] [PubMed]
- Puttrevu, S.K.; Arora, S.; Polak, S.; Patel, N.K. Physiologically Based Pharmacokinetic Modeling of Transdermal Selegiline and Its Metabolites for the Evaluation of Disposition Differences between Healthy and Special Populations. Pharmaceutics 2020, 12, 942. [Google Scholar] [CrossRef] [PubMed]
- Walker, D.K.; Ackland, M.J.; James, G.C.; Muirhead, G.J.; Rance, D.J.; Wastall, P.; Wright, P.A. Pharmacokinetics and metabolism of sildenafil in mouse, rat, rabbit, dog and man. Xenobiotica 1999, 29, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Macente, J.; Nauwelaerts, N.; Russo, F.M.; Deprest, J.; Allegaert, K.; Lammens, B.; Hernandes Bonan, R.; Turner, J.M.; Kumar, S.; Diniz, A.; et al. PBPK-based dose finding for sildenafil in pregnant women for antenatal treatment of congenital diaphragmatic hernia. Front. Pharmacol. 2023, 14, 1068153. [Google Scholar] [CrossRef] [PubMed]
- Salerno, S.N.; Edginton, A.; Gerhart, J.G.; Laughon, M.M.; Ambalavanan, N.; Sokol, G.M.; Hornik, C.D.; Stewart, D.; Mills, M.; Martz, K.; et al. Physiologically-Based Pharmacokinetic Modeling Characterizes the CYP3A-Mediated Drug-Drug Interaction Between Fluconazole and Sildenafil in Infants. Clin. Pharmacol. Ther. 2021, 109, 253–262. [Google Scholar] [CrossRef]
- Nichols, D.J.; Muirhead, G.J.; Harness, J.A. Pharmacokinetics of sildenafil after single oral doses in healthy male subjects: Absolute bioavailability, food effects and dose proportionality. Br. J. Clin. Pharmacol. 2002, 53 (Suppl. 1), 5S–12S. [Google Scholar] [CrossRef]
- Jetter, A.; Kinzig-Schippers, M.; Walchner-Bonjean, M.; Hering, U.; Bulitta, J.; Schreiner, P.; Sorgel, F.; Fuhr, U. Effects of grapefruit juice on the pharmacokinetics of sildenafil. Clin. Pharmacol. Ther. 2002, 71, 21–29. [Google Scholar] [CrossRef]
- Gupta, M.; Kovar, A.; Meibohm, B. The clinical pharmacokinetics of phosphodiesterase-5 inhibitors for erectile dysfunction. J. Clin. Pharmacol. 2005, 45, 987–1003. [Google Scholar] [CrossRef]
- Barbas, R.; Llinas, A.; Prohens, R. The Solid State Landscape of the Sildenafil Drug. J. Pharm. Sci. 2022, 111, 1104–1109. [Google Scholar] [CrossRef]
- Mitra, A.; Kesisoglou, F. Impaired drug absorption due to high stomach pH: A review of strategies for mitigation of such effect to enable pharmaceutical product development. Mol. Pharm. 2013, 10, 3970–3979. [Google Scholar] [CrossRef] [PubMed]
- Masaoka, Y.; Tanaka, Y.; Kataoka, M.; Sakuma, S.; Yamashita, S. Site of drug absorption after oral administration: Assessment of membrane permeability and luminal concentration of drugs in each segment of gastrointestinal tract. Eur. J. Pharm. Sci. 2006, 29, 240–250. [Google Scholar] [CrossRef] [PubMed]
- Abuhelwa, A.Y.; Foster, D.J.R.; Upton, R.N. A Quantitative Review and Meta-models of the Variability and Factors Affecting Oral Drug Absorption-Part II: Gastrointestinal Transit Time. AAPS J. 2016, 18, 1322–1333. [Google Scholar] [CrossRef] [PubMed]
- Porat, D.; Dukhno, O.; Partook-Maccabi, M.; Vainer, E.; Cvijic, S.; Dahan, A. Selective COX-2 inhibitors after bariatric surgery: Celecoxib, etoricoxib and etodolac post-bariatric solubility/dissolution and pharmacokinetics. Int. J. Pharm. 2023, 645, 123347. [Google Scholar] [CrossRef] [PubMed]
- ClinCalc.com. The Top 300 Drugs of 2020. Available online: https://clincalc.com/DrugStats/Top300Drugs.aspx (accessed on 15 December 2023).
- Liu, S.; Cao, D.; Ren, Z.; Li, J.; Peng, L.; Zhang, Q.; Cheng, B.; Cheng, Z.; Ai, J.; Zheng, X.; et al. The relationships between bariatric surgery and sexual function: Current evidence based medicine. BMC Urol. 2020, 20, 150. [Google Scholar] [CrossRef] [PubMed]
- Tenhagen, M.; van Ramshorst, G.H.; Demirkiran, A.; Hunfeld, M.A.; Cense, H.A. Perioperative Online Weight Monitoring in Bariatric Surgery with a Digital Internet-Connected Scale. Obes. Surg. 2016, 26, 1120–1126. [Google Scholar] [CrossRef] [PubMed]
- Sockalingam, S.; Leung, S.E.; Wnuk, S.; Cassin, S.E.; Yanofsky, R.; Hawa, R. Psychiatric Management of Bariatric Surgery Patients: A Review of Psychopharmacological and Psychological Treatments and Their Impact on Postoperative Mental Health and Weight Outcomes. Psychosomatics 2020, 61, 498–507. [Google Scholar] [CrossRef] [PubMed]
- Becerra, A.Z.; Khalid, S.I.; Morgenstern, A.S.; Rembert, E.A.; Carroll, M.M.; Omotosho, P.A.; Torquati, A. The Association Between Bariatric Surgery and Psychiatric Disorders: A National Cohort Study. Obes. Surg. 2022, 32, 1110–1118. [Google Scholar] [CrossRef]
- Trinchieri, M.; Trinchieri, M.; Perletti, G.; Magri, V.; Stamatiou, K.; Cai, T.; Montanari, E.; Trinchieri, A. Erectile and Ejaculatory Dysfunction Associated with Use of Psychotropic Drugs: A Systematic Review. J. Sex. Med. 2021, 18, 1354–1363. [Google Scholar] [CrossRef]
- El Ansari, W.; Elhag, W. Weight Regain and Insufficient Weight Loss After Bariatric Surgery: Definitions, Prevalence, Mechanisms, Predictors, Prevention and Management Strategies, and Knowledge Gaps-a Scoping Review. Obes. Surg. 2021, 31, 1755–1766. [Google Scholar] [CrossRef]
- Porat, D.; Markovic, M.; Zur, M.; Fine-Shamir, N.; Azran, C.; Shaked, G.; Czeiger, D.; Vaynshtein, J.; Replyanski, I.; Sebbag, G.; et al. Increased Paracetamol Bioavailability after Sleeve Gastrectomy: A Crossover Pre- vs. Post-Operative Clinical Trial. J. Clin. Med. 2019, 8, 1949. [Google Scholar] [CrossRef] [PubMed]
- Dahan, A.; Porat, D.; Azran, C.; Mualem, Y.; Sakran, N.; Abu-Abeid, S. Lithium Toxicity with Severe Bradycardia Post Sleeve Gastrectomy: A Case Report and Review of the Literature. Obes. Surg. 2019, 29, 735–738. [Google Scholar] [CrossRef] [PubMed]
- Margolin, N.; Porat, D.; Dahan, A.; Lavon, O. Influence of Bariatric Surgery on Levetiracetam Clinical Effectiveness: Case Series. Obes. Surg. 2022, 32, 2795–2796. [Google Scholar] [CrossRef] [PubMed]
- Azran, C.; Porat, D.; Fine-Shamir, N.; Hanhan, N.; Dahan, A. Oral levothyroxine therapy postbariatric surgery: Biopharmaceutical aspects and clinical effects. Surg. Obes. Relat. Dis. 2019, 15, 333–341. [Google Scholar] [CrossRef]
- Porat, D.; Azran, C.; Kais, H.; Dahan, A. Managing the Unpredictable: Mechanistic Analysis and Clinical Recommendations for Lamotrigine Treatment after Bariatric Surgery. J. Clin. Med. 2021, 10, 5627. [Google Scholar] [CrossRef]
- Kvitne, K.E.; Robertsen, I.; Skovlund, E.; Christensen, H.; Krogstad, V.; Wegler, C.; Angeles, P.C.; Wollmann, B.M.; Hole, K.; Johnson, L.K.; et al. Short- and long-term effects of body weight loss following calorie restriction and gastric bypass on CYP3A-activity—A non-randomized three-armed controlled trial. Clin. Transl. Sci. 2022, 15, 221–233. [Google Scholar] [CrossRef]
- Zarezadeh, M.; Saedisomeolia, A.; Shekarabi, M.; Khorshidi, M.; Emami, M.R.; Muller, D.J. The effect of obesity, macronutrients, fasting and nutritional status on drug-metabolizing cytochrome P450s: A systematic review of current evidence on human studies. Eur. J. Nutr. 2021, 60, 2905–2921. [Google Scholar] [CrossRef]
- Porat, D.; Margolin, N.; Lavon, O.; Dahan, A. Carbamazepine Therapy After Bariatric Surgery: Eight Sleeve Gastrectomy Cases and Review of the Literature. Obes. Surg. 2022, 32, 3481–3486. [Google Scholar] [CrossRef]
- Ryu, S.Y.; Choi, Y.J.; Park, S.Y.; Kim, J.Y.; Kim, Y.D.; Kim, Y.W. Udenafil, a Phosphodiesterase 5 Inhibitor, Reduces Body Weight in High-Fat-Fed Mice. World J. Mens. Health 2018, 36, 41–49. [Google Scholar] [CrossRef]

