1. Introduction
Obesity is currently a prevalent health issue and one of the foremost public health challenges worldwide. In the last four decades, there has been a rise in the prevalence of childhood obesity among children aged 5 to 19 years in most regions and countries. In 2016, it was determined that the number of obese young children (<5 years old) globally exceeded 41 million. Additionally, there has been a noticeable increase in the occurrence of severe obesity (morbid, extreme obesity) in progressively younger age groups.
It is well established that excess body weight in adults is linked to comorbid cardiometabolic and psychosocial diseases as well as premature mortality. Complications of obesity, leading to at least 2.6 million annual deaths, are increasingly diagnosed in individuals under 18 years of age [1].
The global surge in childhood obesity can be attributed to various factors. Firstly, there has been a widespread shift in the diets of young people. Scientific evidence unequivocally confirms a significant increase in both the size and frequency of meals consumed by children and adolescents over the last 40 years. There is also a notable rise in the consumption of high-energy, processed foods that are rich in fats and sugars but deficient in vitamins, minerals, and other essential microelements. Simultaneously, lifestyle changes resulting from progressive urbanization have compelled a reduction in physical activity.
Equally important is the exposure of children and adolescents to chronic stress stimuli, inadequate stress coping mechanisms, a lack of support, and disruptions in their length and quality of sleep. These factors indirectly lead to the development of compensatory mechanisms, often associated with the consumption of excess high-calorie foods and drinks, even at night. All these environmental factors strongly interact with genetic predisposition, which significantly influences body weight control [2]. Obesity, being a multifaceted health concern, necessitates a nuanced understanding of its diverse complications, both obvious and non-obvious. Non-obvious complications refer to health issues or consequences that may not be immediately apparent or visible, especially in the early stages of obesity. These complications may not present obvious physical symptoms or signs, making their detection and diagnosis more challenging. Non-obvious complications may involve subtle or internal changes that can have significant impacts on health over time. Identifying and understanding these non-obvious complications is crucial for comprehensive healthcare, as it enables early intervention and targeted management to mitigate potential risks associated with obesity. The study’s objective is to identify and discuss non-obvious complications of obesity in children, contributing to a better understanding of the mechanisms accompanying childhood obesity.
2. Methods
A search using the keywords “obvious” and “non-obvious” obesity complications was conducted across the PubMed, Cochrane Library, Science Direct, and EBSCO databases from January 2023 to September 2023. The objective was to identify worldwide English-language meta-analyses, systematic reviews, randomized clinical trials, and observational studies. As a result, the complications identified in children are shown in Figure 1. Ultimately, the following 4 main topics were identified: disorders of glucose metabolism; liver disease related to childhood obesity; the relationship between respiratory disorders and obesity in children; and the effects of obesity on the hypothalamic–pituitary–gonadal axis and puberty.
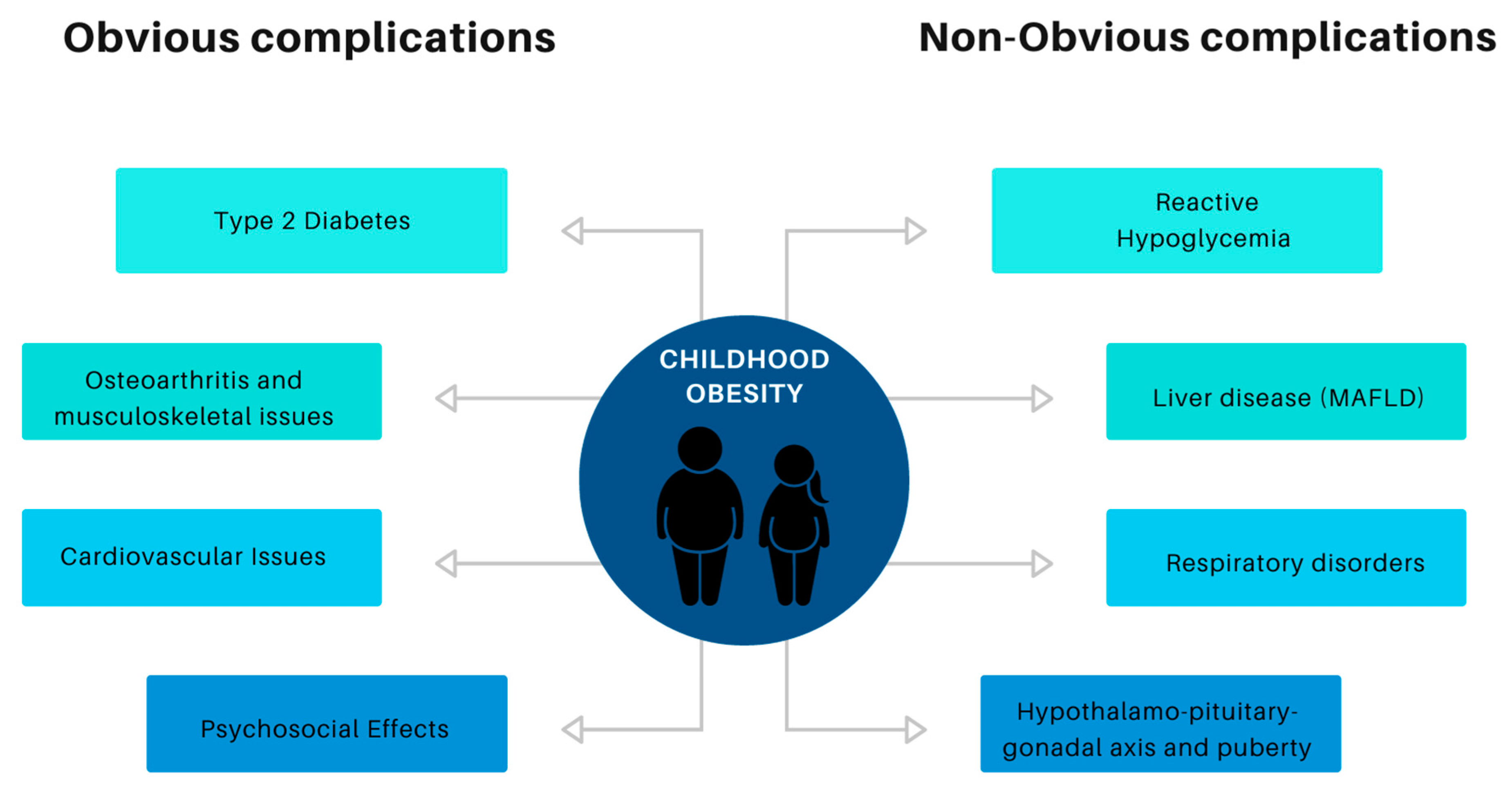
Figure 1. Classification of complications of childhood obesity.
3. Disorders of Glucose Metabolism
Overt and persistent hyperglycemia in obese children is not as common as in adults [3]. Type 2 diabetes occurs in only 1–2% of obese pediatric patients, with the highest prevalence only in genetically predisposed ethnic groups, for example, Native American, Canadian First Nation, Indigenous Australian, African American, Hispanic, etc. This does not mean, however, that the pediatric population affected by obesity is free from glucose metabolism disorders [4]. However, they may be less obvious, such as reactive hypoglycemia. The term “reactive hypoglycemia” was first used in 1924 by Harris, who used this name to describe a set of symptoms similar to those occurring in diabetic patients after insulin administration [5]. Symptoms such as feelings of hunger and behavioral and mood disorders, from agitation and irritation to slowness and drowsiness, weakness, even loss of consciousness, increased sweating, and heart palpitations, occur in people without diabetes and are associated with a rapid decrease in blood glucose concentration in response to a carbohydrate-rich food stimulus. Symptoms disappear after consuming simple carbohydrates. Their direct cause is the incorrect secretion of insulin at a time and in an amount that is not adapted to the body’s current needs. Recent studies indicate that individuals with obesity may have blood glucose levels below 70 mg/dL without significant hypoglycemic symptoms, except for hunger. [6]. That, in turn, may be responsible for snacking behavior [7]. The cause of reactive hypoglycemia is inappropriate insulin secretion. In children with obesity and reactive hypoglycemia, the first phase of insulin secretion is altered in response to the carbohydrates supplied. Subsequently, a large amount of insulin is secreted as a compensatory factor, and, as a consequence, serum glucose concentration is excessively reduced 3–5 h after a meal. As shown in studies using continuous glucose monitoring, reactive hypoglycemia may be experienced by up to 50% of obese patients during an oral glucose tolerance test (OGTT) [6]. Interestingly, only a few report the symptoms described above. In the rest, the disorder is asymptomatic. Traditional glucose measurements involving venipuncture or finger pricks fail to capture the exact fluctuations in blood glucose over time, specifically the variability in glucose levels. Disorders can only be documented using continuous glucose monitoring systems. Alternatively, when interpreting OGTT results, it is worth paying attention not only to the high glycemia values at 120 min after a load but also to those that are within the reference range but are lower than the preload glycemia values. In obese patients with symptoms typical of reactive hypoglycemia or an uncontrollable tendency to snack on sweet snacks, it is worth considering a prolonged oral glucose tolerance test (up to 180 or 240 min) [7]. The basis of treatment is to modify the diet and make the patient aware of the importance of eating regular, well-composed meals and avoiding carbohydrates in the diet. In some situations, metformin or GLP-1 analogues may be helpful. That, however, needs further investigation in the pediatric population.
4. Liver Disease Related to Childhood Obesity
One of the many complications related to childhood obesity is pediatric fatty liver disease associated with metabolic dysfunction (MAFLD), previously known as non-alcoholic liver disease (NAFLD). The diagnostic criteria include liver histology (biopsy), imaging (ultrasound, MRI), or blood sampling (evidence of intrahepatic fat accumulation). It is crucial to underline that the relatively new name MAFLD emphasizes the importance of metabolic causes of the disease, which were not previously included in NAFLD.
In the last two decades, the prevalence of this disease has doubled, and estimates for the European pediatric population vary from 13% to 25% among children aged 3–18 years, depending on the diagnostic criteria. [8,9]. Among obese children in the USA, approximately 38% are estimated to have fatty liver disease [10]. In a Polish retrospective study, steatosis was reported in 4.2% of children aged 6 months to 18 years, with 55.6% of these children being overweight [11].
The manifestations of MAFLD may include steatosis alone, steatohepatitis with and without fibrosis, or even cirrhosis. Since a definitive diagnosis requires a liver biopsy, which is an invasive procedure, the disease is often suspected based on biochemical results (elevated aspartate aminotransferase (AST) or alanine aminotransferase (ALT) concentrations) or imaging, particularly a liver ultrasound, including elastography. A study conducted among adults in the USA using ultrasound elastography showed that 24% of participants had steatosis and 4.4% had significant fibrosis [12]. A corresponding study among obese children revealed that both AST and ALT were significantly higher than in the norm-weight control group. Additionally, 25% of participants showed steatosis on an ultrasound, and elastography showed higher values reflecting fibrosis in the obese pediatric population [13]. The long-term results of MAFLD are not completely defined, as much of the data, especially among the pediatric population, come from retrospective studies and case reports [14,15]. Nevertheless, it is important to underline that, although rare, severe complications such as cirrhosis, liver failure, and hepatocarcinomas have been reported [16]. Obesity in late adolescence and early adulthood appears to increase the risk of severe MAFLD complications, such as liver cancer [17]. The duration of the disease may also play an important role. Two randomized controlled trials among pediatric patients with fatty liver disease showed disease progression in a two-year span, based on histological examinations. Disease progression was also correlated with insulin resistance [18]. According to studies focusing on children who underwent liver biopsy due to fatty liver disease, up to 70% of them showed some degree of fibrosis by the time of diagnosis, including advanced fibrosis in 16–30% of cases. End-stage liver failure requiring liver transplantation due to fatty liver disease was reported even in very young children. According to the USA transplantation registry, from 1987 to 2012, 14 children younger than 18 underwent this procedure [19]. The severity of MAFLD appears to be linked to both the age of the patient and the stage of the disease. It is also twice as common in adolescents with type 2 diabetes [20]. Nevertheless, when treating an obese pediatric patient with fatty liver disease, it is crucial to remember to look for other treatable causes of liver dysfunction, especially if there is poor improvement after weight loss, such as Wilson’s disease, viral hepatitis, or autoimmune hepatitis.
5. Relationship between Respiratory Disorders and Obesity in Children
Asthma is a prevalent chronic disease among children, with a prevalence varying between 1% and 18% [21]. The recently observed rise in the occurrence of obesity and asthma in the pediatric group and their interrelation has been the subject of numerous studies [22]. However, this connection is not well understood [23,24,25]. We often encounter a vicious cycle where asthma contributes to obesity and vice versa. In children with inadequately managed asthma, multiple factors are typically at play, including the utilization of systemic corticosteroids or decreased physical activity. These factors can ultimately disrupt carbohydrate metabolism and elevate the risk of obesity.
Recent findings have indicated a potential connection between the development of asthma and gradual weight gain over time [22,26,27,28]. According to Lang et al., school-aged children before reaching puberty are most susceptible to developing asthma linked to obesity, specifically those between the ages of 7 and 11 [29]. Their suggestion was that the initiation of asthma could be influenced by both the duration and severity of being overweight, and they proposed that the period before puberty, especially among girls, might be a particularly high-risk timeframe for the development of asthma associated with obesity. In their study, Chen et al. monitored the emergence of obesity over a 10-year follow-up in children with asthma. They noted that children who were not obese initially had a 51% greater likelihood of developing obesity when compared to children who did not have a prior asthma diagnosis. Nonetheless, the presence of obesity was not directly linked to the future development of asthma [29,30,31].
Asthma presents with clinically diverse symptoms, such as wheezing, shortness of breath, chest tightness, and cough, all originating from chronic airway inflammation. Obesity has been associated with a decline in lung function, as both forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) exhibit a negative correlation with waist circumference [32,33,34]. On average, every 1 cm increase in waist circumference was linked to a 13 mL decrease in FEV1 and an 11 mL decrease in FVC [35].
The “Obese-Asthma” phenotype displays a distinct molecular pattern compared to the classic form. The Th2-low pattern is characterized by a predominant presence of neutrophils in the bronchial mucosa, alongside low levels of IgE and limited eosinophilic infiltration [36,37]. Excessive adipose tissue accumulation has proinflammatory effects associated with increased leptin production, hypoxia, focal adipocyte necrosis, and activation of neutrophils, reactive oxygen, macrophages, and natural killer cells [38]. Additionally, obesity-related insulin resistance generates proinflammatory molecules, promoting the development of inflammation [28,39]. Furthermore, coexisting hyperinsulinemia, by inhibiting the presynaptic processes of M2 muscarinic receptors, leads to bronchial hyperreactivity. In the research conducted by Leija-Martínez et al., the presence of “Obese-asthma” alongside an elevated Th17 immune response was correlated with airway hyperreactivity (AHR), severe asthma, and resistance to corticosteroid treatment [28,39,40,41].
In the study by Machado et al., it was found that leptin may be a potential predictor of asthma control in children. A weak predictive value was shown for BMI and adiponectin [42].
Elevated levels of CRP, often observed in obese patients due to cytokine stimulation from adipose tissues, have been correlated with the risk of asthma development and its severity [34]. Excessive abdominal tissue deposition also exerts a mechanical influence on the respiratory system by reducing chest expansion and decreasing tidal volume and residual capacity [43]. Afshar-Mohajer et al.’s research revealed that obese children with asthma are more susceptible to the effects of air pollution, specifically PM 2.5, compared to non-obese children. This increased susceptibility was attributed to their higher tidal volumes and minute ventilation. These factors contribute to an elevated risk of experiencing more severe and uncontrolled asthma [44].
The primary approach to addressing pediatric obesity involves lifestyle modifications, including moderate energy consumption, increased physical activity, decreased sedentary behaviors, and active family engagement in the treatment process. Weight reduction in asthmatic children not only decreases the clinical symptoms of asthma but also improves lung function and asthma control, leading to a better quality of life [45]. It has been reported that even a 5–10% reduction in weight can result in improved asthma outcomes [46]. Willeboardse et al. conducted a study monitoring 87 children who were both asthmatic and overweight or obese over 18 months [45]. The intervention involved a combination of activities, including sports sessions, dietary adjustments, parental participation, counseling, and behavioral therapy. Over the course of the study, clinically significant improvements in body weight, lung function, and asthma-related characteristics were observed in both the intervention and control groups. However, certain effects were more prominent in the intervention group, such as FVC, asthma control, and overall quality of life. This suggests that weight-reduction interventions can have clinical benefits for children with asthma.
It is important to note that steroids are less effective for individuals with asthma who are obese compared to those with a lower BMI [47]. Specifically, obese individuals, particularly those with severe obesity, have a reduced likelihood of achieving asthma control. While there have been conflicting reports on this matter, a retrospective cohort study involving data from six European centers found that obesity was not considered a significant risk factor for asthma exacerbations [48]. Up to 40% of children and adolescents with obesity may experience obesity hypoventilation syndrome (OHS) [49]. It typically manifests during sleep through recurrent episodes of either shallow breathing or complete cessation of airflow through the upper airways while chest and abdominal movements continue. Signs of OHS may encompass mouth breathing, disruptions in breathing rhythms, nighttime snoring, difficulties with concentration, as well as restlessness, headaches, and excessive daytime drowsiness. Ventilation dysfunction leads to multiple episodes of hypoxia and hypercapnia, negatively affecting the functioning of the entire body, including growth, development, and psycho-emotional well-being, and leading to the development of other complications of obesity, such as hypertension [50]. Several studies have explored the connection between body mass index measurements and lung function parameters, along with polysomnographic evaluations, in children with asthma. In a retrospective study that examined the polysomnographic data of 448 children aged 7 to 18 years with asthma, efforts were made to investigate the relationship between spirometry results, body mass index, and polysomnography parameters. This analysis also considered the influence of the medications administered. The study revealed that obese children had less favorable sleep patterns and more pronounced disruptions in gas exchange compared to children of normal weight. Additionally, it was found that asthma medications, such as inhaled glucocorticosteroids and leukotriene antagonists, had an impact on sleep pattern disturbances, consequently triggering pathological activations of the sympathetic nervous system. Recognizing the presence of “obesity-related asthma” is vital to initiating personalized interventions for children. These interventions aim to encourage physical activity, cultivate healthy habits, and improve asthma self-care, ultimately reducing long-term morbidity and mortality.
6. Effects of Obesity on the Hypothalamic–Pituitary–Gonadal Axis and Puberty
6.1. Obese Girls
The increasing number of obese children is associated with a broad spectrum of gynecological consequences for adolescent girls, impacting them during adolescence and later in adulthood. Precocious puberty may have adverse effects on girls’ mental and psychosocial health. Obesity heightens the risk of low self-esteem and depression, particularly in girls who are prone to engaging in risky sexual conduct and demonstrate ineffective use of contraception. Irregular menses, amenorrhea, abnormal uterine bleeding, dysmenorrhea, and polycystic ovary syndrome (PCOS) at heightened rates may contribute to infertility, pregnancy complications, as well as breast and endometrial cancers later in adult life [51,52,53,54,55,56,57].
6.2. Obese Boys
7. Summary
We envision that the insights provided in this study will significantly contribute to awareness and understanding of the often-overlooked and non-obvious complications associated with obesity. By shedding light on these intricacies, we aim to empower healthcare professionals with knowledge that can drive more informed decisions and interventions. Obesity, being a multifaceted health concern, necessitates a nuanced understanding of its diverse complications. This work endeavors to unravel its complexities, offering a comprehensive perspective that surpasses surface-level manifestations. This way, we aspire to bridge the gap in knowledge. Moreover, by highlighting non-obvious complications, we aspire to inspire a paradigm shift in how obesity is perceived and managed. Recognizing that certain complications may lurk beneath the surface, undetected for extended periods, underscores the importance of vigilant and comprehensive healthcare practices. Our hope is that this work serves as a catalyst for ongoing research, policy development, and community initiatives aimed at preventing and managing obesity-related complications.
Through increased awareness and a more profound understanding, we can work toward more effective prevention strategies, early interventions, and holistic approaches that address both the visible and concealed challenges posed by obesity.
References
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- Childhood Obesity: Position Statement of Polish Society of Pediatrics, Polish Society for Pediatric Obesity, Polish Society of Pediatric Endocrinology and Diabetes, the College of Family Physicians in Poland and Polish Association for Study on Obesity. Nutrients 2022, 14, 3806. [CrossRef]
- Wójcik, M.; Bociąga, M.; Ciuk, K.; Witczak, Z.; Januś, D.; Furtak, A.; Ruszała, A.; Starzyk, J.B. Prevalence of glucose metabolism disorders in a cohort of children and adolescents with obesity. Acta Paediatr. 2020, 109, 2364–2365. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.S.; Zeitler, P.S.; Wong, J.; Pena, A.S.; Wicklow, B.; Arslanian, S.; Chang, N.; Fu, J.; Dabadghao, P.; Pinhas-Hamiel, O.; et al. ISPAD Clinical Practice Consensus Guidelines 2022: Type 2 diabetes in children and adolescents. Pediatr. Diabetes 2022, 23, 72–902. [Google Scholar] [CrossRef] [PubMed]
- Harris, S. Hyperinsulinism and dysinsulinism. JAMA 1924, 83, 729–733. [Google Scholar] [CrossRef]
- Kishimoto, I.; Ohashi, A. Subclinical Reactive Hypoglycemia Is Associated with Higher Eating and Snacking Frequencies in Obese or Overweight Men without Diabetes. Endocrines 2022, 3, 530–537. [Google Scholar] [CrossRef]
- Kishimoto, I. Subclinical Reactive Hypoglycemia with Low Glucose Effectiveness-Why We Cannot Stop Snacking Despite Gaining Weight. Metabolites 2023, 13, 754. [Google Scholar] [CrossRef]
- Sarin, S.K.; Kumar, M.; Eslam, M.; George, J.; Al Mahtab, M.; Akbar, S.M.F.; Jia, J.; Tian, Q.; Aggarwal, R.; Muljono, D.H.; et al. Liver diseases in the AsiaPacific region: A Lancet Gastroenterology & Hepatology Commission. Lancet Gastroenterol. Hepatol. 2020, 5, 167–228. [Google Scholar] [PubMed]
- Wiegand, S.; Keller, K.M.; Roebl, M.; Reinehr, T.; Widhalm, K.; Holl, R.W. Obese boys at increased risk for nonalcoholic liver disease: Evaluation of 16 390 overweight or obese children and adolescents. Int. J. Obes. 2010, 34, 1468–1474. [Google Scholar] [CrossRef]
- Welsh, J.A.; Karpen, S.; Vos, M.B. Increasing prevalence of nonalcoholic fatty liver disease among United States adolescents, 1988–1994 to 2007–2010. J. Pediatr. 2013, 162, 496–500. [Google Scholar] [CrossRef]
- Rorat, M.; Jurek, T.; Kuchar, E.; Szenborn, L.; Golema, W.; Halon, A. Liver steatosis in Polish children assessed by medicolegal autopsies. World J. Pediatr. 2013, 9, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Ciardullo, S.; Monti, T.; Perseghin, G. Prevalence of liver steatosis and fibrosis detected by transient elastography in adolescents in the 2017–2018 National Health and Nutrition Examination Survey. Clin. Gastroenterol. Hepatol. 2021, 19, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Mărginean, C.O.; Meliţ, L.E.; Ghiga, D.V.; Săsăran, M.O. The assessment of liver fibrosis in children with obesity on two methods: Transient and two dimensional shear wave elastography. Sci. Rep. 2019, 9, 19800. [Google Scholar] [CrossRef] [PubMed]
- Goyal, N.P.; Schwimmer, J.B. The progression and natural history of pediatric nonalcoholic fatty liver disease. Clin. Liver Dis. 2016, 20, 325–338. [Google Scholar] [CrossRef]
- Feldstein, A.E.; Charatcharoenwitthaya, P.; Treeprasertsuk, S.; Benson, J.T.; Enders, F.B.; Angulo, P. The natural history of nonalcoholic fatty liver disease in children: A follow-up study for up to 20 years. Gut 2009, 58, 1538–1544. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, W.L.; Elizabeth, L.Y.; Arin, J.C.; Murray, K.F.; Ali, S.; Desai, N.K.; Xanthakos, S.A.; Lin, H.C.; Alkhouri, N.; Abdou, R.; et al. Clinical practice approach to nonalcoholic fatty liver disease by pediatric gastroenterologists in the United States. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Berentzen, T.L.; Gamborg, M.; Holst, C.; Sørensen, T.I.; Baker, J.L. Body mass index in childhood and adult risk of primary liver cancer. J. Hepatol. 2014, 60, 325–330. [Google Scholar] [CrossRef]
- Xanthakos, S.A.; Lavine, J.E.; Yates, K.P.; Schwimmer, J.B.; Molleston, J.P.; Rosenthal, P.; Murray, K.F.; Vos, M.B.; Jain, A.K.; Scheimann, A.O.; et al. Progression of fatty liver disease in children receiving standard of care lifestyle advice. Gastroenterology 2020, 159, 1731–1751. [Google Scholar] [CrossRef]
- Alkhouri, N.; Hanouneh, I.A.; Zein, N.N.; Lopez, R.; Kelly, D.; Eghtesad, B.; Fung, J.J. Liver transplantation for nonalcoholic steatohepatitis in young patients. Transpl. Int. 2016, 29, 418–424. [Google Scholar] [CrossRef]
- Hecht, L.; Weiss, R. Nonalcoholic fatty liver disease and type 2 diabetes in obese children. Curr. Diab Rep. 2014, 14, 448. [Google Scholar] [CrossRef] [PubMed]
- Pearce, N.; Aït-Khaled, N.; Beasley, R.; Mallol, J.; Keil, U.; Mitchell, E.; Robertson, C. ISAAC Phase Three Study Group Worldwide trends in the prevalence of asthma symptoms: Phase III of the international study of asthma and allergies in childhood (ISAAC). Thorax 2007, 62, 757–765. [Google Scholar] [CrossRef]
- Liu, P.-C.; Kieckhefer, G.M.; Gau, B.-S. A systematic review of the association between obesity and asthma in children. J. Adv. Nurs. 2013, 69, 1446–1465. [Google Scholar] [CrossRef]
- Ali, Z.; Ulrik, C.S. Obesity and asthma: A coincidence or a causal relationship? A systematic review. Respir. Med. 2013, 107, 1287–1300. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, Z.; Berhane, K.; Urman, R.; Chatzi, V.L.; Breton, C.; Gilliland, F.D. The dynamic relationship between asthma and obesity in school children. Am. J. Epidemiol. 2020, 189, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Egan, K.B.; Ettinger, A.S.; Bracken, M.B. Childhood body mass index and subsequent physician-diagnosed asthma: A systematic review and meta-analysis of prospective cohort studies. BMC Pediatr. 2013, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Contreras, Z.A.; Chen, Z.; Roumeliotaki, T.; Annesi-Maesano, I.; Baïz, N.; von Berg, A.; Bergström, A.; Crozier, S.; Duijts, L.; Ekström, S.; et al. Does early onset asthma increase childhood obesity risk? A pooled analysis of 16 European cohorts. Eur. Respir. J. 2018, 52, 3–11. [Google Scholar] [CrossRef]
- De Jesus, J.P.V.; Lima-Matos, A.S.; Almeida, P.C.A.; Lima, V.B.; de Mello, L.M.; Souza-Machado, A.; Ponte, E.V.; Cruz, Á.A. Obesity and asthma: Clinical and laboratory characterization of a common combination. J. Bras. Pneumol. 2018, 44, 207–212. [Google Scholar] [CrossRef]
- Sansone, F.; Attanasi, M.; Di Pillo, S.; Chiarelli, F. Asthma and obesity in children. Biomedicines 2020, 8, 231. [Google Scholar] [CrossRef]
- Lang, J.E.; Bunnell, H.T.; Lima, J.J.; Hossain, M.J.; Wysocki, T.; Bacharier, L.; Dempsey, A.; Ulrich, L.; Test, M.R.; Forrest, C.B. Effects of age, sex, race/ethnicity, and allergy status in obesity-related pediatric asthma. Pediatr. Pulmonol. 2019, 54, 1684–1693. [Google Scholar] [CrossRef]
- Chen, Z.; Salam, M.T.; Alderete, T.L.; Habre, R.; Bastain, T.M.; Berhane, K.; Gilliland, F.D. Effects of childhood asthma on the development of obesity among school-aged children. Am. J. Respir. Crit. Care Med. 2017, 195, 1181–1188. [Google Scholar] [CrossRef] [PubMed]
- McClean, K.M.; Kee, F.; Young, I.S.; Elborn, J.S. Obesity and the Lung: Epidemiology. Thorax 2008, 63, 649–654. [Google Scholar] [CrossRef]
- Holguin, F.; Fitzpatrick, A. Obesity, Asthma, and Oxidative Stress. J. Appl. Physiol. 2010, 108, 754–759. [Google Scholar] [CrossRef]
- Bastard, J.; Maachi, M.; Lagathu, C.; Kim, M.; Caron, M.; Vidal, H.; Capeau, J.; Feve, B. Recent Advances in the Relationshipbetween Obesity, Inflammation, and Insulin Resistance. Eur. Cytokine Netw. 2006, 17, 4–12. [Google Scholar]
- Michelson, P.H.; Williams, L.W.; Benjamin, D.K.; Barnato, A.E. Obesity, Inflammation, and Asthma Severity in Childhood: Data from the National Health and Nutrition Examination Survey 2001–2004. Ann. Allergy Asthma Immunol. 2009, 103, 381–385. [Google Scholar] [CrossRef]
- Chen, Y.; Rennie, D.; Cormier, Y.F.; Dosman, J. Waist circumference is associated with pulmonary function in normal-weight, overweight, and obese subjects. Am. J. Clin. Nutr. 2007, 85, 35–92. [Google Scholar] [CrossRef]
- Dixon, A.E.; Poynter, M.E. Mechanisms of asthma in obesity pleiotropic aspects of obesity produce distinct asthma phenotypes. Am. J. Respir. Cell Mol. Biol. 2016, 54, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Kuruvilla, M.E.; Lee, F.E.H.; Lee, G.B. Understanding asthma phenotypes, endotypes, and mechanisms of disease. Clin. Rev. Allergy Immunol. 2019, 56, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Sood, A.; Shore, S.A. Adiponectin, leptin, and resistin in asthma: Basic mechanisms through population studies. J. Allergy 2013, 2013, 785835. [Google Scholar] [CrossRef]
- Chambers, E.S.; Nanzer, A.M.; Pfeffer, P.E.; Richards, D.F.; Timms, P.M.; Martineau, A.R.; Griffiths, C.J.; Corrigan, C.J.; Hawrylowicz, C.M. Distinct endotypes of steroid-resistant asthma characterized by IL-17A high and IFN-γ high immunophenotypes: Potential benefits of calcitriol. J. Allergy Clin. Immunol. 2015, 136, 628–637. [Google Scholar] [CrossRef] [PubMed]
- Oda, N.; Canelos, P.B.; Essayan, D.M.; Plunkett, B.A.; Myers, A.C.; Huang, S.-K. Interleukin-17F induces pulmonary neutrophilia and amplifies antigen-induced allergic response. Am. J. Respir. Crit. Care Med. 2005, 171, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Udo, M.; Melton, A.C.; Chen, C.; Engler, M.B.; Huang, K.E.; Ren, X.; Wang, Y.; Bernstein, X.; Li, J.T.; Atabai, K.; et al. IL-17A produced by αβ T cells drives airway hyper-responsiveness in mice and enhances mouse and human airway smooth muscle contraction. Nat. Med. 2012, 18, 547–554. [Google Scholar]
- Machado, M.E.; Porto, L.C.; Alves Galvão, M.G.; Sant’Anna, C.C.; Lapa, E.; Silva, J.R. SNPs, adipokynes and adiposity in children with asthma. J. Asthma 2023, 60, 446–457. [Google Scholar] [CrossRef]
- Mohanan, S.; Tapp, H.; McWilliams, A.; Dulin, M. Obesity and asthma: Pathophysiology and implications for diagnosis and management in primary care. Exp. Biol. Med. 2014, 239, 1531–1540. [Google Scholar] [CrossRef]
- Afshar-Mohajer, N.; Wu, T.D.; Shade, R.; Brigham, E.; Woo, H.; Wood, M.; Koehl, R.; Koehler, K.; Kirkness, J.; Hansel, N.N.; et al. Obesity, tidal volume, and pulmonary deposition of fine particulate matter in children with asthma. Eur. Respir. J. 2021, 59, 2100209. [Google Scholar] [CrossRef] [PubMed]
- Willeboordse, M.; Van DeKant, K.D.G.; Tan, F.E.S.; Mulkens, S.; Schellings, J.; Crijns, Y.; van der Ploeg, L.; van Schayck, C.P.; Dompeling, E.A. Multifactorial Weight Reduction Programme for Children with Overweight and Asthma: A Randomized Controlled Trial. PLoS ONE 2016, 11, e0157158. [Google Scholar] [CrossRef] [PubMed]
- Scott, H.A.; Gibson, P.G.; Garg, M.L.; Pretto, J.J.; Morgan, P.J.; Callister, R.; Wood, L.G. Dietary restriction and exercise improve airway inflammation and clinical outcomes in overweight and obese asthma: A randomized trial. Clin. Exp. Allergy 2013, 43, 36–49. [Google Scholar] [CrossRef]
- Pradeepan, S.; Garrison, G.; Dixon, A.E. Obesity in asthma: Approaches to treatment. Curr. Allergy Asthma Rep. 2013, 13, 434–442. [Google Scholar] [CrossRef]
- Engelkes, M.; Baan, E.J.; de Ridder, M.A.J.; Svensson, E.; Prieto-Alhambra, D.; Lapi, F.; Giaquinto, C.; Picelli, G.; Boudiaf, N.; Albers, F.; et al. Incidence, risk factors and re-exacerbation rate of severe asthma exacerbations in a multinational, multidatabase pediatric cohort study. Pediatr. Allergy Immunol. 2020, 31, 496–505. [Google Scholar] [CrossRef]
- Resta, O.; Foschino-Barbaro, M.P.; Legari, G.; Talamo, S.; Bonfitto, P.; Palumbo, A.; Minenna, A.; Giorgino, R.; De Pergola, G. Sleep-related breathing disorders, loud snoring and excessive daytime sleepiness in obese subjects. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 669–675. [Google Scholar] [CrossRef]
- Haas, D.C.; Foster, G.L.; Nieto, F.J.; Redline, S.; Resnick, H.E.; Robbins, J.A.; Young, T.; Pickering, T.G. Age-dependent associations between sleep-disordered breathing and hypertension. Circulation 2005, 111, 614–621. [Google Scholar] [CrossRef]
- Conrad, L.A.; Nandalike, K.; Rani, S.; Rastogi, D. Associations between sleep, obesity, and asthma in urban minority children. J. Clin. Sleep Med. 2022, 18, 2377–2385. [Google Scholar] [CrossRef]
- French, S.A.; Story, M.; Perry, C.L. Self-Esteem and Obesity in Children and Adolescents: A Literature Review. Obes. Res. 1995, 3, 479–490. [Google Scholar] [CrossRef]
- Griffiths, L.J.; Parsons, T.J.; Hill, A.J. Self-esteem and quality of life in obese children and adolescents: A systematic review. Int. J. Pediatr. Obes. IJPO An. Off. J. Int. Assoc. Study Obes. 2010, 5, 282–304. [Google Scholar] [CrossRef]
- Anagnostis, P.; Tarlatzis, B.C.; Kauffman, R.P. Polycystic ovarian syndrome (PCOS): Long-term metabolic consequences. Metab. Clin. Exp. 2018, 86, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Elizondo-Montemayor, L.; Hernández-Escobar, C.; Lara-Torre, E.; Nieblas, B.; Gómez-Carmona, M. Gynecologic and Obstetric Consequences of Obesity in Adolescent Girls. J. Pediatr. Adolesc. Gynecol. 2017, 30, 156–168. [Google Scholar] [CrossRef] [PubMed]
- Hillman, J.B.; Miller, R.J.; Inge, T.H. Menstrual Concerns and Intrauterine Contraception Among Adolescent Bariatric Surgery Patients. J. Women’s Health 2011, 20, 533. [Google Scholar] [CrossRef] [PubMed]
- Itriyeva, K. The effects of obesity on the menstrual cycle. Curr. Probl. Pediatr. Adolesc. Health Care 2022, 52, 101241. [Google Scholar] [CrossRef]
- Frisch, R.E.; Revelle, R. Height and Weight at Menarche and a Hypothesis of Critical Body Weights and Adolescent Events. Science 1970, 169, 397–399. [Google Scholar] [CrossRef]
- Brix, N.; Ernst, A.; Lauridsen, L.L.B.; Parner, E.T.; Arah, O.A.; Olsen, J.; Henriksen, T.B.; Ramlau-Hansen, C.H. Childhood overweight and obesity and timing of puberty in boys and girls: Cohort and sibling-matched analyses. Int. J. Epidemiol. 2020, 49, 834–844. [Google Scholar] [CrossRef]
- Pita, J.; Barrios, V.; Gavela-Pérez, T.; Martos-Moreno, G.Á.; Muñoz-Calvo, M.T.; Pozo, J.; Rovira, A.; Argente, J.; Soriano-Guillén, L. Circulating kisspeptin levels exhibit sexual dimorphism in adults, are increased in obese prepubertal girls and do not suffer modifications in girls with idiopathic central precocious puberty. Peptides 2011, 32, 1781–1786. [Google Scholar] [CrossRef]
- Legro, R.S.; Arslanian, S.A.; Ehrmann, D.A.; Hoeger, K.M.; Murad, M.H.; Pasquali, R.; Welt, C.K. Diagnosis and treatment of polycystic ovary syndrome: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2013, 98, 4565–4592. [Google Scholar] [CrossRef]
- Triggle, C.R.; Mohammed, I.; Bshesh, K.; Marei, I.; Ye, K.; Ding, H.; MacDonald, R.; Hollenberg, M.D.; Hill, M.A. Metformin: Is it a drug for all reasons and diseases? Metabolism 2022, 133, 155223. [Google Scholar] [CrossRef] [PubMed]
- Kousta, E. Premature adrenarche leads to polycystic ovary syndrome? Long-term consequences. Ann. N. Y. Acad. Sci. 2006, 1092, 148–157. [Google Scholar] [CrossRef]
- Peña, A.S.; Witchel, S.F.; Hoeger, K.M.; Oberfield, S.E.; Vogiatzi, M.G.; Misso, M.; Garad, R.; Dabadghao, P.; Teede, H. Adolescent polycystic ovary syndrome according to the international evidence-based guideline. BMC Med. 2020, 18, 72. [Google Scholar] [CrossRef]
- Ibáñez, L.; Oberfield, S.E.; Witchel, S.; Auchus, R.J.; Chang, R.J.; Codner, E.; Dabadghao, P.; Darendeliler, F.; Elbarbary, N.S.; Gambineri, A.; et al. An International Consortium Update: Pathophysiology, Diagnosis, and Treatment of Polycystic Ovarian Syndrome in Adolescence. Horm. Res. Paediatr. 2017, 88, 371–395. [Google Scholar] [CrossRef] [PubMed]
- Teede, H.J.; Misso, M.L.; Costello, M.F.; Dokras, A.; Laven, J.; Moran, L.; Piltonen, T.; Norman, R.J.; Andersen, M.; Azziz, R.; et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil. Steril. 2018, 110, 364–379. [Google Scholar] [CrossRef] [PubMed]
- Nordt, C.A.; DiVasta, A.D. Gynecomastia in adolescents. Curr. Opin. Pediatr. 2008, 20, 375–382. [Google Scholar] [CrossRef]
- Teede, H.J.; Tay, C.T.; Laven, J.J.E.; Dokras, A.; Moran, L.J.; Piltonen, T.T.; Costello, M.F.; Boivin, J.; Redman, L.M.; Boyle, J.A.; et al. Recommendations from the 2023 International Evidence-based Guideline for the Assessment and Management of Polycystic Ovary Syndrome. J. Clin. Endocrinol. Metab. 2023, 108, 2447–2469. [Google Scholar] [CrossRef]
- Lemaine, V.; Cayci, C.; Simmons, P.S.; Petty, P. Gynecomastia in adolescent males. Semin. Plast. Surg. 2013, 27, 56–61. [Google Scholar] [CrossRef]
- Soliman, A.T.; De Sanctis, V.; Yassin, M. Management of adolescent gynecomastia: An update. Acta Biomed. 2017, 88, 204–213. [Google Scholar] [PubMed]
- Sansone, A.; Romanelli, F.; Sansone, M.; Lenzi, A.; Di Luigi, L. Gynecomastia and hormones. Endocrine 2017, 55, 37–44. [Google Scholar] [CrossRef] [PubMed]
- De Sanctis, V.; Soliman, A.T.; Tzoulis, P.; Daar, S.; Di Maio, S.; Kattamis, C. Unilateral breast enlargement in males during adolescence (10–19 years): Review of current literature and personal experience. Acta Biomed. 2023, 94, e2023004. [Google Scholar] [CrossRef]
- Reinehr, T.; Kulle, A.; Barth, A.; Ackermann, J.; Lass, N.; Holterhus, P.M. Sex Hormone Profile in Pubertal Boys With Gynecomastia and Pseudogynecomastia. J. Clin. Endocrinol. Metab. 2020, 105, dgaa044. [Google Scholar] [CrossRef]
- Jones, K.N. Imaging of the adolescent breast. Semin. Plast. Surg. 2013, 27, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Hellmann, P.; Christiansen, P.; Johannsen, T.H.; Main, K.M.; Duno, M.; Juul, A. Male patients with partial androgen insensitivity syndrome: A longitudinal follow-up of growth, reproductive hormones and the development of gynaecomastia. Arch. Dis. Child. 2012, 97, 403–409. [Google Scholar] [CrossRef]
- Ankarberg-Lindgren, C.; Norjavaara, E. Twenty-four hours secretion pattern of serum estradiol in healthy prepubertal and pubertal boys as determined by a validated ultra-sensitive extraction RIA. BMC Endocr. Disord. 2008, 8, 10. [Google Scholar] [CrossRef]
- Lee, P.A. The relationship of concentrations of serum hormones to pubertal gynecomastia. J. Pediatr. 1975, 86, 212–215. [Google Scholar] [CrossRef]
- Zuckerman-Levin, N.; Hochberg, Z.; Rosenfeld, R.L. Gynecomastia. In Practical Algorithms in Pediatric Endocrinology; Hochberg, Z., Ed.; Karger: Basel, Switzerland, 2007; pp. 20–21. [Google Scholar]
- Godwin, Y. Gynaecomastia: Considerations and challenges in treating male patients with varying body habitus. Eur. J. Plast. Surg. 2012, 35, 55–64. [Google Scholar] [CrossRef]
- Rohrich, R.J.; Ha, R.Y.; Kenkel, J.M.; Adams, W.P. Classification and management of gynecomastia: Defining the role of ultrasound assisted liposuction. Plast. Reconstr. Surg. 2003, 11, 909–923. [Google Scholar] [CrossRef]
- Cordova, A.; Moschella, F. Algorithm for clinical evaluation and surgical treatment of gynecomastia. J. Plast. Reconstr. Aesthet. Surg. 2008, 61, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.C.; Schlaepfer, L.P.; Sizonenko, P.C. Hormonal changes during puberty: Transient pubertal gynecomastia; abnormal androgen-estrogens ratios. J. Clin. Endocrinol. Metab. 1984, 58, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Shozu, M.; Fukami, M.; Ogata, T. Understanding the pathological manifestations of aromatase excess syndrome: Lessons for clinical diagnosis. Expert. Rev. Endocrinol. Metab. 2014, 9, 397–409. [Google Scholar] [CrossRef] [PubMed]
- Biro, F.M.; Lucky, A.W.; Huster, G.A.; Morrison, J.A. Hormonal studies and physical maturation in adolescent gynecomastia. J. Pediatr. 1990, 116, 450–455. [Google Scholar] [CrossRef]
- Mieritz, M.G.; Sorensen, K.; Aksglaede, L.; Mouritsen, A.; Hagen, C.P.; Hilsted, L.; Andersson, A.M.; Juul, A. Elevated serum IGF-I, but unaltered sex steroid levels, in healthy boys with pubertal gynaecomastia. Clin. Endocrinol. 2014, 80, 691–698. [Google Scholar] [CrossRef]
- Aluclu, M.A.; Sen, S.; Cevik, M. Association between plasma kisspeptin levels and adolescent gynecomastia. Afr. J. Paediatr. Surg. 2016, 13, 136–139. [Google Scholar] [PubMed]
- Kilic, M.; Kanbur, N.; Derman, O.; Akgül, S.; Kutluk, T. The relationship between pubertal gynecomastia, prostate specific antigen, free androgen index, SHBG and sex steroids. J. Pediatr. Endocrinol. Metab. 2011, 24, 61–67. [Google Scholar] [CrossRef]
- Devalia, H.L.; Layer, G.T. Current concepts in gynecomastia. J. R. Coll. Surg. Edinb. 2009, 7, 114–119. [Google Scholar]
- Limony, Y.; Friger, M.; Hochberg, Z. Pubertal gynecomastia coincides with peak height velocity. J. Clin. Res. Pediatr. Endocrinol. 2013, 5, 142–144. [Google Scholar] [CrossRef]
- Dickson, G. Gynecomastia. Am. Fam. Physician 2012, 85, 716–722. [Google Scholar]
- Marcus, C.; Danielsson, P.; Hagman, E. Pediatric obesity—Long-term consequences and effect of weight loss. J. Intern. Med. 2022, 292, 870–891. [Google Scholar] [CrossRef] [PubMed]
- Nicolis, G.L.; Modlinger, R.S.; Gabrilove, J.L. A study of the histopathology of human gynecomastia. J. Clin. Endocrinol. Metab. 1971, 32, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Fricke, A.; Lehner, G.M.; Stark, G.B.; Penna, V. Gynecomastia: Histological appearance in different age groups. J. Plast. Surg. Hand Surg. 2018, 52, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Szumlas, Z.; Jurek, A.; Mrozek, Ł.; Klocek, K.; Zwolski, M.; Puchalski, K.; Kostecki, B.; Hajduk, A. Gynecomastia—A literature review of management, diagnosis and treatment. J. Educ. Health Sport 2023, 35, 147–159. [Google Scholar] [CrossRef]
- Kasielska, A.; Antoszewski, B. Effect of operative treatment on psychosocial problems of men with gynaecomastia. Pol. Przegl. Chir. 2011, 83, 614–621. [Google Scholar] [CrossRef]
- Laituri, C.A.; Garey, C.L.; Ostlie, D.J.; St Peter, S.D.; Gittes, G.K.; Snyder, C.L. Treatment of adolescent gynecomastia. J. Pediatr. Surg. 2010, 45, 650–654. [Google Scholar] [CrossRef]
- De Leonibus, C.; Marcovecchio, M.L.; Chiavaroli, V.; de Giorgis, T.; Chiarelli, F.; Mohn, A. Timing of puberty and physical growth in obese children: A longitudinal study in boys and girls. Pediatr. Obes. 2014, 9, 292–299. [Google Scholar] [CrossRef]
- Laaksonen, D.E.; Niskanen, L.; Punnonen, K.; Nyyssönen, K.; Tuomainen, T.-P.; Valkonen, V.-P.; Salonen, R.; Salonen, J.T. Testosterone and sex hormone-binding globulin predict the metabolic syndrome and diabetes in middle-aged men. Diabetes Care 2004, 27, 1036–1041. [Google Scholar] [CrossRef]
- Stancampiano, M.R.; Lucas-Herald, A.K.; Russo, G.; Rogol, A.D.; Ahmed, S.F. Testosterone Therapy in Adolescent Boys: The Need for a Structured Approach. Horm. Res. Paediatr. 2020, 92, 215–228. [Google Scholar] [CrossRef]
- Grossmann, M.; Matsumoto, A.M. A perspective on middle-aged and older men with functional hypogonadism: Focus on holistic management. J. Clin. Endocrinol. Metab. 2017, 102, 1067–1075. [Google Scholar] [CrossRef]
- Palmert, M.R.; Dunkel, L. Clinical practice. Delayed puberty. N. Engl. J. Med. 2012, 366, 443–453. [Google Scholar] [CrossRef]
- Sedlmeyer, I.L.; Palmert, M.R. Hospital CNS. Delayed puberty: Analysis of a large case series from an academic center. J. Clin. Endocrinol. Metab. 2002, 87, 1613–1620. [Google Scholar] [CrossRef]
- Elliott, V.; Waldrop, S.W.; Wiromrat, P.; Carreau, A.M.; Green, M.C. The Interaction of Obesity and Reproductive Function in Adolescents. Semin. Reprod. Med. 2022, 40, 53–68. [Google Scholar] [CrossRef] [PubMed]
- Grumbach, M.M. The neuroendocrinology of human puberty revisited. Horm. Res. 2002, 57, 2–14. [Google Scholar] [CrossRef] [PubMed]
- Dwyer, A.A.; Phan-Hug, F.; Hauschild, M.; Elowe-Gruau, E.; Pitteloud, N. Hypogonadism in adolescence. Eur. J. Endocrinol. 2015, 173, R15–R24. [Google Scholar] [CrossRef] [PubMed]
- Roa, J.; Herbison, A.E. Direct regulation of GnRH neuron excitability by arcuate nucleus POMC and NPY neuron neuropeptides in female mice. Endocrinology 2012, 153, 5587–5599. [Google Scholar] [CrossRef]
- Vollbach, H.; Brandt, S.; Lahr, G.; Denzer, C.; von Schnurbein, J.; Debatin, K.M.; Wabitsch, M. Prevalence and phenotypic characterization of MC4R variants in a large pediatric cohort. Int. J. Obes. 2017, 41, 13–22. [Google Scholar] [CrossRef]
- Han, J.C.; Lawlor, D.A.; Kimm, S.Y. Childhood obesity. Lancet 2010, 375, 1737–1748. [Google Scholar] [CrossRef] [PubMed]
- Bell, C.G.; Walley, A.J.; Froguel, P. The genetics of human obesity. Nat. Rev. Genet. 2005, 6, 221–234. [Google Scholar] [CrossRef]
- Di Cesare, M.; Sorić, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.P.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 212. [Google Scholar] [CrossRef]
- Rak, A.; Mellouk, N.; Froment, P.; Dupont, J. Adiponectin and resistin: Potential metabolic signals affecting hypothalamo-pituitary gonadal axis in females and males of different species. Reproduction 2017, 153, R215–R226. [Google Scholar] [CrossRef] [PubMed]
- Elias, C.F. Leptin action in pubertal development: Recent advances and unanswered questions. Trends Endocrinol. Metab. 2012, 23, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Vazquez, M.J.; Velasco, I.; Tena-Sempere, M. Novel mechanisms for the metabolic control of puberty: Implications for pubertal alterations in early-onset obesity and malnutrition. J. Endocrinol. 2019, 242, R51–R65. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.W.; Elias, C.F. Neuroanatomical framework of the metabolic control of reproduction. Physiol. Rev. 2018, 98, 2349–2380. [Google Scholar] [CrossRef]
- Manfredi-Lozano, M.; Roa, J.; Ruiz-Pino, F.; Piet, R.; Garcia-Galiano, D.; Pineda, R.; Zamora, A.; Leon, S.; Sanchez-Garrido, M.A.; Romero-Ruiz, A.; et al. Defining a novel leptin-melanocortin-kisspeptin pathway involved in the metabolic control of puberty. Mol. Metab. 2016, 5, 844–857. [Google Scholar] [CrossRef] [PubMed]
- Reinehr, T.; Roth, C.L. Is there a causal relationship between obesity and puberty? Lancet Child Adolesc. Health 2019, 3, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Pinhas-Hamiel, O.; Singer, S.; Pilpel, N.; Koren, I.; Boyko, V.; Hemi, R.; Pariente, C.; Kanety, H. Adiponectin levels in adolescent girls with polycystic ovary syndrome (PCOS). Clin. Endocrinol. 2009, 71, 823–827. [Google Scholar] [CrossRef]
- Pereira, A.; Busch, A.S.; Solares, F.; Baier, I.; Corvalan, C.; Mericq, V. Total and central adiposity are associated with age at gonadarche and incidence of precocious gonadarche in boys. J. Clin. Endocrinol. Metab. 2021, 106, 1352–1361. [Google Scholar] [CrossRef]
- Juul, A.; Magnusdottir, S.; Scheike, T.; Prytz, S.; Skakkebaek, N.E. Age at voice break in Danish boys: Effects of pre-pubertal body mass index and secular trend. Int. J. Androl. 2007, 30, 537–542. [Google Scholar] [CrossRef]
- Monteilh, C.; Kieszak, S.; Flanders, W.D.; Maisonet, M.; Rubin, C.; Holmes, A.K.; Heron, J.; Golding, J.; McGeehin, M.A.; Marcus, M. Timing of maturation and predictors of Tanner stage transitions in boys enrolled in a contemporary British cohort. Paediatr. Perinat. Epidemiol. 2011, 25, 75–87. [Google Scholar] [CrossRef]
- Ong, K.K.; Bann, D.; Wills, A.K.; Ward, K.; Adams, J.E.; Hardy, R.; Kuh, D.; National Survey of Health and Development Scientific and Data Collection Team. Timing of voice breaking in males associated with growth and weight gain across the life course. J. Clin. Endocrinol. Metab. 2012, 97, 2844–2852. [Google Scholar] [CrossRef]
- Sopher, A.B.; Jean, A.M.; Zwany, S.K.; Winston, D.M.; Pomeranz, C.B.; Bell, J.J.; McMahon, D.J.; Hassoun, A.; Fennoy, I.; Oberfield, S.E. Bone age advancement in prepubertal children with obesity and premature adrenarche: Possible potentiating factors. Obesity 2011, 19, 1259–1264. [Google Scholar] [CrossRef] [PubMed]
- Dhindsa, S.; Ghanim, H.; Batra, M.; Dandona, P. Hypogonadotropic hypogonadism in men with diabesity. Diabetes Care 2018, 41, 1516–1525. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.; Nassau, D.E.; Patel, P.; Ramasamy, R. Low testosterone in adolescents & young adults. Front. Endocrinol. 2020, 10, 916. [Google Scholar]
- Vignolo, M.; Naselli, A.; Di Battista, E.; Mostert, M.; Aicardi, G. Growth and development in simple obesity. Eur. J. Pediatr. 1988, 147, 242–244. [Google Scholar] [CrossRef] [PubMed]
- Denzer, C.; Weibel, A.; Muche, R.; Karges, B.; Sorgo, W.; Wabitsch, M. Pubertal development in obese children and adolescents. Int. J. Obes. 2007, 31, 1509–1519. [Google Scholar] [CrossRef] [PubMed]
- Rosenfield, R.L.; Bordini, B. Evidence that obesity and androgens have independent and opposing effects on gonadotropin production from puberty to maturity. Brain Res. 2010, 1364, 186–197. [Google Scholar] [CrossRef]
- Fernandez, C.J.; Chacko, E.C.; Pappachan, J.M. Male obesity related secondary hypogonadism–pathophysiology, clinical implications and management. Eur. Endocrinol. 2019, 15, 83–90. [Google Scholar] [CrossRef]
- Nokoff, N.; Thurston, J.; Hilkin, A.; Pyle, L.; Zeitler, P.S.; Nadeau, K.J.; Santoro, N.; Kelsey, M.M. Sex Differences in Effects of Obesity on Reproductive Hormones and Glucose Metabolism in Early Puberty. J. Clin. Endocrinol. Metab. 2019, 104, 4390–4397. [Google Scholar] [CrossRef]
- Silvestris, E.; de Pergola, G.; Rosania, R.; Loverro, G. Obesity as disruptor of the female fertility. Reprod. Biol. Endocrinol. 2018, 16, 22. [Google Scholar] [CrossRef]
- Sarchielli, E.; Comeglio, P.; Squecco, R.; Ballerini, L.; Mello, T.; Guarnieri, G.; Idrizaj, E.; Mazzanti, B.; Vignozzi, L.; Gallina, P.; et al. Tumor Necrosis Factor-α Impairs Kisspeptin Signaling in Human Gonadotropin-Releasing Hormone Primary Neurons. J. Clin. Endocrinol. Metab. 2017, 102, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Morelli, A.; Sarchielli, E.; Comeglio, P.; Filippi, S.; Vignozzi, L.; Marini, M.; Rastrelli, G.; Maneschi, E.; Cellai, I.; Persani, L.; et al. Metabolic syndrome induces inflammation and impairs gonadotropin-releasing hormone neurons in the preoptic area of the hypothalamus in rabbits. Mol. Cell. Endocrinol. 2014, 382, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Corona, G.; Goulis, D.G.; Huhtaniemi, I.; Zitzmann, M.; Toppari, J.; Forti, G.; Vanderschueren, D.; Wu, F.C. European Academy of Andrology (EAA) guidelines on investigation, treatment and monitoring of functional hypogonadism in males: Endorsing organization: European Society of Endocrinology. Andrology 2020, 8, 970–987. [Google Scholar] [CrossRef]
- Corona, G.; Rastrelli, G.; Monami, M.; Saad, F.; Luconi, M.; Lucchese, M.; Facchiano, E.; Sforza, A.; Forti, G.; Manucci, E.; et al. Body weight loss reverts obesity-associated hypogonadotropic hypogonadism: A systematic review and meta-analysis. Eur. J. Endocrinol. 2013, 168, 829–843. [Google Scholar] [CrossRef]
- Clark, A.M.; Ledger, W.; Galletly, C.; Tomlinson, L.; Blaney, F.; Wang, X.; Norman, R.J. Weight loss results in significant improvement in pregnancy and ovulation rates in anovulatory obese women. Hum. Reprod. 1995, 10, 2705–2712. [Google Scholar] [CrossRef] [PubMed]

