1. Introduction
Wound healing is a complex process that repairs damaged tissues, with acute wounds healing predictably, while chronic wounds require specialized and prolonged treatment [1]. While traditional dressings offer some protection, modern dressings actively promote optimal healing for complex wounds, revolutionizing the wound care [1,2]. The hydrogel market is anticipated to experience a growth rate of 6.5%, reaching USD 22.8 billion by 2032, driven by increased demand for advanced wound-healing products due to factors like an aging population and a rise in chronic wounds. Hydrogels, known for moisture retention and easy application, are increasingly preferred in advanced wound care. The market is segmented by raw material (synthetic, natural, hybrid), with synthetic holding 53.4% market share in 2022. Key players include 3M, Johnson & Johnson, Cardinal Health, Cooper Vision, and Smith & Nephew [3,4]. Hydrogels’ distinct properties render them ideal for wound care, promoting wound protection, cell migration, proliferation, and tissue regeneration. Hydrogel membranes can be customized for various wound types, sizes, and depths, benefiting both clinicians and patients. One of the key advantages of hydrogels lies in their ability to incorporate and release a wide range of bioactive compounds, ensuring their optimal delivery at the wound site. These compounds can include growth factors [5], antimicrobial agents [6,7], anti-inflammatory drugs [8], plant extracts [9], and even stem cells [10]. Notably, hydrogel membranes with bioactive compounds like collagen and hyaluronic acid hold promise for wound healing as they stimulate cell growth, angiogenesis, and tissue regeneration, mimicking the natural extracellular matrix [11].
Doxycycline (DOXY), a member of the tetracycline class of antibiotics, exhibits broad-spectrum activity against both Gram-positive and Gram-negative bacteria by disrupting bacterial protein synthesis through binding to the bacterial ribosome [12]. Although DOXY has antimicrobial activity, the literature findings have highlighted several other biological effects independent of this action. Tetracyclines are believed to possess anti-inflammatory, immunomodulatory, and antioxidant properties, influencing cell proliferation and migration [13,14]. Among these non-antimicrobial effects, the inhibition of MMP is particularly representative of DOXY’s action. The use of DOXY as a MMP inhibitor via topical administration has been reported at doses ranging from 200 to 375 μg [15]. Researchers are exploring the biological effects of tetracyclines that can be achieved at lower, subantimicrobial doses (20–50 mg) compared to the usual antimicrobial dose (100–300 mg) and also reported that topical application of doses up to 10,000 mg/mL did not cause adverse reactions while maintaining the biological effects [16,17,18]. Modulating protease activity is crucial for addressing conditions with increased inflammation and excessive proteolytic activity, like chronic wounds. In chronic wounds, as in other chronic inflammatory conditions, the elevated levels of pro-inflammatory cytokines (such as tumor necrosis factor [TNF-α] and interleukin [IL-1β]) and matrix metalloproteinases (MMPs) impede the natural healing process. Both animal models and clinical research on ulcerative diseases have indicated that DOXY, an affordable and FDA-approved antibiotic, shows promise in inhibiting MMPs and TNF-α-converting enzyme (TACE), which belongs to the MMP superfamily [19].
In recent years, researchers have been actively exploring alternatives to traditional antibiotic treatments, and one promising option is the use of metallic nanoparticles, such as silver, gold, copper, or titanium nanoparticles [20,21]. The antibacterial properties of silver nanoparticles (npAg) are attributed to the disruptions of the bacterial cell wall (through electrostatic effects and accumulation between lipid layers), the generation of reactive oxygen species (ROS) due to nanoparticle internalization, and the release of positive ions [22,23]. The bactericidal effect is dependent on the size of the nanoparticles (e.g., nanoparticles below 30 nm exhibit increased efficiency in generating ROS) or their shape (e.g., triangular shape more efficient against E. coli) [24,25,26,27]. The npAg can be utilized in biomedical material mixtures in low concentrations due to their specific high surface area [28]. Recent research has demonstrated the antimicrobial activity of npAg against a broad spectrum of microorganisms, inhibiting over 650 pathogens, including bacteria, fungi, parasites, and viruses [29]. However, it is crucial to address concerns regarding environmental contamination, cytotoxicity, and potential side effects that may arise from prolonged exposure to npAg. The properties and concentration of npAg can influence their bioactivity, with smaller particles and higher concentrations being more likely to induce adverse effects [30,31,32]. Additionally, the release of silver ions from npAg may contribute to cellular toxicity, impacting both healthy and damaged tissues [33]. Prolonged exposure to npAg within the wound environment may give rise to inflammatory reactions [34] or could result in the accumulation of silver in tissues, potentially causing systemic effects [35,36,37]. To mitigate potential side effects and enhance the safety profile, researchers are exploring various strategies. These include surface modifications [38,39,40], optimization of properties and concentration of npAg [41,42], or incorporation in controlled-release systems [43,44] to minimize cytotoxicity while retaining their therapeutic properties. Currently, there are no internationally agreed investigation standards for nanomaterials [45]. International Standards Organization (ISO) [46], the International Life Science Institute [47], the Institute of Food Science and Technology (IFST) [48], and the European Food Safety Authority (EFSA) [49] are some of the organizations that aim to regulate safety and health issues of nanomaterials.
Both antibiotics and metal nanoparticles have been integrated into a variety of scaffolds, including gels, nanofibers, nanoparticles, foams, and creams, for use as wound dressings. The type of polymer(s) and the crosslinking method stand as pivotal factors governing not only the indication and effectiveness of the end product but also its cost, accessibility, and versatility [50,51]. Erring et al. found that a nanosilver foam dressing was more efficient for re-epithelialization, healing, ease of application, and tolerance when compared to silver nanoparticle gel dressing [52]. Eskitoros-Togay et al. developed core/shell nanofibers containing DOXY for wound treatment, and the results showed good biocompatibility and enhanced drug release; however, the antimicrobial activity was not studied [53]. Abdallah et al. developed a three-dimensional biodegradable electrospun nanofiber scaffold loaded with amoxicillin for wound dressing, drug delivery, and other tissue engineering applications that showed antibacterial activity against E. coli, S. aureus, and S. pyogenes [54]. Several injectable hydrogels containing DOXY and other antibiotics have been formulated for osteoarthritis [55], chronic periodontitis [56], or wound [57,58] treatment. The literature also reports the development of wound dressings that integrate both nanoparticles and antibiotics. Ndlovu et al. developed an alginate-based dissolvable wound dressing incorporating npAg, ampicillin, and ciprofloxacin that exhibited suitable physicochemical properties and demonstrated antibacterial activity [59]. DOXY has mainly been incorporated into nanofibrous scaffolds for wound care applications. While these scaffolds present many advantages, the usage of expensive equipment and an elaborate production process may raise the cost of the final product and limit its availability. Also, the way the treatment is administered can have an impact on the patient’s adherence to the treatment (e.g., injections versus topical). To the best of our knowledge, the production of a hydrogel membrane using the proposed formulations and fabrication process employed in our study has not been previously reported in the existing literature.
In our research, we aim to develop a novel biohybrid hydrogel membrane for wound management that incorporates antimicrobial agents and is designed to be user-friendly, comfortable for patients, and economically viable for production. Our primary objective is to validate the effectiveness of the chosen crosslinking method in preserving the antimicrobial properties of DOXY. Moreover, we have developed formulations containing npAg. A thorough investigation into how the addition of DOXY or npAg influences the physicochemical properties and biocompatibility of the biohybrid hydrogel membrane was also conducted, along with the DOXY release study.
2. Materials and Methods
2.1. Chemicals and Reagents
All chemical reagents were analytical grade. Polyvinyl alcohol (PVA, Mw = 89,000–98,000, 99% hydrolyzed, MKCP0171, USA), albumin from bovine serum (BSA, fraction V, minimum 96% electrophoresis, nitrogen content 16.2%, 028K0759, USA), calcium chloride (CaCl2, pure reagent > 99%, SLBV6838, USA), doxycycline hyclate (DOXY, 0000187261, USA), silver nanoparticles (npAg, citrate stabilized, 20 nm MKCR4722 and 100 nm MKCP3854, USA), glycerol (L125H, Germany), and PEG 200 (BCCB3990, Germany) were purchased from Sigma-Aldrich. Hyaluronic acid (HA, 26337, USA) was purchased from MedChemExpress, and collagen (COL, 354231) from Corning, Europe. Sodium alginate (SA, 19L234104, Belgium) was purchased from VWR Chemicals. CellTiter 96 Aqueous One Solution Cell Proliferation Assay kit was acquired from Promega, Madison, WI, USA. Human foreskin fibroblasts (Hs27, ATCC, CRL-1634, Manassas, VA, USA) were used for cellular studies.
2.2. Bacterial Strains and Culture Media
Staphylococcus epidermidis (ATCC 12228), Staphylococcus aureus (ATCC 700699), Enterococcus faecalis (ATCC 19433), Streptococcus pyogenes (ATCC 19615), Pseudomonas aeruginosa (ATCC 10145), Acinetobacter baumannii (ATCC 19606), and Klebsiella pneumoniae (ATCC BAA-1705) strains were purchased from MediMark, Europe. Culture media were procured from Avena, Romania, and standardized doxycycline discs (30 μg, 64443624) from Bio-Rad, France.
2.3. Equipment
Micrometer (Mytutyo, Japan), pH meter (Thermo Fisher Orion Star A211, Vantaa, Finland), UH5300 Hitachi spectrophotometer (Tokyo, Japan), Anthos Zentyth 3100 spectrophotometer (Anthos, GMBH, Austria), iShak TS4 NXT Microplate Incubator Shaker (GC Life Science, Jaipur, India), Cell-IQ™ Series 5.8 cu.ft. High Heat Sterilization CO2 Incubator model MCO-170AICUVDL-PA (PHC Europe, B.V., Nijverheidsweg, The Netherlands), rheometer MFR 2100 (GBC, VIC, Australia), circulating water bath (Lauda Brinkman Ecoline E100, Suite C Marlton, NJ08053, USA), Nova NanoSEM 630 Scanning Electron Microscope (FEI Company, Hillsboro, OR, USA).
2.4. Biohybrid Hydrogel Membrane Production
The biohybrid hydrogel membranes (HM) were prepared following the two-step crosslinking process previously described by Stan et al. [60], as depicted in Figure 1 Briefly, to create the hydrogel membranes; PVA (Sigma-Aldrich, USA) was dissolved in distilled water. Separately, SA (VWR Chemicals, Belgium) and CaCl2 (Sigma-Aldrich, USA) were dispersed in glycerol (Sigma-Aldrich, Germany), and then the suspension was added to warm distilled water containing doxycycline hyclate (Sigma-Aldrich, USA) in the concentrations mentioned in . Next, the two polymer solutions were mixed until a homogeneous mixture was obtained, to which bioactive compounds, namely, HA (MedChemExpress, USA) and COL (Corning, Europe), were added. For the production of npAg-containing hydrogel membranes, the appropriate amount of npAg (Sigma-Aldrich, USA) was added to the polymeric and bioactive compound suspension . The npAg were solved in PEG 200 (Sigma-Aldrich, Germany) to achieve a final 0.75 mg/mL concentration. The blank hydrogel membranes (HM-C) and pristine hydrogel membranes (HM-Cp) were produced using the same protocol, excluding the incorporation of bioactive components. The mixture was transferred to 5 cm diameter Petri dishes, dried at 28 °C for 72 h, frozen at −20 °C for 20 h, and subjected to three 2-h freezing–thawing cycles for proper crosslinking, following a method adapted from Peppas and Stauffer [61]. The samples were kept in the dark during the production process. To ensure sterility, the samples were exposed to UV light for 15 min. The resulting biohybrid hydrogel membranes were refrigerated in tightly sealed containers until further testing. presents the formulations for all the hydrogel membranes, and Figure 1 depicts the production process.
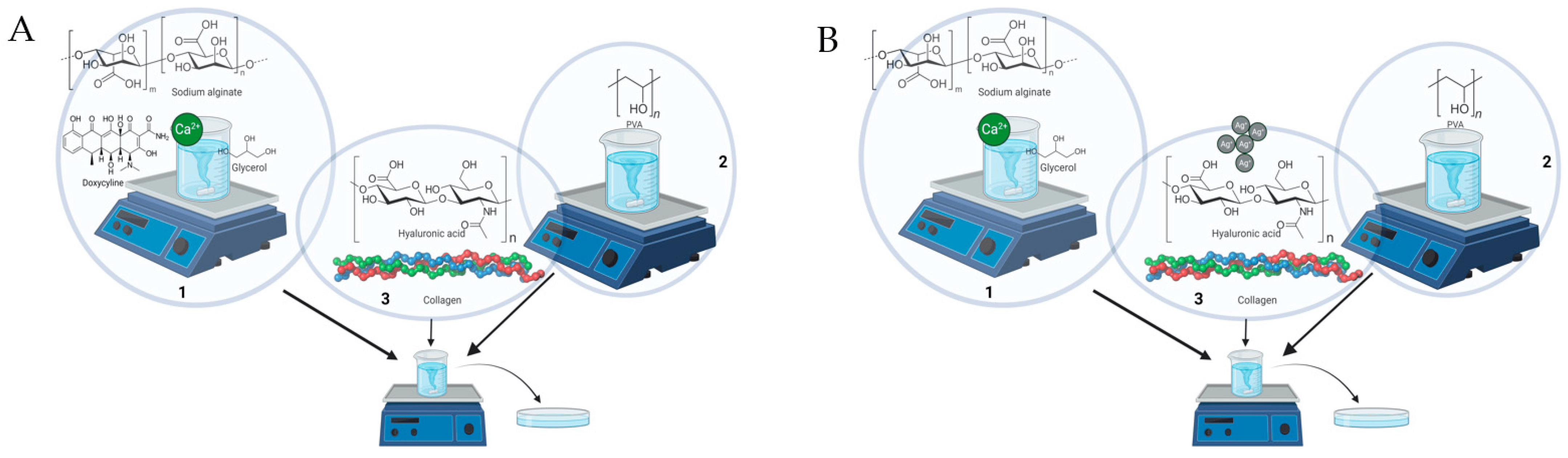
Figure 1. Production process of the hydrogel membranes. (A) Doxycycline hydrogel. (B) Silver nanoparticles hydrogel. (1). Preparation of alginate suspensions. (2). Preparation of PVA suspension. (3). Adding the final bioactive compounds.
2.5. Macroscopic Evaluation and pH
The thickness of the obtained hydrogel membranes was measured using a digital micrometer (Mytutyo, Japan). A total of five points were measured on each sample, and the obtained results are presented as the average value ± standard deviation (S.D.). For the weight variation test, each hydrogel membrane was individually weighed. For pH determination the samples were added to 10 mL of PBS (pH 7.4) and vortexed. The solution was left for 2 h so that all the hydrogel particles were deposited. Later, 5 mL of the solution was taken and analyzed using a digital pH meter (Thermo Fisher Orion Star A211, Vantaa, Finland). All samples were analyzed in triplicate, and the results are presented as mean ± standard deviation (S.D.).
2.6. Swelling Index
The swelling index (SI) of the hydrogel membranes was assessed in vitro using the gravimetric method. The simulated wound fluid (SWF, pH 8.4) was prepared following the method described in Arafa’s work [62]. The hydrogel membranes (1.5 cm diameter) were dried for 24–48 h at 55 °C until a constant weight was achieved (Wi). Subsequently, the samples were immersed in excess of SWF (37 °C, 50 rpm) and were weighed (Wf) at predetermined time intervals (5, 30 min, 1, 2, 3, 6, and 24 h). To ensure accurate measurements, excess liquid on the swollen samples was removed using filter paper before weighing, and the consumed liquid was periodically replaced to maintain complete immersion of the samples throughout the test. The SI rate was calculated using the following formula [63]:
2.7. Water Vapor Uptake
The hydrogel membranes were weighed before (Wi) and after (Wf) being placed in a chamber with a relative humidity of 75% for 72 h. The water vapor uptake (WVU) was assayed using the following formula [64]:
2.8. Gel Fraction
The in vitro evaluation of the gel fraction (GF) of the hydrogel membranes was conducted using the gravimetric method in PBS pH 7.4 at room temperature. Initially, the hydrogel membranes (1.5 cm diameter) were dried for 24–48 h at 55 °C until a constant weight was achieved (Wi). Next, the dried samples were immersed in excess PBS for a period of 24 h. After this immersion, the samples were removed from the liquid and dried again for 24–48 h at 55 °C to ensure complete evaporation of the solvent and weighted (Wf). To calculate the GF, the following formula was used [65]:
2.9. Degradation Study
The hydrogel membranes (1.5 cm in diameter) were dried for 24–48 h at 55 °C (Wi). Subsequently, the samples were immersed in PBS pH 7.4 at 37 °C for a period of 4 h. After this immersion, the samples were taken out of the liquid and dried for an additional 24–48 h at 55 °C (Wf). To assess the degradation rate (DR), the same samples underwent a second immersion in distilled water, this time for 20 h. The samples were finally dried for 24–48 h at 55 °C. The degradation rate was calculated using the provided formula [66]:
2.10. Dynamic Rheology Measurements
Oscillatory rheology investigation (frequency sweep tests) was performed on disk-shaped samples by employing a rheometer (GBC, VIC, Australia) equipped with a homemade jacket connected to a circulating water bath (Lauda Brinkman Ecoline E100, Suite C Marlton, NJ08053, USA) to ensure a constant temperature of 37.0 ± 0.1 °C during the measurements. A disk-shaped specimen was carefully placed between the two circular plates of the instrument oriented parallel to each other with a working gap between them corresponding to a relative compression of the sample of 10%. After a time period of 15 min of keeping the system at 37.0 ± 0.1 °C, the dynamic rheology measurements were carried out following a squeezing deformation induced by a motion of pseudorandom noise shape exerted on the sandwiched sample. Actually, this oscillatory displacement took place vertically by the upper plate with a very small amplitude compared to the value of the gap (thickness of the sandwiched specimen), giving rise to a corresponding force transmitted through the sample to the bottom plate below, where a very sensitive sensor recorded it continuously. The displacement and force data acquired during the measurements were processed by using a Fourier transform algorithm to finally give the values of the storage (G′) and loss (G″) moduli at 400 discrete frequencies concomitantly in the range of 0.25–100.00 Hz, with a step of 0.25 Hz. The dynamic rheological measurements were performed in triplicate (with a relative standard deviation of max. 15%), and every single rheogram was an averaged result of 30 consecutive scans acquired. The other operational parameters regarding the samples investigated and rheological measurements are listed in .
2.11. Antioxidant Activity
The constant-weight hydrogel samples (0.5 cm × 1 mm disks, approximatively 0.1 mg) were agitated in an orbital shaker at 200 rpm, 37 °C, in a solution of 1 mL 10−6 M DPPH (1 M in MeOH) diluted in ethanol/sample. The samples were incubated in the dark for 45 min. The absorbance of the samples was read at 517 nm against the control solution (the hydrogel sample free of biologically active compounds) [67]. The percentage of radicals scavenged can be determined using the following equation:
2.12. Inhibition of Protein Denaturation
To investigate the anti-inflammatory properties of the hydrogels and their capacity to inhibit protein denaturation under pro-inflammatory conditions, we adopted a methodology based on Nowak’s work [68]. Circular hydrogel samples (1 × 1 × 0.1 cm) were used for the experiments, and the following formula was used:
The samples were immersed in a 5 mL solution containing 5% BSA (Sigma-Aldrich, USA) in PBS (pH = 7.4) and incubated at 200 rpm and 37 °C for 15 min. After this initial incubation, the samples were heated at 70 °C for 5 min. Subsequently, the reaction solutions were cooled using an ice bath to reach a temperature of 25 °C. For the control experiments, we used aspirin at a concentration of 0.5 mg/mL in PBS as the positive control and water as the negative control.
2.13. Doxycycline Release Study
2.14. Antibacterial Activity
The antibacterial activity of hydrogel membranes containing npAg or DOXY was evaluated by an adapted protocol [70] against four Gram-positive bacteria (S. epidermidis, S. aureus, E. faecalis, S. pyogenes) and three Gram-negative bacteria (P. aeruginosa, A. baumanii, K. pneumoniae) employing disk diffusion test. This qualitative method is used to evaluate the antibacterial activity of samples employing zones of inhibition. First, bacterial cultures of the aforementioned strains were obtained and confirmed. Then, bacterial suspensions with 0.5 McFarland turbidity were prepared (1.5 × 108 cfu/mL). The suspensions were then inoculated on suitable sterile agar media using the spread plate method to ensure even distribution. Next, pre-cut hydrogel membrane samples of 0.5 cm diameter were placed onto the inoculated agar surface. For this assay, pristine hydrogel membranes without any bioactive compounds were prepared to determine if the addition of collagen and hyaluronic acid had any impact on the membranes’ behavior (sample HM-Cp). Also, for the positive control, standardized doxycycline discs were used (30 μg). The plates were incubated at 37 °C for 24 h to allow for bacterial growth and potential interaction with the hydrogel membranes. After the incubation period, the zone of inhibition surrounding each sample was carefully evaluated and measured. The presence and size of the inhibition zone indicated the extent of antibacterial activity against tested strains, as described by CLSI guidelines (2016). The assay was conducted in duplicate.
2.15. Biocompatibility Study
2.16. Surface Morphology
The morphological features of the biohybrid hydrogel membranes with and without antimicrobial agents were acquired using a Scanning Electron Microscope (FEI Company, Hillsboro, OR, USA) with an accelerating voltage of 5 and 10 kV. For the SEM images, all samples were coat-sputtered with Au to ensure the conductivity of the sample (60 s).
2.17. Statistical Analysis
Statistical analysis was performed using SPSS 26 (SPSS Inc., USA). More specifically, the experimental data for water vapor uptake, gel fraction, antioxidant activity, and anti-inflammatory activity were analyzed using ANOVA. Degradation rate data were analyzed using two-factor ANOVA. Data are presented as mean ± standard deviation (S.D.).
For the scratch-wound assay, statistical analysis was performed using GraphPad v7, One-Way ANOVA, and Dunnett multiple comparisons, where data were compared to the control.
3. Results and Discussion
3.1. Production of Biohybrid Hydrogel Membranes
The combination of natural and synthetic polymers in the production of wound dressings leads to a synergistic effect that enhances the material’s properties [72]. As shown in our previous work, polymer type, concentration, and the addition of bioactive compounds have the potential to significantly impact the properties of hydrogel membranes [60]. In this study, a combination of alginate and polyvinyl alcohol (PVA) was employed, alongside the inclusion of bioactive compounds like collagen and hyaluronic acid. Wound dressings can incorporate a wide range of antibiotics, such as vancomycin [73], tetracycline [74], erythromycin [75], ciprofloxacin [76,77], and gentamicin [78]. Our drug model of choice was doxycycline [7]. DOXY has been incorporated in nanofibrous membranes [79], hydrogel membranes and films [80,81], in situ gelling powder [82], microspheres [83], and sponges [84]. Metal nanoparticles have proven to be effective in enhancing the antimicrobial properties of wound dressings. They have been successfully incorporated into various scaffold materials like hydrogels [85] and nanofibers [86]. A crucial aspect when incorporating npAg into a wound dressing is to achieve a material that maintains strong antimicrobial activity while also exhibiting good biocompatibility and minimal cytotoxicity. In our methodology, we loaded the hydrogel membrane with the antimicrobial agents by directly mixing them into the formulation before the crosslinking process. Hydrogel materials are very hydrophilic, with a three-dimensional network structure that contains hydrophilic groups such as hydroxyl (−OH) or amine (−NH2) groups that may establish hydrogen bonds with water molecules and other hydrophilic molecules such as doxycycline. As a result, the molecular structure of hydrogel membranes that aid in doxycycline retention is frequently based on the network of polymeric chains of the hydrogel. In addition, the polymeric hydrogen chains form a network that can physically entrap doxycycline molecules and prevent them from diffusing out of the hydrogel when it is not hydrated. Furthermore, electrostatic interactions between the charged functional groups of the polymer and the doxycycline molecules can aid retention. To avoid potential undesired byproducts that might arise from the reaction and better control of the final concentration of the npAg, we choose to use ex situ-synthesized nanoparticles [87]. The npAg can also interact with hydroxyl and amine functional groups available in the matrix, establish electrostatic interactions, and sit into the pores of the foamed network [88,89].
3.2. Macroscopic Evaluation and pH
Following the completion of the crosslinking protocol, all samples were formed into the hydrogel membranes, and a macroscopic analysis was conducted. All samples exhibited a uniform and homogenous appearance. However, the surface of the hydrogel membranes displayed some irregularities and had impressions of crystals, likely attributed to the freeze–thaw cycles utilized during the production process. The color of the hydrogel membranes varied depending on the integrated compound, as visually depicted in Figure 2. Except for sample HM5-Dox, which contained a high concentration of DOXY and appeared dark yellow and opaque, the rest of the samples were translucent, while the control sample was transparent. The samples demonstrated favorable physical characteristics and the ability to adapt to the body curves. Each sample had a specific odor, mostly due to the addition of alginate. Moreover, all samples exhibited some degree of skin adhesion and provided a pleasant cooling sensation upon contact with intact skin. shows information about weight and thickness variation, as well as pH. The pH values of the samples ranged from 4.62 ± 0.03–7.34 ± 0.05. Notably, samples containing DOXY exhibited lower pH values, with sample HM5-Dox being the most acidic (pH 4.62 ± 0.03). This result can be attributed to the acidic nature of the DOXY solution that was added at a higher concentration. For reference, a 2% stock solution of DOXY in distilled water showed a pH value of 2.26, while the blank hydrogel membrane (sample HM-C) had a pH value of 7.34 ± 0.05. The literature also reported similar findings, demonstrating that the incorporation of DOXY resulted in a reduction in the pH values in the samples [80]. Numerous research papers have investigated the pH of the wound environment and sought to identify the most effective pH for wound dressings, considering the unique characteristics of each wound. Depending on the type of wound, both neutral and acidic pH wound dressings are considered appropriate [90]. Sample HM5-Dox, with its high DOXY concentration, would be suitable for treating chronic and complicated wounds that often exhibit high pH values, making its acidic pH beneficial in this context.
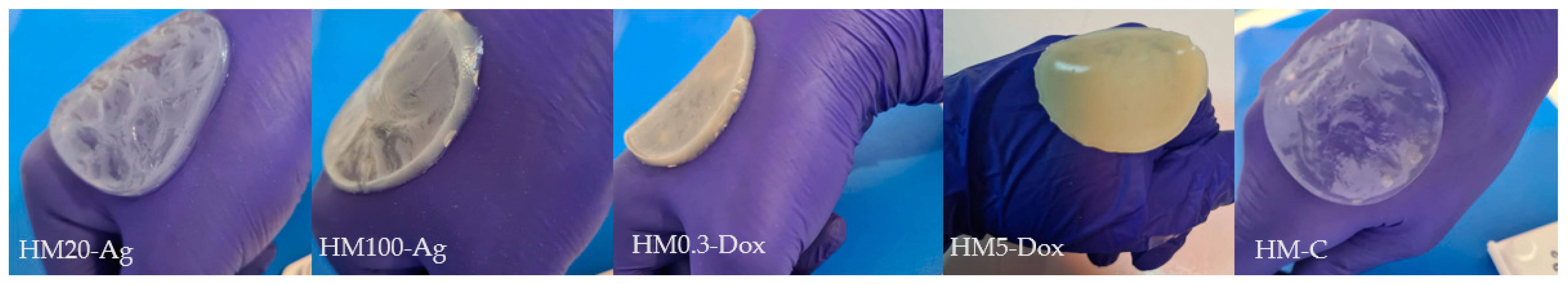
Figure 2. Visual representation of samples.
3.3. Swelling Index
The addition of both npAg and DOXY influenced the swelling behavior of the hydrogel membranes compared to the control (Figure 3). For samples HM20-Ag and HM100-Ag, the maximum swelling index was at 2 h, reaching 267.23 ± 1.96 and 254.29 ± 7.31%, respectively. Between 2 and 6 h, these samples showed an equilibrium state. However, after 6 h, the matrix began to solubilize, which led to the disruption of its water retention capacity. The presence of both 20 nm and 100 nm npAg decreased the swelling ability of the hydrogel membranes, with no significant difference observed based on nanoparticle size. These results align with findings from the existing literature [87,91,92,93] as well as with the other results obtained within this study, where the addition of npAg has been shown to diminish the crosslinking density of polymer chains and concurrently decrease the hydrophilicity of the hydrogel due to the hydrophobic nature of nanoparticles. It is worth mentioning that some studies have reported contrasting outcomes, highlighting an increase in the swelling ability upon the introduction of npAg. These results can be attributed to pore enlargement that led to superior water-holding capacity [94,95] or increased electrostatic repulsion between ionic charges in the polymer network [96]. The outcome often depends on the properties and concentrations of the nanoparticles, which may or may not impact the swelling behavior of the hydrogel [85].
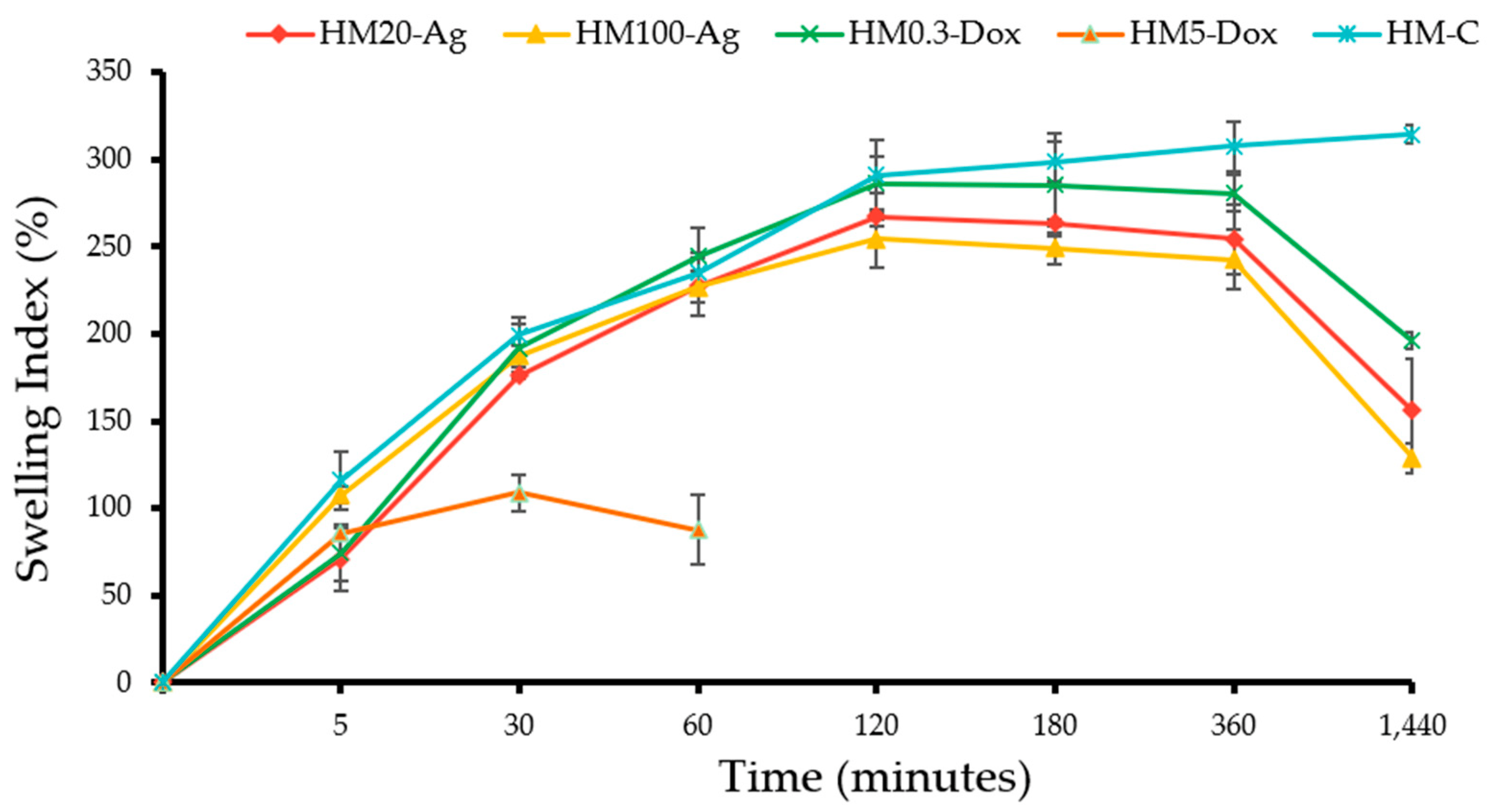
Figure 3. Swelling index of the hydrogel membranes. Samples were analyzed in triplicate, and the results are presented as mean ± S.D.
The addition of DOXY influenced the swelling behavior in a concentration-dependent manner (Figure 3). Sample HM0.3-Dox showed maximum swelling at 2 h, reaching a value of 285.68 ± 6.99%. However, beyond the 6 h timeframe, the hydrogel matrix started to solubilize, leading to a gradual decline in its water-holding ability. When compared to all other specimens, sample HM0.3-Dox exhibited the most remarkable swelling performance, similar to that of the control. Conversely, in the case of sample HM5-Dox, the introduction of a high concentration of DOXY yielded an adverse effect on the swelling ability. At 30 min, the swelling index was 108.77 ± 8.61%, followed by a rapid destructuring of the hydrogel matrix at 1 h. This instability culminated in compromised structural integrity of the sample after only 2 h, making adherence to the test protocol impossible. Hedayatyanfard et al. reported that the addition of genipin and doxycycline reduced the water uptake ability of semi-IPN films based on chitosan/PVA [81]. Patlolla et al. found that the addition of doxycycline to buccal films based on chitosan, gelatin, and Eudragit® RS led to slower water uptake [97]. We presume that the addition of DOXY can influence the hydrogel’s properties and swelling behavior due to the high number of functional groups, which could potentially disrupt the crosslinking of polymer chains within the hydrogel matrix. Also, several other factors, such as molecular size, ionic interactions, and hydrophobic–hydrophilic interactions, could potentially influence the water uptake ability.
3.4. Water Vapor Uptake
The moisture uptake values were found to be significantly different between the sample groups (p < 0.0001). Sample HM20-Ag exhibited the lowest moisture uptake capacity at 33.36 ± 0.73%, while sample HM100-Ag had the highest moisture capacity of 43.39 ± 1.91% (Figure 4) among all samples. The incorporation of smaller-sized npAg (20 nm) resulted in a reduction in the moisture uptake capacity when compared to the inclusion of 100 nm npAg and the blank hydrogel membrane. Similarly, the introduction of a higher dose of DOXY led to a decrease in moisture uptake ability when compared to the low-dose DOXY and the blank hydrogel membrane. These findings suggest that small-sized nanoparticles and a high dose of DOXY have a negative impact on the moisture uptake capacity of the hydrogel membranes. The addition of nanoparticles can influence the hydrogel’s properties, and this is largely due to the unique characteristics of nanoparticles [67,98], such as their high surface area and their ability to interact with pores [99,100]. Also, the presence of DOXY with its many functional groups [101] can influence the properties of the hydrogels by affecting the formation of bonds between the polymer chains and their ability to attract and retain water.

Figure 4. Moisture uptake of hydrogel membranes. Samples were analyzed in triplicate, and the results are presented as mean ± S.D, where **** p < 0.0001; *** p < 0.001; and * p < 0.05.
3.5. Gel Fraction
The results revealed a significant difference in gel fraction values among the sample groups (p < 0.0001). Sample HM-C had the highest gel fraction value of 41.73 ± 1.32%, while sample HM5-Dox had the lowest value of only 27.71 ± 1.4% (Figure 5). The inclusion of 20 and 100 nm npAg, as well as a low dose of DOXY, resulted in a slight decrease in the gel fraction compared to the control. However, the addition of a higher dose of DOXY significantly reduced the gel fraction. While there was not a notable reduction in gel fraction among samples containing npAg, there was a significant difference in gel fraction between samples with low and high DOXY doses. Alcântara et al. showed that the addition of silver to hydrogels obtained by ionizing radiation had little impact on the gel fraction [102]. Boonkaew et al. found that incorporating silver nitrate led to comparable gelation of the hydrogels obtained using the UV radiation technique [92]. Popescu et al. reported that the gel fraction of a hydrogel obtained by the freeze–thaw method is influenced by the concentration of chitosan-capped npAg, where higher npAg concentrations resulted in lower gel fractions [103]. We can presume that the incorporation of silver intro hydrogels may influence the formation of bonds between polymer chains, and this effect could vary based on the properties and concentration of npAg as well as the crosslinking method employed [104,105]. Due to the presence of an increased number of DOXY molecules, which possess many functional groups, the formation of non-covalent interactions between the polymer chains was hindered, resulting in a reduced gel fraction value. Wassenaar et al. demonstrated that in a PVA/alginate hydrogel produced via the freeze–thaw method, variation in polymer ratio was not the sole influencing factor of the gel fraction; the introduction of sodium ampicillin also contributed to a reduction in this value [106].
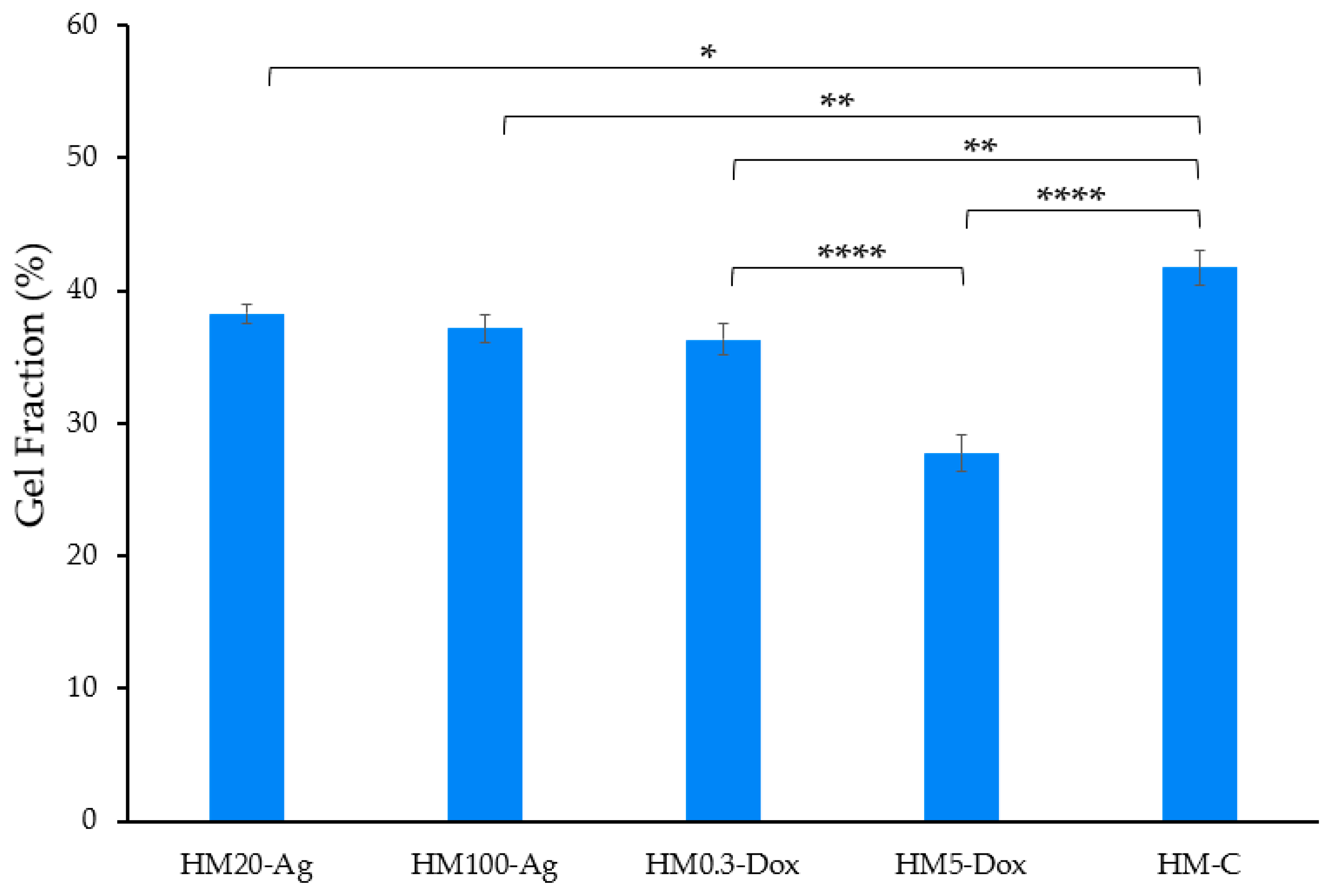
Figure 5. Gel fraction of the hydrogel membranes. Samples were analyzed in triplicate, and the results are presented as mean ± S.D. where **** p < 0.0001, ** p < 0.01, and * p < 0.05.
3.6. Degradation Study
The degradation rate of the samples ranged from 60.29 ± 1.38 to 68.46 ± 1.66% at 4 h and between 70.88 ± 1.07 and 77.10 ± 0.86% at 20 h (Figure 6). The degradation rates differ significantly between the hydrogel membranes (p < 0.0001). Degradation increased significantly from 4 h to 20 h across all samples (p < 0.0001). The change in degradation over time varies depending on the formulation (p < 0.05). The samples that contain npAg tend to have a slight reduction in the degradation rate compared to the control at 4 h but show a higher degradation rate compared to the control at 20 h, which is not statistically significant. Sample HM5-Dox consistently showed higher degradation compared to the other samples at both 4 h (68.46 ± 1.66%) and 20 h (77.10 ± 0.86%). All other comparisons between samples at 4 and 20 h are not statistically significant (p > 0.05). At both 4 h and 20 h, there was no significant difference in degradation between HM20-Ag and HM100-Ag, as well as between HM0.3-Dox and HM5-Dox (p > 0.05). These results are consistent with the gel fraction findings, suggesting a correlation between gel fraction and degradation rate, as expected. Samadi et al. showed that the addition of npAg to a glycerol/chitosan/polyvinyl alcohol-based hydrogel significantly decreased the degradation rate [91], while Qui et al. showed that an increase in npAg concentration in a hydroxypropyl methylcellulose-hydroxyapatite scaffold hydrogel leads to an increased degradation rate [105]. Wassenaar et al. investigated how DOXY incorporation affects the degradation rate of an injectable hydrogel derived from decellularized porcine ventricular myocardium. The modulation of degradation rate was evident in reduced collagenase degradation in vitro and diminished matrix degradation in vivo through MMP inhibition, while the hydrogel maintained biocompatibility and mechanical properties [107].
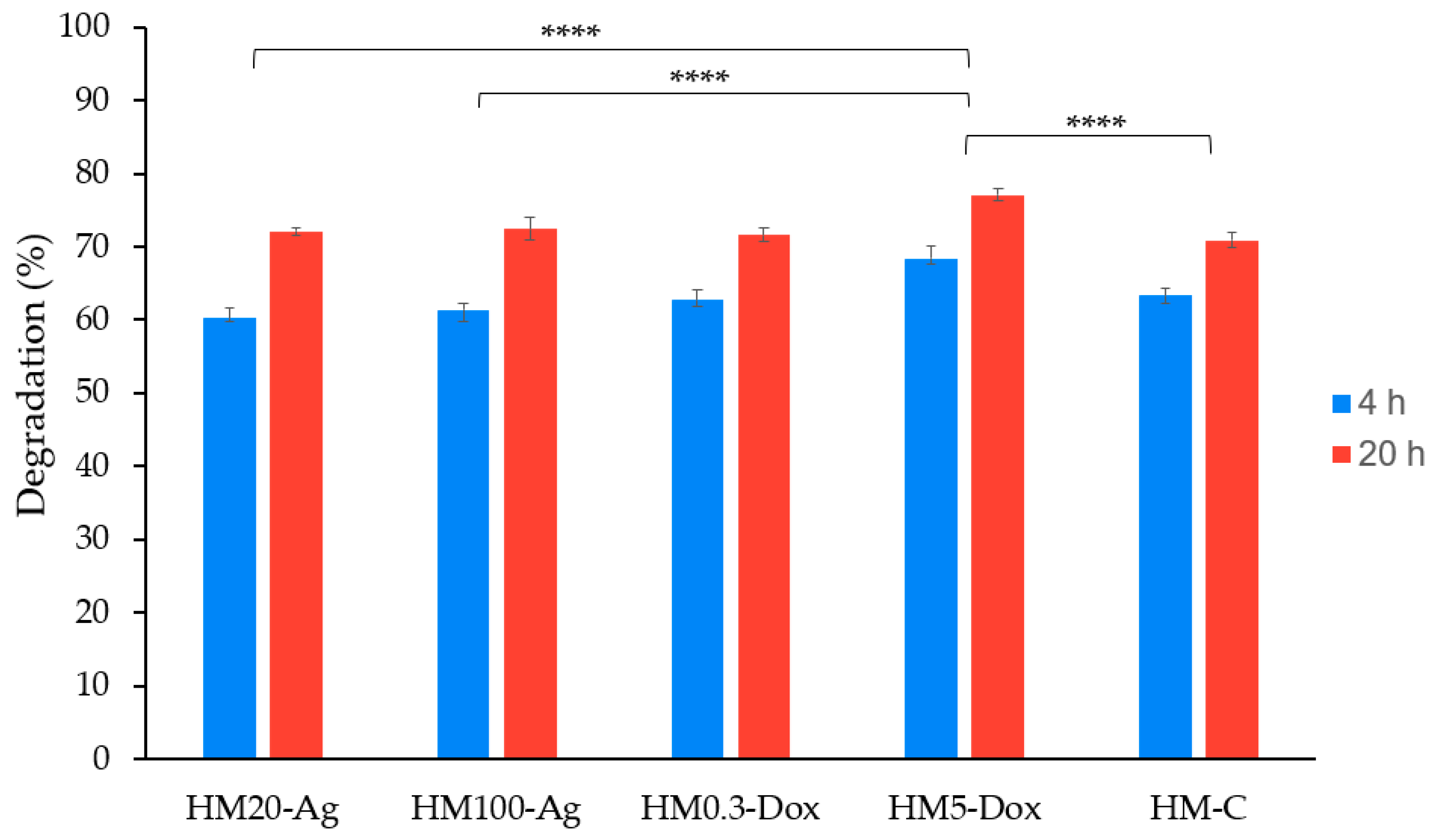
Figure 6. In vitro degradation study of hydrogel membranes at 4 and at 20 h. Samples were analyzed in triplicate, and the results are presented as mean ± S.D. where **** p < 0.0001.
3.7. Oscillatory Rheology—Frequency Sweep Tests
The investigated hydrogel membranes undergo small squeezing deformations (around 0.005%), leading to corresponding low-amplitude oscillatory shear strain (SAOS). Dynamic rheology data reveal two distinct viscoelastic states, a gel-like state (G′ > G″, frequency-independent) and a liquid-like state (G′ < G″, frequency-dependent). The crossover point, where G′ equals G″, defines a gel point. G′ represents stiffness and energy storage, while G″ indicates viscous behavior and energy dissipation as heat. This distinction is characterized by the loss tangent (tgδ) with values <1 for gel-like behavior, >1 for liquid-like behavior, and =1 at the crossover point [108,109,110,111].
The frequency-seep tests carried out on the investigated systems revealed their strong gel-like properties, with G′ values larger than those of G″ by at least one order of magnitude over the operational frequency range of 0.25–100 Hz. This well-defined behavior can be noticed in Figure 7. First of all, a comparative analysis of the rheological findings for the samples containing npAg displays quite a different behavior if considered G′-f rheograms and very similar properties when accounted for G″-f dependences (Figure 7a). Thus, taking them together, the presence of 100 nm npAg seems to strengthen the gel-like character (sample HM100-Ag) by comparison with the hydrogel containing 20 nm npAg (sample HM20-Ag). In practical terms, sample HM100-Ag (having the same rigidity as the control one) is stiffer than sample HM20-Ag, but both show a gel-like behavior following the order relationship between G′ values (Figure 7b), as mirrored by the values of loss tangent graphically plotted in Figure 8a: sample HM100-Ag is stronger (and stiffer) than sample HM20-Ag (more flexible), which is equivalent to say that the values of tgδ for HM100-Ag are generally smaller than those calculated for HM20-Ag. In this case, to partially conclude, the smaller npAg size increased the hydrogel flexibility compared to that of the control hydrogel, and adding the larger npAg maintained almost the same stiffness of the final hydrogels as for that of the control membranes, even though the gel-like character (the elastic component is by far prevalent concerning the dissipative energy/loss component) was strong for all three gels (tgδ < 0.1 for f ∈ [0.25, 100 Hz], Figure 8a).
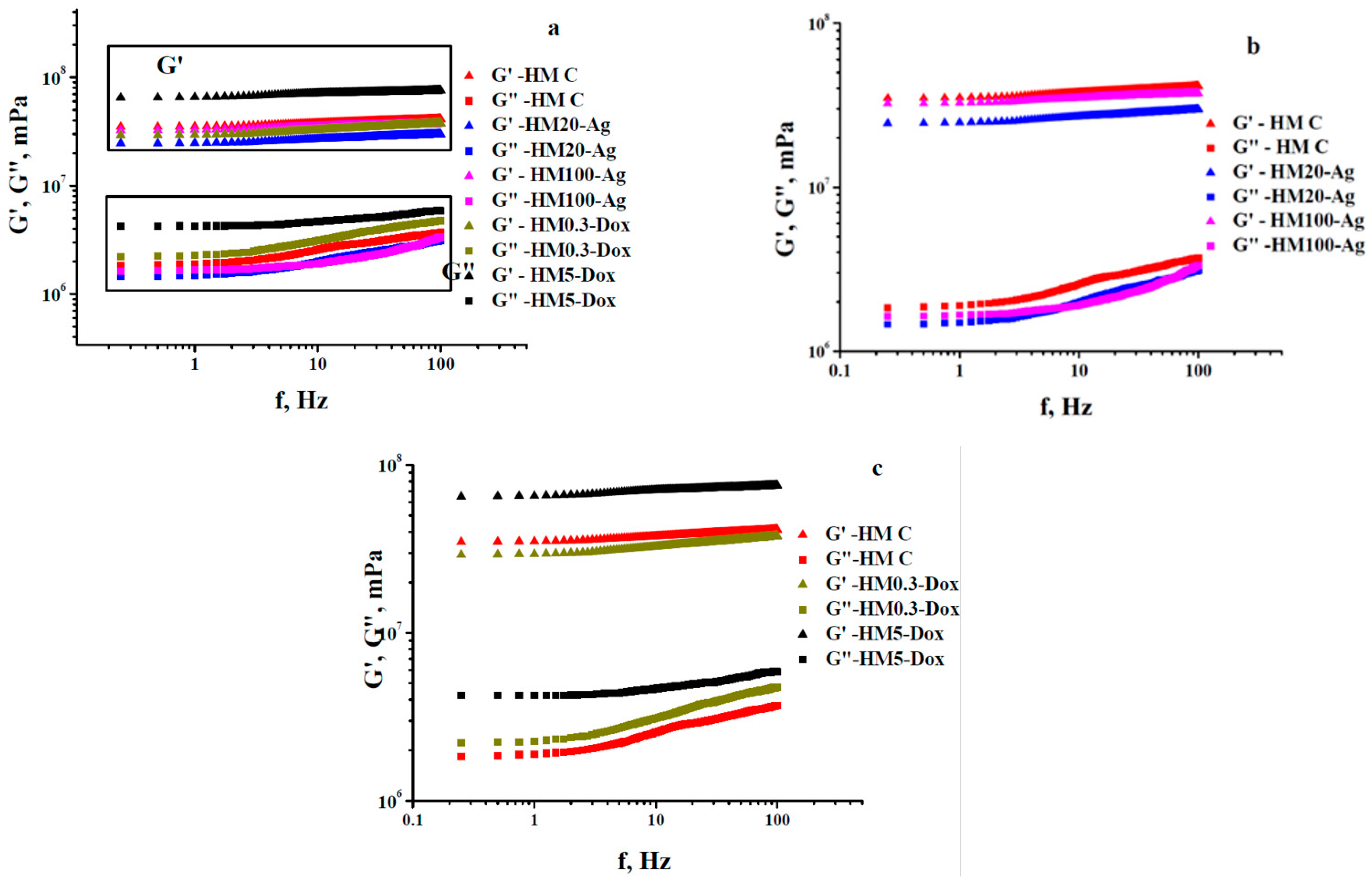
Figure 7. Frequency evolution of viscoelastic moduli acquired at 37 °C: (a) general picture outlined for all five systems; (b) comparative plots for hydrogels HM20-Ag and HM100-Ag taken in relation to those for control hydrogel; (c) comparative rheograms for hydrogels HM0.3-Dox and HM5-Dox compared to the control sample.
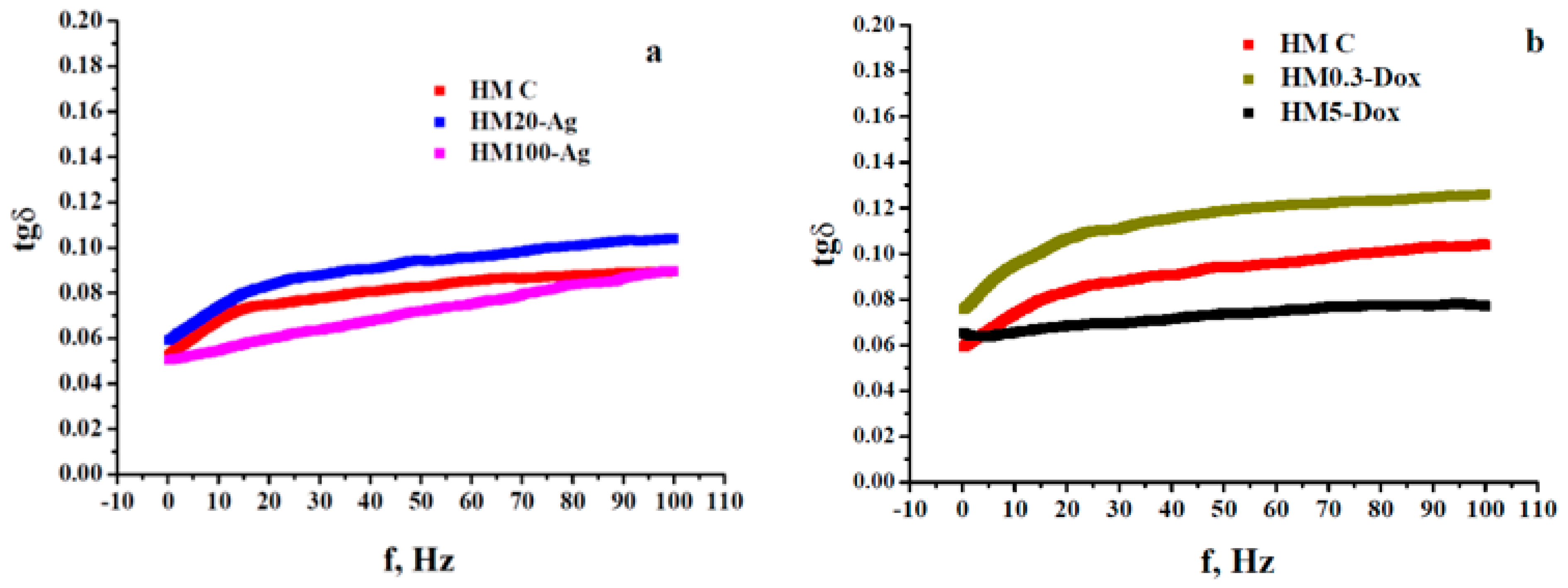
Figure 8. Comparative variation in loss tangent as a function of frequency at 37 °C for the specified hydrogels: (a) comparation between samples HM-C, HM20-Ag and HM100-Ag; (b) comparation between samples HM-C, HM0.3-Dox and HM5-Dox.
As far as the hydrogels with DOXY are concerned, the data of dynamic rheology obtained at the same temperature of 37 °C showed a viscoelastic behavior different from that exhibited by the membranes with npAg by considering the same kind of comparative analysis made toward the viscoelasticity of the control membranes. As presented in Figure 7c, a low-dose DOXY (0.3 mg/mL) resulted in the hydrogel (HM0.3-Dox) exhibiting almost the same rigidity (as indicated by the G′ values) as that of the control hydrogel (sample HM-C). Conversely, a significantly higher doxycycline content (5 mg/mL) led to increased stiffness in the samples (HM5-Dox), surpassing both HM0.3-Dox and control membranes. At the same time, a similar evolution was observed for the viscous/dissipative energy character (accounting for G″ values): the larger the content of DOXY, the higher the loss modulus values. Moreover, the two G″-f rheograms of the two doxycycline-containing hydrogels are located above that of the control hydrogels, as shown in graphs in Figure 7c. However, all these three systems displayed a pronounced gel-like character if taking into account the much smaller than unity values of loss tangent (tgδ < 0.13, Figure 8b). The enhancement of gel-like character (and also hydrogel rigidity) at higher DOXY concentrations could be related to a possible crosslinking ability of such a molecular structure via attractive interactions with some components of the hydrogel network.
The dissipative energy properties as a part of the viscoelastic behavior of the investigated hydrogels may be properly assessed by obtaining the values of dynamic viscosity (ηdyn = G″/ω, where ω is the angular frequency (in rad/s) defined as 2∙π∙f [110,112]) as a function of the frequency used during the frequency-sweep trials. The plots inserted into Figure 9a,b illustrate the same order relationships established between the rheograms G″-f shown in Figure 7, but with a substantial decrease in vertical shifting between them. Nevertheless, for all these strong enough hydrogels (G′ >> G″) for which the flow process is actually frozen during deformation, it is not advisable/practical to make an analysis based on viscosity dependences (mandatorily involving a flow phenomenon) because such an approach has a high degree of redundancy [110].
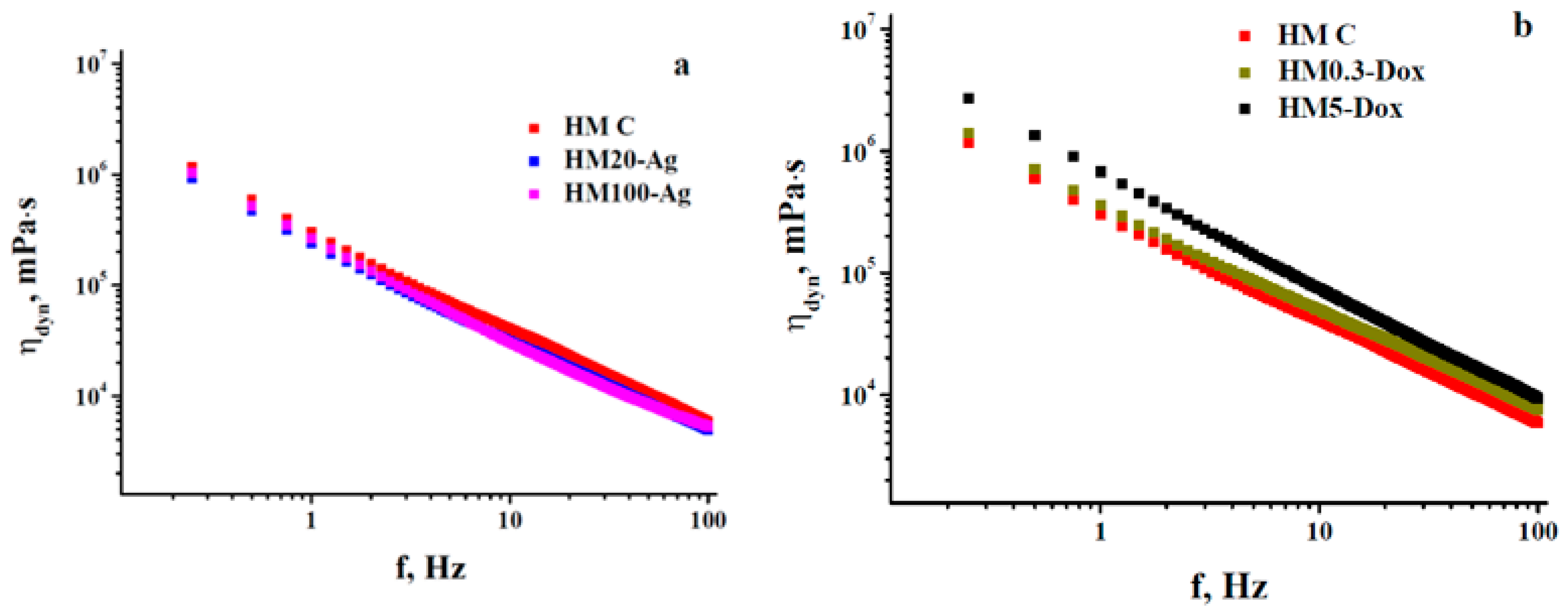
Figure 9. Frequency-dependences of dynamic viscosity measured at 37 °C for hydrogels (a) HM20-Ag—HM100-Ag and (b) HM0.3-Dox—HM5-Dox considered in comparison with that of the control sample.
The usefulness of the rheological data acquired during frequency-sweep trials at a certain temperature resides in describing the viscoelastic behavior of the hydrogels employed to mimic conditions at rest (low frequencies, Figure 10) or those under stress (different higher frequencies, Figure 7, Figure 8 and Figure 9).
3.8. Antioxidant Activity
The antioxidant activity of hydrogels was monitored using a 2,2-diphenyl-1-picrylhydrazyl (DPPH) assay [113]. The results indicate that there is a significant difference in antioxidant activity levels among the samples (p < 0.0001). The inclusion of 20 nm npAg positively influenced the antioxidant activity of the hydrogel membranes compared to the addition of 100 nm npAg. Similarly, hydrogel membranes containing a higher dose of DOXY exhibited greater antioxidant activity compared to those with a low dose of DOXY. Interestingly, sample HM5-Dox displayed significantly higher antioxidant activity compared to all other samples. This indicates that HM5-Dox may have potential benefits in terms of antioxidant properties. The experimental results of the tested hydrogels align well with the findings in the literature [114], particularly highlighting the notable scavenger activity exhibited by DOXY (attributed to the presence of hydroxyl groups), even when it is integrated within a matrix (Figure 11). Kharat and Mendhulkar assessed synthesized nanoparticles’ antioxidant activity using the DPPH assay, noting their potential as radical scavengers [115]. Priya et al. studied the antioxidant activity of nanoparticles from P. pinnata extract, demonstrating their scavenging potential [116]. Patra and Baek demonstrated robust antioxidant activity in terms of DPPH radical scavenging of npAg obtained from aqueous plant extracts [117]. These findings strongly suggest that npAg could serve as natural antioxidants for safeguarding health against oxidative stress [118]. In the same line of observations, the hydrogel formulation enriched with silver nanoparticles presents anti-scavenging activity, dependent on the size of the npAg.
3.9. Anti-Inflammatory Activity
It has been shown that preventing protein denaturation by medicinal agents in vitro indicates an anti-inflammatory effect. The assays used BSA as a model protein and aspirin as a positive control, and determinations were performed at 280 nm [60]. It was observed that all hydrogel formulations present an anti-inflammatory activity, protecting BSA from denaturation (Figure 12). The results indicate that there was a significant difference in the inhibition of protein denaturation among samples (p < 0.0001). The sample HM0.3-Dox (37.38 ± 8.1%) showed lower inhibition of protein denaturation compared to HM5-Dox (p < 0.05). Based on these results, we can conclude that the addition of DOXY in a higher concentration had a positive effect on the antioxidant effect. However, the results show that the antioxidant effect is minimally influenced by the addition of npAg or DOXY in low doses, and that is most likely attributed to the hydrogel matrix formulation, as there is no statistically significant difference between the sample HM-C and the rest of the samples (p > 0.05).
3.10. Doxycycline Release Study
3.11. Antimicrobial Analysis
In our work, we have selected seven microbial species, both Gram-positive and Gram-negative, to assess our hydrogel membrane’s antimicrobial activity and optimal drug concentrations, providing a comprehensive evaluation for potential applications (Figure 14). The samples HM-C and HM-Cp were considered negative controls due to their lack of intrinsic antibacterial activity. The samples HM0.3-Dox and HM5-Dox exhibited a clear zone of inhibition for both Gram-positive and Gram-negative bacteria. The dimension of the inhibition zone was found to be concentration-dependent, as expected (Figure 14) [7,81,82,122]. Notably, the sample HM0.3-Dox demonstrated an inhibition zone comparable to that of the standard DOXY disc for S. epidermidis, E. faecalis, S. pyogenes, P. aeruginosa, and K. pneumoniae. The sample HM5-Dox exhibited a significantly larger inhibition zone in comparison to sample HM0.3-Dox for all tested microorganisms, as expected. Our results show that the incorporation of DOXY at both low dose and high dose was successful and that DOXY maintained its clinical effect with successful release. In contrast, the samples HM20-Ag and HM-100-Ag did not display any inhibition zone for any of the tested bacterial strains (Figure 14). Recent studies reported similar results when using disk diffusion assay [123], but by using a different technique (broth dilution), the results showed that the hydrogels containing npAg had antimicrobial activity. However, the results were inconsistent for the different types of formulations [102]. The antimicrobial activity of npAg could be attributed to several factors, such as the concentration [93,124,125] and properties [94,125] of the npAg and release kinetics of the silver ions [93,124], as well as the number of microbial cells [126]. The lack of an inhibition zone might be attributed to the limited release of nanoparticles caused by the presence of polymers on their surface [127,128], which restricts their diffusion. Additionally, the stability of the silver ions (Ag+) could play a role in this phenomenon [102]. At lower concentrations, silver ions could potentially interact with the -COOH functional groups present in alginate, resulting in a reduction in the antibacterial effect [129]. Furthermore, the hydrogel discs exhibited some swelling during the 24 h assay. As a result, the absence of an inhibition zone could be attributed to the coverage caused by the swelling effect, as sometimes the inhibition zone is rather small, only a couple of mm [125,130]. The measured inhibition zones (in mm) for each sample are provided in . Upon comparing the measured inhibition zones to Clinical and Laboratory Standard Institute (CLSI) guidelines (2016), it was concluded that hydrogel membranes incorporating DOXY possessed significant antibacterial activity (see , Table A1). These findings, in conjunction with the drug release assay, support the idea that the hydrogel membranes obtained in this study effectively and optimally encapsulate and release the antimicrobial agent. Our results are similar or even superior to those reported in the existing literature for other drug delivery scaffolds [122,131,132,133]. A recent study (2019) highlighted that the nanofiber scaffold had lost the antibacterial activity compared to the film scaffold for P. aeruginosa, emphasizing the importance of scaffold selection for DOXY topical delivery [81]. Wound contamination or infection presents a challenge that hinders the healing process and gives rise to further complications [134,135,136]. The ability of wound dressings to encapsulate and release antibacterial agents is a highly desirable attribute as it not only supports wound healing but also helps prevent and treat complications [15,137]. Despite the absence of an inhibition zone in samples HM20-Ag and HM100-Ag, we observed that the hydrogel membranes incorporating npAg exhibited a notable advantage: improved storage stability at room temperature. While pristine hydrogel membranes (sample HM-Cp) demonstrated satisfactory stability when stored at room temperature, the inclusion of COL and HA (sample HM-C) led to rapid contamination of the samples under the same conditions. In contrast, samples HM20-Ag and HM100-Ag, which contained both COL, HA, and npAg, exhibited prolonged storage stability at room temperature without contamination. This observation is consistent with previously reported findings, which indicate that hydrogels incorporating npAg possess an antiseptic activity [88,127,138]. The storage stability at room temperature for samples containing DOXY was found to be satisfactory, with no contamination.
3.12. Biocompatibility Study
3.13. Surface Morphology Analysis
The microstructure of the hydrogel was assessed using SEM (Figure 19). Increasing magnification and focus led to the destruction of the hydrogel’s surface in some cases, with the appearance of cracks, so the microscope parameters had to be carefully adjusted [91]. The surface morphology of the hydrogel membranes differs among formulations. The uniform incorporation of different-sized npAg is confirmed for both sample HM20-Ag and sample HM100-Ag; however, some aggregations can be observed. As reported by other authors, npAg appears as a glowing spherical structure within the hydrogel membrane [153,154]. The surface of samples containing npAg is smooth and uniform, and the porosity of the membrane is lost compared to the rest of the samples. The hydrogel membrane appears to be more compact and denser. Wang et al. report that the hydrogel incorporated with npAg maintained the porous structure, although the mean size of the npAg was in the range of 200 nm, and the samples were freeze-dried before analysis [127]. Helmiyati et al. showed by SEM images how npAg with an average size of 20 nm occupies the pores of sodium alginate–polyvinyl alcohol–g–acrylamide hydrogel [99]. The literature reports that the addition of metal nanoparticles can have a nanofilling effect that will modify the hydrogel properties such as mechanical properties, conductivity, antimicrobial action, and other stimuli-responsive properties [87,155,156]. With the addition of DOXY, the porosity of the hydrogel membrane is preserved. The sample HM0.3-Dox showed a similar surface morphology to that of the control, with well-preserved porosity. Sample HM100-Dox exhibited increased surface roughness but also showed several pores, although the distribution was reduced.
4. Conclusions
Our extensive investigation of the biohybrid hydrogel membranes underscores their potential as highly effective wound dressings. All samples showed exceptional swelling capabilities except the high-dose DOXY hydrogel. Hydrogels incorporating 100 nm npAg or low-dose DOXY demonstrated acceptable moisture absorption capacities. All samples displayed gel-like properties. However, the incorporation of 100 nm npAg led to a notably stiffer hydrogel compared to the introduction of 20 nm npAg. Similarly, higher doses of DOXY resulted in increased rigidity of the hydrogel when compared to lower doses of DOXY. All samples exhibited a degradation rate of 70% or higher within a 20-h timeframe. High-dose DOXY hydrogel demonstrated superior antioxidant and anti-inflammatory properties when compared to all other samples. Interestingly, the pH value exhibited minimal influence on the cumulative release of DOXY over 24 h. It was observed that the release profile was more significantly affected by the concentration of DOXY, which also exerted a substantial influence on the physicochemical properties of the hydrogel membranes. Furthermore, all DOXY-containing hydrogels exhibited excellent antibacterial properties against the tested microbial strains. Also, hydrogels incorporating 100 nm npAg or low-dose DOXY demonstrated exceptional biocompatibility, yielding good results in terms of cell proliferation and cell migration. These combined characteristics make the biohybrid hydrogel membranes a promising candidate for advanced wound dressing applications. Further comprehensive analyses are warranted to gain a deeper understanding of the properties and behavior exhibited by the hydrogel membranes. This will facilitate a more nuanced exploration of their potential applications, particularly in the context of wound dressings. The absence of X-ray diffraction (XDR) or differential scanning calorimetry (DSC) investigations, which could offer valuable insights into the material’s characteristics, represents a limitation of the current study.
References
- Tottoli, E.M.; Dorati, R.; Genta, I.; Chiesa, E.; Pisani, S.; Conti, B. Skin Wound Healing Process and New Emerging Technologies for Skin Wound Care and Regeneration. Pharmaceutics 2020, 12, 735. [Google Scholar] [CrossRef] [PubMed]
- Rezvani Ghomi, E.; Niazi, M.; Ramakrishna, S. The Evolution of Wound Dressings: From Traditional to Smart Dressings. Polym. Adv. Technol. 2023, 34, 520–530. [Google Scholar] [CrossRef]
- Hydrogel Market Trends, Analysis. Forecast Report, 2032. Available online: https://www.gminsights.com/industry-analysis/hydrogel-market (accessed on 14 September 2023).
- Hydrogel Market—Size, Report & Overview. Available online: https://www.mordorintelligence.com/industry-reports/hydrogel-market (accessed on 14 September 2023).
- Augustine, R.; Hasan, A.; Dalvi, Y.B.; Rehman, S.R.U.; Varghese, R.; Unni, R.N.; Yalcin, H.C.; Alfkey, R.; Thomas, S.; Al Moustafa, A.-E. Growth Factor Loaded in Situ Photocrosslinkable Poly(3-Hydroxybutyrate-Co-3-Hydroxyvalerate)/Gelatin Methacryloyl Hybrid Patch for Diabetic Wound Healing. Mater. Sci. Eng. C 2021, 118, 111519. [Google Scholar] [CrossRef]
- Rezaei, N.; Hamidabadi, H.G.; Khosravimelal, S.; Zahiri, M.; Ahovan, Z.A.; Bojnordi, M.N.; Eftekhari, B.S.; Hashemi, A.; Ganji, F.; Darabi, S.; et al. Antimicrobial Peptides-Loaded Smart Chitosan Hydrogel: Release Behavior and Antibacterial Potential against Antibiotic Resistant Clinical Isolates. Int. J. Biol. Macromol. 2020, 164, 855–862. [Google Scholar] [CrossRef]
- Hu, Y.; Yu, B.; Jia, Y.; Lei, M.; Li, Z.; Liu, H.; Huang, H.; Xu, F.; Li, J.; Wei, Z. Hyaluronate- and Gelatin-Based Hydrogels Encapsulating Doxycycline as a Wound Dressing for Burn Injury Therapy. Acta Biomater. 2023, 164, 151–158. [Google Scholar] [CrossRef]
- Morgado, P.I.; Miguel, S.P.; Correia, I.J.; Aguiar-Ricardo, A. Ibuprofen Loaded PVA/Chitosan Membranes: A Highly Efficient Strategy towards an Improved Skin Wound Healing. Carbohydr. Polym. 2017, 159, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Gavan, A.; Colobatiu, L.; Hanganu, D.; Bogdan, C.; Olah, N.K.; Achim, M.; Mirel, S. Development and Evaluation of Hydrogel Wound Dressings Loaded with Herbal Extracts. Processes 2022, 10, 242. [Google Scholar] [CrossRef]
- Meamar, R.; Ghasemi-Mobarakeh, L.; Norouzi, M.-R.; Siavash, M.; Hamblin, M.R.; Fesharaki, M. Improved Wound Healing of Diabetic Foot Ulcers Using Human Placenta-Derived Mesenchymal Stem Cells in Gelatin Electrospun Nanofibrous Scaffolds plus a Platelet-Rich Plasma Gel: A Randomized Clinical Trial. Int. Immunopharmacol. 2021, 101, 108282. [Google Scholar] [CrossRef]
- Mousavi, S.; Khoshfetrat, A.B.; Khatami, N.; Ahmadian, M.; Rahbarghazi, R. Comparative Study of Collagen and Gelatin in Chitosan-Based Hydrogels for Effective Wound Dressing: Physical Properties and Fibroblastic Cell Behavior. Biochem. Biophys. Res. Commun. 2019, 518, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.S.; Parmar, M. Doxycycline Hyclate. In StatPearls; StatPearls Publishing: St. Petersburg, FL, USA, 2023. [Google Scholar]
- Sapadin, A.N.; Fleischmajer, R. Tetracyclines: Nonantibiotic Properties and Their Clinical Implications. J. Am. Acad. Dermatol. 2006, 54, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Golub, L.M.; Lee, H.M.; Ryan, M.E.; Giannobile, W.V.; Payne, J.; Sorsa, T. Tetracyclines Inhibit Connective Tissue Breakdown by Multiple Non-Antimicrobial Mechanisms. Adv. Dent. Res. 1998, 12, 12–26. [Google Scholar] [CrossRef] [PubMed]
- Anumolu, S.S.; Menjoge, A.R.; Deshmukh, M.; Gerecke, D.; Stein, S.; Laskin, J.; Sinko, P.J. Doxycycline Hydrogels with Reversible Disulfide Crosslinks for Dermal Wound Healing of Mustard Injuries. Biomaterials 2011, 32, 1204–1217. [Google Scholar] [CrossRef]
- Weinberg, J.M. The Anti-Inflammatory Effects of Tetracyclines. Cutis 2005, 75, 6–11. [Google Scholar] [PubMed]
- Bikowski, J.B. Subantimicrobial Dose Doxycycline for Acne and Rosacea. Skinmed Dermatol. Clin. 2003, 2, 234–245. [Google Scholar] [CrossRef]
- Anti-Inflammatory Effects of Tetracyclines—Schaller—2017—Journal of the European Academy of Dermatology and Venereology—Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/jdv.14641 (accessed on 28 August 2023).
- Stechmiller, J.; Cowan, L.; Schultz, G. The Role of Doxycycline as a Matrix Metalloproteinase Inhibitor for the Treatment of Chronic Wounds. Biol. Res. Nurs. 2010, 11, 336–344. [Google Scholar] [CrossRef] [PubMed]
- Mendes, C.; Thirupathi, A.; Corrêa, M.E.A.B.; Gu, Y.; Silveira, P.C.L. The Use of Metallic Nanoparticles in Wound Healing: New Perspectives. Int. J. Mol. Sci. 2022, 23, 15376. [Google Scholar] [CrossRef] [PubMed]
- Nam, G.; Rangasamy, S.; Purushothaman, B.; Song, J.M. The Application of Bactericidal Silver Nanoparticles in Wound Treatment. Nanomater. Nanotechnol. 2015, 5, 23. [Google Scholar] [CrossRef]
- Yin, I.X.; Zhang, J.; Zhao, I.S.; Mei, M.L.; Li, Q.; Chu, C.H. The Antibacterial Mechanism of Silver Nanoparticles and Its Application in Dentistry. Int. J. Nanomed. 2020, 15, 2555–2562. [Google Scholar] [CrossRef]
- Lin, J.; Miao, L.; Zhong, G.; Lin, C.-H.; Dargazangy, R.; Alexander-Katz, A. Understanding the Synergistic Effect of Physicochemical Properties of Nanoparticles and Their Cellular Entry Pathways. Commun. Biol. 2020, 3, 1–10. [Google Scholar] [CrossRef]
- Pal, S.; Tak, Y.K.; Song, J.M. Does the Antibacterial Activity of Silver Nanoparticles Depend on the Shape of the Nanoparticle? A Study of the Gram-Negative Bacterium Escherichia Coli. Appl. Environ. Microbiol. 2007, 73, 1712–1720. [Google Scholar] [CrossRef]
- Carlson, C.; Hussain, S.M.; Schrand, A.M.; Braydich-Stolle, L.K.; Hess, K.L.; Jones, R.L.; Schlager, J.J. Unique Cellular Interaction of Silver Nanoparticles: Size-Dependent Generation of Reactive Oxygen Species. J. Phys. Chem. B 2008, 112, 13608–13619. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.-H.; Kim, M.; Park, H.S.; Shin, U.; Gong, M.-S.; Kim, H.-W. Size-Dependent Cellular Toxicity of Silver Nanoparticles. J. Biomed. Mater. Res. Part. A 2012, 100, 1033–1043. [Google Scholar] [CrossRef] [PubMed]
- Agnihotri, S.; Mukherji, S.; Mukherji, S. Size-Controlled Silver Nanoparticles Synthesized over the Range 5–100 Nm Using the Same Protocol and Their Antibacterial Efficacy. RSC Adv. 2014, 4, 3974–3983. [Google Scholar] [CrossRef]
- Ambrožová, N.; Zálešák, B.; Ulrichová, J.; Čížková, K.; Galandáková, A. Low Concentrations of Silver Nanoparticles Have a Beneficial Effect on Wound Healing in Vitro. J. Nanopart Res. 2017, 19, 108. [Google Scholar] [CrossRef]
- Antifungal, Antiviral, and Antibacterial Activities of Silver Nanoparticles Synthesized Using Fungi: A Review. Lett. Appl. NanoBioSci. 2020, 9, 1307–1312. [CrossRef]
- Shang, L.; Nienhaus, K.; Nienhaus, G.U. Engineered Nanoparticles Interacting with Cells: Size Matters. J. Nanobiotechnol. 2014, 12, 5. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Guo, H.; Liu, L.; Liu, Y.; Xie, L. Size-Dependent Cellular Uptake and Localization Profiles of Silver Nanoparticles. Int. J. Nanomed. 2019, 14, 4247–4259. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Stenzel, M.H. Entry of Nanoparticles into Cells: The Importance of Nanoparticle Properties. Polym. Chem. 2018, 9, 259–272. [Google Scholar] [CrossRef]
- Beer, C.; Foldbjerg, R.; Hayashi, Y.; Sutherland, D.S.; Autrup, H. Toxicity of Silver Nanoparticles—Nanoparticle or Silver Ion? Toxicol. Lett. 2012, 208, 286–292. [Google Scholar] [CrossRef]
- Kobos, L.; Alqahtani, S.; Xia, L.; Coltellino, V.; Kishman, R.; McIlrath, D.; Perez-Torres, C.; Shannahan, J. Comparison of Silver Nanoparticle-Induced Inflammatory Responses Between Healthy and Metabolic Syndrome Mouse Models. J. Toxicol. Environ. Health A 2020, 83, 249–268. [Google Scholar] [CrossRef]
- Lankveld, D.P.K.; Oomen, A.G.; Krystek, P.; Neigh, A.; Troost—De Jong, A.; Noorlander, C.W.; Van Eijkeren, J.C.H.; Geertsma, R.E.; De Jong, W.H. The Kinetics of the Tissue Distribution of Silver Nanoparticles of Different Sizes. Biomaterials 2010, 31, 8350–8361. [Google Scholar] [CrossRef]
- Noga, M.; Milan, J.; Frydrych, A.; Jurowski, K. Toxicological Aspects, Safety Assessment, and Green Toxicology of Silver Nanoparticles (AgNPs)—Critical Review: State of the Art. Int. J. Mol. Sci. 2023, 24, 5133. [Google Scholar] [CrossRef] [PubMed]
- Olugbodi, J.O.; Lawal, B.; Bako, G.; Onikanni, A.S.; Abolenin, S.M.; Mohammud, S.S.; Ataya, F.S.; Batiha, G.E.-S. Effect of Sub-Dermal Exposure of Silver Nanoparticles on Hepatic, Renal and Cardiac Functions Accompanying Oxidative Damage in Male Wistar Rats. Sci. Rep. 2023, 13, 10539. [Google Scholar] [CrossRef] [PubMed]
- Bastos, V.; Ferreira de Oliveira, J.M.P.; Brown, D.; Jonhston, H.; Malheiro, E.; Daniel-da-Silva, A.L.; Duarte, I.F.; Santos, C.; Oliveira, H. The Influence of Citrate or PEG Coating on Silver Nanoparticle Toxicity to a Human Keratinocyte Cell Line. Toxicol. Lett. 2016, 249, 29–41. [Google Scholar] [CrossRef] [PubMed]
- Das, B.; Tripathy, S.; Adhikary, J.; Chattopadhyay, S.; Mandal, D.; Dash, S.K.; Das, S.; Dey, A.; Dey, S.K.; Das, D.; et al. Surface Modification Minimizes the Toxicity of Silver Nanoparticles: An in Vitro and in Vivo Study. J. Biol. Inorg. Chem. 2017, 22, 893–918. [Google Scholar] [CrossRef]
- Vega-Chacón, J.; Arbeláez, M.I.A.; Jorge, J.H.; Marques, R.F.C.; Jafelicci, M. pH-Responsive Poly(Aspartic Acid) Hydrogel-Coated Magnetite Nanoparticles for Biomedical Applications. Mater. Sci. Eng. C 2017, 77, 366–373. [Google Scholar] [CrossRef]
- Helmlinger, J.; Sengstock, C.; Groß-Heitfeld, C.; Mayer, C.; Schildhauer, A.T.; Köller, M.; Epple, M. Silver Nanoparticles with Different Size and Shape: Equal Cytotoxicity, but Different Antibacterial Effects. RSC Adv. 2016, 6, 18490–18501. [Google Scholar] [CrossRef]
- Menichetti, A.; Mavridi-Printezi, A.; Mordini, D.; Montalti, M. Effect of Size, Shape and Surface Functionalization on the Antibacterial Activity of Silver Nanoparticles. J. Funct. Biomater. 2023, 14, 244. [Google Scholar] [CrossRef]
- Agnihotri, S.; Mukherji, S.; Mukherji, S. Antimicrobial Chitosan–PVA Hydrogel as a Nanoreactor and Immobilizing Matrix for Silver Nanoparticles. Appl. Nanosci. 2012, 2, 179–188. [Google Scholar] [CrossRef]
- Bhowmick, S.; Koul, V. Assessment of PVA/Silver Nanocomposite Hydrogel Patch as Antimicrobial Dressing Scaffold: Synthesis, Characterization and Biological Evaluation. Mater. Sci. Eng. C 2016, 59, 109–119. [Google Scholar] [CrossRef]
- King, T.; Osmond-McLeod, M.J.; Duffy, L.L. Nanotechnology in the Food Sector and Potential Applications for the Poultry Industry. Trends Food Sci. Technol. 2018, 72, 62–73. [Google Scholar] [CrossRef]
- ISO/TS 13830:2013; 14:00–17:00. ISO: Geneva, Switzerland. Available online: https://www.iso.org/standard/54315.html (accessed on 12 October 2023).
- International Life Sciences Institute. Available online: https://ilsi.org/ (accessed on 12 October 2023).
- Nanosciences and Nanotechnologies: An Action Plan for Europe 2005–2009. Second Implementation Report 2007–2009.
- The Potential Risks Arising from Nanoscience and Nanotechnologies on Food and Feed Safety. EFSA. Available online: https://www.efsa.europa.eu/en/efsajournal/pub/958 (accessed on 12 October 2023).
- Zielińska, A.; Karczewski, J.; Eder, P.; Kolanowski, T.; Szalata, M.; Wielgus, K.; Szalata, M.; Kim, D.; Shin, S.R.; Słomski, R.; et al. Scaffolds for Drug Delivery and Tissue Engineering: The Role of Genetics. J. Control. Release 2023, 359, 207–223. [Google Scholar] [CrossRef] [PubMed]
- Coelho, J.F.; Ferreira, P.C.; Alves, P.; Cordeiro, R.; Fonseca, A.C.; Góis, J.R.; Gil, M.H. Drug Delivery Systems: Advanced Technologies Potentially Applicable in Personalized Treatments. EPMA J. 2010, 1, 164–209. [Google Scholar] [CrossRef] [PubMed]
- Erring, M.; Gaba, S.; Mohsina, S.; Tripathy, S.; Sharma, R.K. Comparison of Efficacy of Silver-Nanoparticle Gel, Nano-Silver-Foam and Collagen Dressings in Treatment of Partial Thickness Burn Wounds. Burns 2019, 45, 1888–1894. [Google Scholar] [CrossRef] [PubMed]
- Eskitoros-Togay, Ş.M.; Bulbul, Y.E.; Dilsiz, N. Controlled Release of Doxycycline within Core/Shell Poly(ε-Caprolactone)/Poly(Ethylene Oxide) Fibers via Coaxial Electrospinning. J. Appl. Polym. Sci. 2020, 137, 49273. [Google Scholar] [CrossRef]
- Abdallah, O.; Jalali, F.; Zamani, S.; Isamil, H.M.; Ma, S.; Nasrallah, G.K.; Younes, H.M. Fabrication & Characterization of 3D Electrospun Biodegradable Nanofibers for Wound Dressing, Drug Delivery and Other Tissue Engineering Applications. Pharm. Nanotechnol. 2016, 4, 191–201. [Google Scholar] [PubMed]
- Lu, H.-T.; Sheu, M.-T.; Lin, Y.-F.; Lan, J.; Chin, Y.-P.; Hsieh, M.-S.; Cheng, C.-W.; Chen, C.-H. Injectable Hyaluronic-Acid-Doxycycline Hydrogel Therapy in Experimental Rabbit Osteoarthritis. BMC Vet. Res. 2013, 9, 68. [Google Scholar] [CrossRef]
- Zhao, X.; Yang, Y.; Yu, J.; Ding, R.; Pei, D.; Zhang, Y.; He, G.; Cheng, Y.; Li, A. Injectable Hydrogels with High Drug Loading through B-N Coordination and ROS-Triggered Drug Release for Efficient Treatment of Chronic Periodontitis in Diabetic Rats. Biomaterials 2022, 282, 121387. [Google Scholar] [CrossRef]
- Liang, Y.; Zhao, X.; Hu, T.; Han, Y.; Guo, B. Mussel-Inspired, Antibacterial, Conductive, Antioxidant, Injectable Composite Hydrogel Wound Dressing to Promote the Regeneration of Infected Skin. J. Colloid. Interface Sci. 2019, 556, 514–528. [Google Scholar] [CrossRef]
- Dong, M.; Mao, Y.; Zhao, Z.; Zhang, J.; Zhu, L.; Chen, L.; Cao, L. Novel Fabrication of Antibiotic Containing Multifunctional Silk Fibroin Injectable Hydrogel Dressing to Enhance Bactericidal Action and Wound Healing Efficiency on Burn Wound: In Vitro and in Vivo Evaluations. Int. Wound J. 2022, 19, 679–691. [Google Scholar] [CrossRef]
- Ndlovu, S.P.; Fonkui, T.Y.; Ndinteh, D.T.; Aderibigbe, B.A. Dissolvable Wound Dressing Loaded with Silver Nanoparticles Together with Ampicillin and Ciprofloxacin. Ther. Deliv. 2022, 13, 295–311. [Google Scholar] [CrossRef] [PubMed]
- Stan, D.; Codrici, E.; Enciu, A.-M.; Olewnik-Kruszkowska, E.; Gavril, G.; Ruta, L.L.; Moldovan, C.; Brincoveanu, O.; Bocancia-Mateescu, L.-A.; Mirica, A.-C.; et al. Exploring the Impact of Alginate—PVA Ratio and the Addition of Bioactive Substances on the Performance of Hybrid Hydrogel Membranes as Potential Wound Dressings. Gels 2023, 9, 476. [Google Scholar] [CrossRef] [PubMed]
- Ritger, P.L.; Peppas, N.A. A Simple Equation for Description of Solute Release I. Fickian and Non-Fickian Release from Non-Swellable Devices in the Form of Slabs, Spheres, Cylinders or Discs. J. Control. Release 1987, 5, 23–36. [Google Scholar] [CrossRef]
- Arafa, A.A.; Nada, A.A.; Ibrahim, A.Y.; Zahran, M.K.; Hakeim, O.A. Greener Therapeutic pH-Sensing Wound Dressing Based on Curcuma Longa and Cellulose Hydrogel. Eur. Polym. J. 2021, 159, 110744. [Google Scholar] [CrossRef]
- Barleany, D.R.; Ananta, C.; Maulina, F.; Rochmat, A.; Alwan, H.; Erizal, E. Controlled Release of Metformin Hydrogen Chloride from Stimuli-Responsive Hydrogel Based on Poly(N-Isopropylacrylamide)/Chitosan/Polyvinyl Alcohol Composite. Int. J. Technol. 2020, 11, 511. [Google Scholar] [CrossRef]
- Chopra, H.; Bibi, S.; Kumar, S.; Khan, M.S.; Kumar, P.; Singh, I. Preparation and Evaluation of Chitosan/PVA Based Hydrogel Films Loaded with Honey for Wound Healing Application. Gels 2022, 8, 111. [Google Scholar] [CrossRef] [PubMed]
- Wu, N.; Yu, H.; Sun, M.; Li, Z.; Zhao, F.; Ao, Y.; Chen, H. Investigation on the Structure and Mechanical Properties of Highly Tunable Elastomeric Silk Fibroin Hydrogels Cross-Linked by Gamma-Ray Radiation. ACS Appl. Bio Mater. 2019, 3, 721–734. [Google Scholar] [CrossRef]
- Sasikala, L.; Durai, B.; Rathinamoorthy, R.; Author, C. Manuka Honey Loaded Chitosan Hydrogel Films for Wound Dressing Applications. Int. J. PharmTech Res. 2013, 5, 1774–1785. [Google Scholar]
- Kang, B.; Vales, T.P.; Cho, B.-K.; Kim, J.-K.; Kim, H.-J. Development of Gallic Acid-Modified Hydrogels Using Interpenetrating Chitosan Network and Evaluation of Their Antioxidant Activity. Molecules 2017, 22, 1976. [Google Scholar] [CrossRef]
- Nowak, A.; Zagórska-Dziok, M.; Perużyńska, M.; Cybulska, K.; Kucharska, E.; Ossowicz-Rupniewska, P.; Piotrowska, K.; Duchnik, W.; Kucharski, Ł.; Sulikowski, T.; et al. Assessment of the Anti-Inflammatory, Antibacterial and Anti-Aging Properties and Possible Use on the Skin of Hydrogels Containing Epilobium angustifolium L. Extracts. Front. Pharmacol. 2022, 13, 896706. [Google Scholar] [CrossRef]
- Dash, S.; Murthy, P.N.; Nath, L.; Chowdhury, P. Kinetic Modeling on Drug Release from Controlled Drug Delivery Systems. Acta Pol. Pharm. 2010, 67, 217–223. [Google Scholar]
- Delavari, M.M.; Stiharu, I. Preparation and Characterization of Eco-Friendly Transparent Antibacterial Starch/Polyvinyl Alcohol Materials for Use as Wound-Dressing. Micromachines 2022, 13, 960. [Google Scholar] [CrossRef]
- Gago, D.; Corvo, M.C.; Chagas, R.; Ferreira, L.M.; Coelhoso, I. Protein Adsorption Performance of a Novel Functionalized Cellulose-Based Polymer. Polymers 2022, 14, 5122. [Google Scholar] [CrossRef] [PubMed]
- Augustine, R.; Dan, P.; Schlachet, I.; Rouxel, D.; Menu, P.; Sosnik, A. Chitosan Ascorbate Hydrogel Improves Water Uptake Capacity and Cell Adhesion of Electrospun Poly(Epsilon-Caprolactone) Membranes. Int. J. Pharm. 2019, 559, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Saif, A.B.; Jabbar, S.; Akhtar, M.S.; Mushtaq, A.; Tariq, M. Effects of Topical Vancomycin Dressing on Methicillin-Resistant Staphylococcus Aureus (MRSA) Positive Diabetic Foot Ulcers. Pak. J. Med. Sci. 2019, 35, 1099–1103. [Google Scholar] [CrossRef]
- Chen, H.; Li, B.; Feng, B.; Wang, H.; Yuan, H.; Xu, Z. Tetracycline Hydrochloride Loaded Citric Acid Functionalized Chitosan Hydrogel for Wound Healing. RSC Adv. 2019, 9, 19523–19530. [Google Scholar] [CrossRef] [PubMed]
- Movassaghi, S.; Nadia Sharifi, Z.; Koosha, M.; Abdollahifar, M.A.; Fathollahipour, S.; Tavakoli, J.; Abdi, S. Effect of Honey/PVA Hydrogel Loaded by Erythromycin on Full-Thickness Skin Wound Healing in Rats; Stereological Study. Galen. Med. J. 2019, 8, e1362. [Google Scholar] [CrossRef]
- Kowalczuk, D.; Miazga-Karska, M.; Gładysz, A.; Warda, P.; Barańska, A.; Drop, B. Characterization of Ciprofloxacin-Bismuth-Loaded Antibacterial Wound Dressing. Molecules 2020, 25, 5096. [Google Scholar] [CrossRef]
- Heydari, P.; Zargar Kharazi, A.; Asgary, S.; Parham, S. Comparing the Wound Healing Effect of a Controlled Release Wound Dressing Containing Curcumin/Ciprofloxacin and Simvastatin/Ciprofloxacin in a Rat Model: A Preclinical Study. J. Biomed. Mater. Res. A 2022, 110, 341–352. [Google Scholar] [CrossRef] [PubMed]
- AlSalem, H.S.; Bukhari, A.A.H. Biodegradable Wound Dressing-Based Collagen/Hyaluronic Acid Loaded Antibacterial Agents for Wound Healing Application. Int. J. Biol. Macromol. 2023, 242, 124700. [Google Scholar] [CrossRef]
- Tort, S.; Acartürk, F.; Beşikci, A. Evaluation of Three-Layered Doxycycline-Collagen Loaded Nanofiber Wound Dressing. Int. J. Pharm. 2017, 529, 642–653. [Google Scholar] [CrossRef]
- Ardika, K.A.R.; Marzaman, A.N.F.; Kaharuddin, K.M.; Parenden, M.D.K.; Karimah, A.; Musfirah, C.A.; Pakki, E.; Permana, A.D. Development of Chitosan-Hyaluronic Acid Based Hydrogel for Local Delivery of Doxycycline Hyclate in an Ex Vivo Skin Infection Model. J. Biomater. Sci. Polym. Ed. 2023, 34, 2274–2290. [Google Scholar] [CrossRef] [PubMed]
- Hedayatyanfard, K.; Bagheri Khoulenjani, S.; Abdollahifar, M.A.; Amani, D.; Habibi, B.; Zare, F.; Asadirad, A.; Pouriran, R.; Ziai, S.A. Chitosan/PVA/Doxycycline Film and Nanofiber Accelerate Diabetic Wound Healing in a Rat Model. Iran. J. Pharm. Res. 2020, 19, 225–239. [Google Scholar] [CrossRef] [PubMed]
- Amante, C.; Esposito, T.; Del Gaudio, P.; Di Sarno, V.; Porta, A.; Tosco, A.; Russo, P.; Nicolais, L.; Aquino, R.P. A Novel Three-Polysaccharide Blend In Situ Gelling Powder for Wound Healing Applications. Pharmaceutics 2021, 13, 1680. [Google Scholar] [CrossRef] [PubMed]
- Adhirajan, N.; Shanmugasundaram, N.; Babu, M. Gelatin Microspheres Cross-Linked with EDC as a Drug Delivery System for Doxycyline: Development and Characterization. J. Microencapsul. 2007, 24, 647–659. [Google Scholar] [CrossRef] [PubMed]
- Patel, N.; Hatch, D.; Wells, C.M.; Ahn, D.; Harris, M.; Jennings, J.A.; Haggard, W.; Armstrong, D.G. Characteristics and Clinical Assessment of Antibiotic Delivery by Chitosan Sponge in the High-Risk Diabetic Foot: A Case Series. J. Wound Care 2017, 26, S32–S38. [Google Scholar] [CrossRef] [PubMed]
- Sulastri, E.; Lesmana, R.; Zubair, M.S.; Abdelwahab Mohammed, A.F.; Elamin, K.M.; Wathoni, N. Ulvan/Silver Nanoparticle Hydrogel Films for Burn Wound Dressing. Heliyon 2023, 9, e18044. [Google Scholar] [CrossRef] [PubMed]
- GhavamiNejad, A.; Rajan Unnithan, A.; Ramachandra Kurup Sasikala, A.; Samarikhalaj, M.; Thomas, R.G.; Jeong, Y.Y.; Nasseri, S.; Murugesan, P.; Wu, D.; Hee Park, C.; et al. Mussel-Inspired Electrospun Nanofibers Functionalized with Size-Controlled Silver Nanoparticles for Wound Dressing Application. ACS Appl. Mater. Interfaces 2015, 7, 12176–12183. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, K.B.; Han, S.S. Dual-Crosslinked Poly(Vinyl Alcohol)/Sodium Alginate/Silver Nanocomposite Beads—A Promising Antimicrobial Material. Food Chem. 2017, 234, 103–110. [Google Scholar] [CrossRef]
- Pangli, H.; Vatanpour, S.; Hortamani, S.; Jalili, R.; Ghahary, A. Incorporation of Silver Nanoparticles in Hydrogel Matrices for Controlling Wound Infection. J. Burn. Care Res. 2020, 42, 785–793. [Google Scholar] [CrossRef]
- Azizi-Lalabadi, M.; Garavand, F.; Jafari, S.M. Incorporation of Silver Nanoparticles into Active Antimicrobial Nanocomposites: Release Behavior, Analyzing Techniques, Applications and Safety Issues. Adv. Colloid. Interface Sci. 2021, 293, 102440. [Google Scholar] [CrossRef] [PubMed]
- Sim, P.; Strudwick, X.L.; Song, Y.; Cowin, A.J.; Garg, S. Influence of Acidic pH on Wound Healing In Vivo: A Novel Perspective for Wound Treatment. Int. J. Mol. Sci. 2022, 23, 13655. [Google Scholar] [CrossRef]
- Samadi, A.; Azandeh, S.; Orazizadeh, M.; Bayati, V.; Rafienia, M.; Karami, M.A. Fabrication and Characterization of Glycerol/Chitosan/Polyvinyl Alcohol-Based Transparent Hydrogel Films Loaded with Silver Nanoparticles for Antibacterial Wound Dressing Applications. Adv. Biomed. Res. 2021, 10, 4. [Google Scholar] [CrossRef]
- Boonkaew, B.; Suwanpreuksa, P.; Cuttle, L.; Barber, P.M.; Supaphol, P. Hydrogels Containing Silver Nanoparticles for Burn Wounds Show Antimicrobial Activity without Cytotoxicity. J. Appl. Polym. Sci. 2014, 131. [Google Scholar] [CrossRef]
- Aldakheel, F.M.; Mohsen, D.; El Sayed, M.M.; Alawam, K.A.; Binshaya, A.S.; Alduraywish, S.A. Silver Nanoparticles Loaded on Chitosan-g-PVA Hydrogel for the Wound-Healing Applications. Molecules 2023, 28, 3241. [Google Scholar] [CrossRef] [PubMed]
- Song, S.; Liu, Z.; Abubaker, M.A.; Ding, L.; Zhang, J.; Yang, S.; Fan, Z. Antibacterial Polyvinyl Alcohol/Bacterial Cellulose/Nano-Silver Hydrogels That Effectively Promote Wound Healing. Mater. Sci. Eng. C 2021, 126, 112171. [Google Scholar] [CrossRef]
- Yang, J.; Chen, Y.; Zhao, L.; Feng, Z.; Peng, K.; Wei, A.; Wang, Y.; Tong, Z.; Cheng, B. Preparation of a Chitosan/Carboxymethyl Chitosan/AgNPs Polyelectrolyte Composite Physical Hydrogel with Self-Healing Ability, Antibacterial Properties, and Good Biosafety Simultaneously, and Its Application as a Wound Dressing. Compos. Part. B Eng. 2020, 197, 108139. [Google Scholar] [CrossRef]
- Solbu, A.A.; Caballero, D.; Damigos, S.; Kundu, S.C.; Reis, R.L.; Halaas, Ø.; Chahal, A.S.; Strand, B.L. Assessing Cell Migration in Hydrogels: An Overview of Relevant Materials and Methods. Mater. Today Bio 2023, 18, 100537. [Google Scholar] [CrossRef]
- Patlolla, V.G.R.; Popovic, N.; Peter Holbrook, W.; Kristmundsdottir, T.; Gizurarson, S. Effect of Doxycycline Microencapsulation on Buccal Films: Stability, Mucoadhesion and In Vitro Drug Release. Gels 2021, 7, 51. [Google Scholar] [CrossRef]
- Szałaj, U.; Świderska-Środa, A.; Chodara, A.; Gierlotka, S.; Łojkowski, W. Nanoparticle Size Effect on Water Vapour Adsorption by Hydroxyapatite. Nanomaterials 2019, 9, 1005. [Google Scholar] [CrossRef] [PubMed]
- Helmiyati; Novientri, G.; Abbas, G.H.; Budianto, E. Nanocomposite Hydrogel-Based Biopolymer Modified with Silver Nanoparticles as an Antibacterial Material for Wound Treatment. J. App. Pharm. Sci. 2019, 9, 001–009. [Google Scholar] [CrossRef]
- Rodríguez Nuñez, Y.A.; Castro, R.I.; Arenas, F.A.; López-Cabaña, Z.E.; Carreño, G.; Carrasco-Sánchez, V.; Marican, A.; Villaseñor, J.; Vargas, E.; Santos, L.S.; et al. Preparation of Hydrogel/Silver Nanohybrids Mediated by Tunable-Size Silver Nanoparticles for Potential Antibacterial Applications. Polymers 2019, 11, 716. [Google Scholar] [CrossRef] [PubMed]
- PubChem Doxycycline. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/54671203 (accessed on 27 August 2023).
- Alcântara, M.T.S.; Lincopan, N.; Santos, P.M.; Ramirez, P.A.; Brant, A.J.C.; Riella, H.G.; Lugão, A.B. Simultaneous Hydrogel Crosslinking and Silver Nanoparticle Formation by Using Ionizing Radiation to Obtain Antimicrobial Hydrogels. Radiat. Phys. Chem. 2020, 169, 108777. [Google Scholar] [CrossRef]
- Popescu, I.; Constantin, M.; Pelin, I.M.; Suflet, D.M.; Ichim, D.L.; Daraba, O.M.; Fundueanu, G. Eco-Friendly Synthesized PVA/Chitosan/Oxalic Acid Nanocomposite Hydrogels Embedding Silver Nanoparticles as Antibacterial Materials. Gels 2022, 8, 268. [Google Scholar] [CrossRef]
- Mohamadinia, P. Preparation and Characterization of Sodium Alginate/Acrylic Acid Composite Hydrogels Conjugated to Silver Nanoparticles As An Antibiotic Delivery System. Green Process. Synth. 2021, 10, 860–873. [Google Scholar] [CrossRef]
- Qiu, Y.; Sun, X.; Lin, X.; Yi, W.; Jiang, J. An Injectable Metal Nanoparticle Containing Cellulose Derivative-based Hydrogels: Evaluation of Antibacterial and in Vitro-vivo Wound Healing Activity in Children with Burn Injuries. Int. Wound J. 2021, 19, 666–678. [Google Scholar] [CrossRef]
- Kamoun, E.A.; Kenawy, E.-R.S.; Tamer, T.M.; El-Meligy, M.A.; Mohy Eldin, M.S. Poly (Vinyl Alcohol)-Alginate Physically Crosslinked Hydrogel Membranes for Wound Dressing Applications: Characterization and Bio-Evaluation. Arab. J. Chem. 2015, 8, 38–47. [Google Scholar] [CrossRef]
- Wassenaar, J.W.; Braden, R.L.; Osborn, K.G.; Christman, K.L. Modulating in Vivo Degradation Rate of Injectable Extracellular Matrix Hydrogels. J. Mater. Chem. B 2016, 4, 2794–2802. [Google Scholar] [CrossRef]
- Coupland, J.N. An Introduction to the Physical Chemistry of Food; Springer: Berlin/Heidelberg, Germany, 2014; ISBN 978-1-4939-0761-8. [Google Scholar]
- Grillet, A.M.; Wyatt, N.B.; Gloe, L.M. Polymer Gel Rheology and Adhesion. Rheology 2012, 3, 59–80. [Google Scholar]
- Mezger, T.G. The Rheology Handbook: For Users of Rotational and Oscillatory Rheometers; Vincentz Network GmbH & Co KG: Hannover, Germany, 2006; ISBN 978-3-87870-174-3. [Google Scholar]
- Borzacchiello, A.; Ambrosio, L. Structure-Property Relationships in Hydrogels. In Hydrogels: Biological Properties and Applications; Barbucci, R., Ed.; Springer: Milan, Italy, 2009; pp. 9–20. ISBN 978-88-470-1104-5. [Google Scholar]
- Staicu, T.; Iliş, M.; Cîrcu, V.; Micutz, M. Influence of Hydrocarbon Moieties of Partially Fluorinated N-Benzoyl Thiourea Compounds on Their Gelation Properties. A Detailed Rheological Study of Complex Viscoelastic Behavior of Decanol/N-Benzoyl Thiourea Mixtures. J. Mol. Liq. 2018, 255, 297–312. [Google Scholar] [CrossRef]
- Galanakis, C.M. Nutraceutical and Functional Food Components: Effects of Innovative Processing Techniques; Academic Press: London, UK, 2017; ISBN 978-0-12-809650-5. [Google Scholar]
- Tort, S.; Demiröz, F.T.; Coşkun Cevher, Ş.; Sarıbaş, S.; Özoğul, C.; Acartürk, F. The Effect of a New Wound Dressing on Wound Healing: Biochemical and Histopathological Evaluation. Burns 2020, 46, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Kharat, S.N.; Mendhulkar, V.D. Synthesis, Characterization and Studies on Antioxidant Activity of Silver Nanoparticles Using Elephantopus Scaber Leaf Extract. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 62, 719–724. [Google Scholar] [CrossRef] [PubMed]
- Priya, R.S.; Geetha, D.; Ramesh, P.S. Antioxidant Activity of Chemically Synthesized AgNPs and Biosynthesized Pongamia Pinnata Leaf Extract Mediated AgNPs—A Comparative Study. Ecotoxicol. Environ. Saf. 2016, 134, 308–318. [Google Scholar] [CrossRef] [PubMed]
- Patra, J.K.; Baek, K.-H. Biosynthesis of Silver Nanoparticles Using Aqueous Extract of Silky Hairs of Corn and Investigation of Its Antibacterial and Anticandidal Synergistic Activity and Antioxidant Potential. IET Nanobiotechnol 2016, 10, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Mohanta, Y.K.; Panda, S.K.; Jayabalan, R.; Sharma, N.; Bastia, A.K.; Mohanta, T.K. Antimicrobial, Antioxidant and Cytotoxic Activity of Silver Nanoparticles Synthesized by Leaf Extract of Erythrina suberosa (Roxb.). Front. Mol. Biosci. 2017, 4, 14. [Google Scholar] [CrossRef]
- Caló, E.; Khutoryanskiy, V.V. Biomedical Applications of Hydrogels: A Review of Patents and Commercial Products. Eur. Polym. J. 2015, 65, 252–267. [Google Scholar] [CrossRef]
- Bhasarkar, J.; Bal, D. Kinetic Investigation of a Controlled Drug Delivery System Based on Alginate Scaffold with Embedded Voids. J. Appl. Biomater. Funct. Mater. 2019, 17, 2280800018817462. [Google Scholar] [CrossRef]
- Peppas, N.; Korsmeyer, R. Dynamically Swelling Hydrogel in Controlled Release Application. Hydrogels Med. Pharm. 1986, 3, 109–136. [Google Scholar]
- Khampieng, T.; Wnek, G.; Supaphol, P. Electrospun DOXY-h Loaded-Poly(Acrylic Acid) Nanofiber Mats: In Vitro Drug Release and Antibacterial Properties Investigation. J. Biomater. Sci. Polym. Ed. 2014, 25, 1–14. [Google Scholar] [CrossRef]
- Khampieng, T.; Wongkittithavorn, S.; Chaiarwut, S.; Ekabutr, P.; Pavasant, P.; Supaphol, P. Silver Nanoparticles-Based Hydrogel: Characterization of Material Parameters for Pressure Ulcer Dressing Applications. J. Drug Deliv. Sci. Technol. 2018, 44, 91–100. [Google Scholar] [CrossRef]
- Nguyen, T.D.; Nguyen, T.T.; Ly, K.L.; Tran, A.H.; Nguyen, T.T.N.; Vo, M.T.; Ho, H.M.; Dang, N.T.N.; Vo, V.T.; Nguyen, D.H.; et al. In Vivo Study of the Antibacterial Chitosan/Polyvinyl Alcohol Loaded with Silver Nanoparticle Hydrogel for Wound Healing Applications. Int. J. Polym. Sci. 2019, 2019, e7382717. [Google Scholar] [CrossRef]
- Archana, D.; Singh, B.K.; Dutta, J.; Dutta, P.K. Chitosan-PVP-Nano Silver Oxide Wound Dressing: In Vitro and in Vivo Evaluation. Int. J. Biol. Macromol. 2015, 73, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Sondi, I.; Salopek-Sondi, B. Silver Nanoparticles as Antimicrobial Agent: A Case Study on E. Coli as a Model for Gram-Negative Bacteria. J. Colloid. Interface Sci. 2004, 275, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Zhang, F.; Zhao, R.; Wang, C.; Hu, K.; Sun, Y.; Politis, C.; Shavandi, A.; Nie, L. Polyvinyl Alcohol/Sodium Alginate Hydrogels Incorporated with Silver Nanoclusters via Green Tea Extract for Antibacterial Applications. Des. Monomers Polym. 2020, 23, 118–133. [Google Scholar] [CrossRef]
- Ahmed, E.M. Hydrogel: Preparation, Characterization, and Applications: A Review. J. Adv. Res. 2015, 6, 105–121. [Google Scholar] [CrossRef]
- Zakia, M.; Koo, J.M.; Kim, D.; Ji, K.; Huh, P.; Yoon, J.; Yoo, S.I. Development of Silver Nanoparticle-Based Hydrogel Composites for Antimicrobial Activity. Green. Chem. Lett. Rev. 2020, 13, 34–40. [Google Scholar] [CrossRef]
- Eghbalifam, N.; Frounchi, M.; Dadbin, S. Antibacterial Silver Nanoparticles in Polyvinyl Alcohol/Sodium Alginate Blend Produced by Gamma Irradiation. Int. J. Biol. Macromol. 2015, 80, 170–176. [Google Scholar] [CrossRef]
- Adhirajan, N.; Shanmugasundaram, N.; Shanmuganathan, S.; Babu, M. Functionally Modified Gelatin Microspheres Impregnated Collagen Scaffold as Novel Wound Dressing to Attenuate the Proteases and Bacterial Growth. Eur. J. Pharm. Sci. 2009, 36, 235–245. [Google Scholar] [CrossRef]
- Hafezi Moghaddam, R.; Dadfarnia, S.; Shabani, A.M.H.; Amraei, R.; Hafezi Moghaddam, Z. Doxycycline Drug Delivery Using Hydrogels of O-Carboxymethyl Chitosan Conjugated with Caffeic Acid and Its Composite with Polyacrylamide Synthesized by Electron Beam Irradiation. Int. J. Biol. Macromol. 2020, 154, 962–973. [Google Scholar] [CrossRef]
- Varshosaz, J.; Arabloo, K.; Sarrami, N.; Ghassami, E.; Yazdani Kachouei, E.; Kouhi, M.; Jahanian-Najafabadi, A. RGD Peptide Grafted Polybutylene Adipate-Co-Terephthalate/Gelatin Electrospun Nanofibers Loaded with a Matrix Metalloproteinase Inhibitor Drug for Alleviating of Wounds: An in Vitro/in Vivo Study. Drug Dev. Ind. Pharm. 2020, 46, 484–497. [Google Scholar] [CrossRef]
- Guo, S.; DiPietro, L.A. Factors Affecting Wound Healing. J. Dent. Res. 2010, 89, 219–229. [Google Scholar] [CrossRef]
- Basu, S.; Shukla, V. Complications of Wound Healing. In Measurements in Wound Healing: Science and Practice; Mani, R., Romanelli, M., Shukla, V., Eds.; Springer: London, UK, 2013; pp. 109–144. ISBN 978-1-4471-2987-5. [Google Scholar]
- Gushiken, L.F.S.; Beserra, F.P.; Bastos, J.K.; Jackson, C.J.; Pellizzon, C.H. Cutaneous Wound Healing: An Update from Physiopathology to Current Therapies. Life 2021, 11, 665. [Google Scholar] [CrossRef]
- Moore, A.L.; desJardins-Park, H.E.; Duoto, B.A.; Mascharak, S.; Murphy, M.P.; Irizarry, D.M.; Foster, D.S.; Jones, R.E.; Barnes, L.A.; Marshall, C.D.; et al. Doxycycline Reduces Scar Thickness and Improves Collagen Architecture. Ann. Surg. 2020, 272, 183–193. [Google Scholar] [CrossRef]
- Ghasemzadeh, H.; Ghanaat, F. Antimicrobial Alginate/PVA Silver Nanocomposite Hydrogel, Synthesis and Characterization. J. Polym. Res. 2014, 21, 355. [Google Scholar] [CrossRef]
- Rahmati, M.; Mozafari, M. Protein Adsorption on Polymers. Mater. Today Commun. 2018, 17, 527–540. [Google Scholar] [CrossRef]
- Yoon, J.-Y.; Kim, J.-H.; Kim, W.-S. The Relationship of Interaction Forces in the Protein Adsorption onto Polymeric microspheres1This Paper Was Presented in the 7th Iketani Conference—International Symposium on Advanced Technology of Fine Particles, October 1997, Yokohama Symposia, Japan.1. Colloids Surf. A Physicochem. Eng. Asp. 1999, 153, 413–419. [Google Scholar] [CrossRef]
- O’Brien, J.; Shea, K.J. Tuning the Protein Corona of Hydrogel Nanoparticles: The Synthesis of Abiotic Protein and Peptide Affinity Reagents. Acc. Chem. Res. 2016, 49, 1200–1210. [Google Scholar] [CrossRef]
- Catanzano, O.; Docking, R.; Schofield, P.; Boateng, J. Advanced Multi-Targeted Composite Biomaterial Dressing for Pain and Infection Control in Chronic Leg Ulcers. Carbohydr. Polym. 2017, 172, 40–48. [Google Scholar] [CrossRef]
- Avalos, A.; Haza, A.I.; Mateo, D.; Morales, P. Interactions of Manufactured Silver Nanoparticles of Different Sizes with Normal Human Dermal Fibroblasts. Int. Wound J. 2014, 13, 101–109. [Google Scholar] [CrossRef]
- Löfdahl, A.; Jern, A.; Flyman, S.; Kåredal, M.; Karlsson, H.L.; Larsson-Callerfelt, A.-K. Silver Nanoparticles Alter Cell Viability Ex Vivo and in Vitro and Induce Proinflammatory Effects in Human Lung Fibroblasts. Nanomaterials 2020, 10, 1868. [Google Scholar] [CrossRef]
- Gliga, A.R.; Skoglund, S.; Odnevall Wallinder, I.; Fadeel, B.; Karlsson, H.L. Size-Dependent Cytotoxicity of Silver Nanoparticles in Human Lung Cells: The Role of Cellular Uptake, Agglomeration and Ag Release. Part. Fibre Toxicol. 2014, 11, 11. [Google Scholar] [CrossRef]
- Akter, M.; Sikder, M.T.; Rahman, M.M.; Ullah, A.K.M.A.; Hossain, K.F.B.; Banik, S.; Hosokawa, T.; Saito, T.; Kurasaki, M. A Systematic Review on Silver Nanoparticles-Induced Cytotoxicity: Physicochemical Properties and Perspectives. J. Adv. Res. 2018, 9, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Wang, L.; Chen, Q.; Chen, C. Cytotoxic Potential of Silver Nanoparticles. Yonsei Med. J. 2014, 55, 283. [Google Scholar] [CrossRef] [PubMed]
- Cui, S.; Sun, X.; Li, K.; Gou, D.; Zhou, Y.; Hu, J.; Liu, Y. Polylactide Nanofibers Delivering Doxycycline for Chronic Wound Treatment. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 104, 109745. [Google Scholar] [CrossRef]
- de A Vieira, L.F.; Lins, M.P.; Viana, I.M.M.N.; dos Santos, J.E.; Smaniotto, S.; Reis, M.D. dos S. Metallic Nanoparticles Reduce the Migration of Human Fibroblasts in Vitro. Nanoscale Res. Lett. 2017, 12, 200. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.Y.C.; Clements, D.; Johnson, S.R. Effect of Doxycycline on Proliferation, MMP Production, and Adhesion in LAM-Related Cells. Am. J. Physiol. Lung Cell. Mol. Physiol. 2010, 299, L393–L400. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.-M.; Kang, J.-H.; Lee, S.-A.; Park, I.-H.; Lee, H.-M. Effect of Doxycycline on Epithelial-Mesenchymal Transition via the P38/Smad Pathway in Respiratory Epithelial Cells. Am. J. Rhinol. Allergy 2017, 31, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.-F.; Cheng, H.-T.; Chen, H.-Y.; Yeung, W.K.; Cheng, J.-Y. Doxycycline Inhibits Electric Field-Induced Migration of Non-Small Cell Lung Cancer (NSCLC) Cells. Sci. Rep. 2019, 9, 8094. [Google Scholar] [CrossRef] [PubMed]
- Masood, N.; Ahmed, R.; Tariq, M.; Ahmed, Z.; Masoud, M.S.; Ali, I.; Asghar, R.; Andleeb, A.; Hasan, A. Silver Nanoparticle Impregnated Chitosan-PEG Hydrogel Enhances Wound Healing in Diabetes Induced Rabbits. Int. J. Pharm. 2019, 559, 23–36. [Google Scholar] [CrossRef]
- Chandrasekharan, S.; Chinnasamy, G.; Bhatnagar, S. Sustainable Phyto-Fabrication of Silver Nanoparticles Using Gmelina Arborea Exhibit Antimicrobial and Biofilm Inhibition Activity. Sci. Rep. 2022, 12, 156. [Google Scholar] [CrossRef] [PubMed]
- Xing, W.; Tang, Y. On Mechanical Properties of Nanocomposite Hydrogels: Searching for Superior Properties. Nano Mater. Sci. 2022, 4, 83–96. [Google Scholar] [CrossRef]
- Xu, D.; Gersappe, D. Structure Formation in Nanocomposite Hydrogels. Soft Matter 2017, 13, 1853–1861. [Google Scholar] [CrossRef] [PubMed]

