1. Introduction
Maternity is a term used to define assistance and medical care provided to a woman during her pregnancy and delivery. The state of being expecting or anticipating a child is called pregnancy. Maternity is the time following childbirth [1]. Critical maternal care is a rapidly developing area of clinical practice [1]. The World Health Organization (WHO) recommends respectful maternity care [2], which is defined as components of inclusive and respectful maternity care that include maintaining a woman’s privacy, dignity, and confidentiality; guaranteeing her anonymity from harm and mistreatment; allowing the woman to make an educated decision; and to receive ongoing support throughout her pregnancy and delivery [2]. In providing prospective knowledge and seeking informed consent, continuous access to relatives and local support, women value care that respects their culture, values, and beliefs [3] as well as improving the physical environment and resources, making maternity care better for everyone, providing care that is effective and productive, care stability, and participating in effective conversation [2,3].
The most effective way to maintain safety and ease is through ongoing technological monitoring, maintenance, medication, and to prompt expert assistance when problems emerge [4]. Inclusive and respectful maternity care is a human right, as stated in the 2012 technical guidance on the application of a human rights-based strategy to the implementation of policies and initiatives to decrease preventable maternal morbidity and mortality, as well as the Universal Rights of Childbearing Women Charter from the White Ribbon Alliance [3,5,6]. Access to interventions, medicines, and commodities is insufficient to ensure quality maternal and newborn care [6]. Respectful and inclusive care is a fundamental component of high-quality, clinically secure care, but, more significantly, it feels psychologically and emotionally safe to the woman and her family [7]. This means that treatment must include respect, community knowledge and values, be tailored to women’s needs, and be delivered by health professionals who combine clinical knowledge and skills with interpersonal and cultural competence [8].
Respectful maternity care (RMC) includes all of these aspects and more, and it should be a fundamental component of all maternity care providers in every nation [3,7,8,9]. Another approach is enhanced maternal care [1]. Enhanced maternal care was developed to standardize and deliver the specialized monitoring, treatment, and attention a specific patient may require in maternal or obstetric critical care [1]. The need for skills to treat pregnant, postpartum, or perinatal women who have obstetric, surgical, or medical issues but are not critically ill enough to be admitted to a critical care center drives the development of enhanced maternal care [1]. Any practitioner with the required skills may offer this form of care [1,10].
Moreover, one more approach used for maternal care is evidence-based maternity care. To assist in guiding maternity care decisions and facilitating the best outcomes for mothers and newborns, it uses the most current studies on the effectiveness and safety of specific practices [11]. Evidence-based maternal care in facilities should include humane and dignified care regarding women’s fundamental rights [12]. Respectful maternity care is a term international maternal health organizations use to describe this approach [12]. Obstetric patient treatment is becoming increasingly complex due to comorbidities and advancing maternal age, with socioeconomic factors additionally playing an important part [1]. Another major factor affecting maternity care is income. Evidence demonstrated that lack of income had been associated with poor maternal and newborn health outcomes [13]. Considering the factor of income, maternal care differs in low- and middle-income countries. A list of some low- and middle-income countries is indicated below .
Socioeconomic status (SES) is one of the key factors affecting healthcare outcomes. When SES is inadequate, medical care is insufficient, which has been related to detrimental outcomes [14]. Expectant women with low SES may experience more unfavorable pregnancy outcomes [14,15]. Low SES has been linked to pregnancy complications such as preterm birth, abortion, eclampsia, preeclampsia, and gestational diabetes, according to earlier research [14]. Poor prenatal care is related to poor obstetric outcomes, including preterm delivery, preeclampsia, and stillbirth, and women from low SES are less likely to be provided with it [14,15].
Despite improvements in reproductive, maternal, newborn, and pediatric health, disparities in low- and middle-income countries (LMICs) remain significant [13]. In addition to the approximately 4.5 million infants born stillborn or that pass away within the first week of life, it is estimated that nearly 300,000 women worldwide pass away while giving birth each year. Most of these occur in low- and middle-income nations [16] and can be prevented with proper care [13,17]. Giving birth in a health facility lowers maternal and neonatal mortality. However, in low- and middle-income countries, such as Haiti, Kenya, Malawi, Namibia, Nepal, and Tanzania, using facilities more frequently has not always resulted in lower mortality rates. In these nations, many deliveries occur in primary healthcare facilities, where the standard of treatment is substandard [18].
Moreover, in Canada, it has been estimated that every year, approximately 100,000 children are born into poverty [19]. A baby’s health endures greatly during the first few years of life due to poverty and pregnancy, frequently resulting in health inequalities later in life [19]. Low- and middle-income countries carry a significant maternal and newborn mortality burden worldwide. Maternal mortality is typically considered the mother’s death during pregnancy or within the first 42 days following delivery. Maternal mortality rates are 50–100 times higher in low- and some middle-income nations than high-income countries [20]. Most low- and some middle-income countries’ leading causes of maternal mortality are hemorrhage, hypertensive disorders, and maternal infections [20,21,22].
To bring these high levels down, the standard of care must be improved [23]. Maternal and neonatal mortality rates are still high in many low- and middle-income countries, despite substantial decreases over the previous 20 years [18]. Maternal mortality reduction is a top priority for the Sustainable Development Goals (SDGs), which set a global average maternal mortality goal of 70 per 100,000 live births and an additional national target that states that by 2030, no country should have a Maternal Mortality Ratio (MMR) of >140 per 100,000 live births [18]. Additionally, targets were established for each nation’s newborn mortality rate and stillbirth rate to be 12 or less per 1000 live births and 1000 total births, respectively. With an average yearly decrease of 2.9% between 2000 and 2017, there were almost 300,000 maternal and neonatal deaths in women in low- and middle-income countries in 2017 [17].
Advances in maternal and perinatal health and survival were being made through several programs. The worldwide initiatives Every Newborn Action Plan (ENAP) and Ending Preventable Maternal Mortality (EPMM), which focus on stillbirths and neonatal deaths, respectively, seek to hasten and monitor improvements to maternal, perinatal, and newborn health and wellbeing [17]. Although many nations have started the execution process, more aggressive efforts are required to operationalize at the national level to achieve the SDGs [24]. Reviewing current approaches to increase maternal and perinatal survival and wellbeing is necessary, drawing on available data and lessons learned while considering changing epidemiology and demography [17,18,24,25].
According to a study, pregnant women in low-income groups, compared to middle-income, receive worse care, with the most underprivileged being 60% less likely than the least underprivileged to attain antenatal care. The inadequate maternal quality of care constrains improvements in maternal and perinatal results [12]. Poor quality treatment frequently results from a push for births in facilities with insufficient staff, training, infrastructure, and equipment and insufficient evidence-based clinical practice [12]. This type of treatment is known as “Too Little, Too Late” (TLTL). On the other hand, widespread overmedicalization of childbirth has been accompanied by the rapid rise in facility use, especially in middle-income countries (MICs) [26]. The benefits from improvements in maternal and perinatal health may be offset by this excessive medicalization, which we typically refer to as “Too Much, Too Soon” (TMTS) [27]. The clinical care component of the increasing variety and divergence in maternal health is represented by TLTL and TMTS [12]. Individual practitioners in facilities can prevent TLTL or TMTS by adhering to evidence-based clinical standards [12,26,27].
Furthermore, respectful maternity care should be followed by utilizing several measures. Much of the fetal mortality has been decreased by monitoring the fetus during pregnancy and delivery using various methods, such as fetal heart rate monitoring and delivery for signs of distress [20]. The maternal health community has concentrated on ways to lower maternal mortality in low-income and middle-income countries (LMICs), including addressing the direct causes of pregnancy-related deaths, increasing skilled birth attendance, encouraging facility births, and guaranteeing everyone access to essential maternal health care. These approaches have had some degree of effectiveness [12]. A respectful maternity care scale can also assess women’s perceptions of respectful maternity care in health care institutions [28]. The RMC scale of 15 items is a valid and reliable measure. It signifies that hospitals use the RMC scale in urban public health institutions and that other researchers conduct additional exploratory and confirmatory factor analyses [28].
This systematic review aims to determine the impact of income on maternal care and respectful maternity care in low- and middle-income countries.
2. Materials and Methods
2.1. Search Strategy
In order to execute this review, recent research and review articles/publications based on respectful maternity care in low- and middle-income countries were considered. Data were gathered from the following electronic databases: Google Scholar, PubMed, Web of Science, NCBI, Hindawi, CINAHL, PLoS ONE, National Library of Medicine, ResearchGate, Internal Medicine Journal, MEDLINE, EMBASE database, Science Direct, Scopus, Cochrane Central Register of Controlled Trials (CENTRAL), Maternity and Infant Care (MIC) database, and BioMed.
For this study, we searched through the literature to find articles addressing the meaning of respectful maternity care in low- and middle-income countries and compared them. Studies were selected from years 2010 to 2023 using keywords comprising ‘Respectful maternity’, ‘Care in Low and Middle-Income Countries’, ‘Respectful Maternity Care’, ‘Motherhood’, Childbearing’, ‘Maternity Precautions’, ‘Pregnant Women’, ‘Low and medium income countries’, ‘Attitude of Health Personnel’, ‘Obstetrics’, ‘Delivery’, ‘Delivery Obstetrics’, ‘Infants’, ‘Nursing’, ‘Maternity Care’, ‘Nurse-Patient Relations’, ‘Maternity’, ‘Maternity & care Regulations’, ‘Effects of Income on Pregnancy’, ‘Association between Income and Maternity Care’, ‘Pregnancy and Precautions’, and ‘Income Effect on Maternity Care.’ Search keywords were combined using proximity operators (NEAR, NEXT, WITHIN) and Boolean (AND, OR) operators. indicates the data selection strategy for this review.
First, following a search of databases for pertinent articles, text words contained in the title and abstract and index terms used to describe the article were analyzed. Then, across all databases, a second search was conducted using all the discovered keywords, index terms, and MeSH terms for MEDLINE. Third, new studies were found by searching the reference lists of all the studies, reports, and articles. Fourth, databases were searched to identify all related articles and reports in LMICs such as PubMed, Google Scholar, and Google. Titles and abstracts were examined for the search terms. Access was made to the whole texts of the articles that were found. PRISMA guidelines were followed for this review.
The SPIDER framework was employed to determine which studies to include in this systematic review, as shown in . The PICO model was also used to evaluate databases, as shown in .
2.2. Study Design
2.3. Study Outcomes
2.4. Inclusion Criteria
The following addition and omission criteria were used to filter the titles rather than study relevance. We only selected the studies submitted to peer-reviewed journals for approval that were already published. These studies were taken into consideration to understand the research criteria better.
2.5. Exclusion Criteria
The exclusion criteria involve
The outcomes of this systematic review were summarized and made explicit by the exclusion and inclusion criteria. Articles that failed to meet the criteria for eligibility were eliminated, duplicate records were eliminated, records with irrelevant titles, abstracts, and keywords were removed, and articles for which no full text was available were also excluded. Most papers were eliminated due to their no direct relevance to this study’s main goal and were written primarily in languages other than English, most commonly Arabic, French, Spanish, and Dutch.
2.6. Data Extraction
Using Microsoft Excel, the researcher extracted and sorted the sample size, study type, duplicates, full-text articles, and empirical studies, making this systematic review approach practicable. The reason for the exclusion and reduction of data is depicted in the flowchart, as seen in Figure 1.
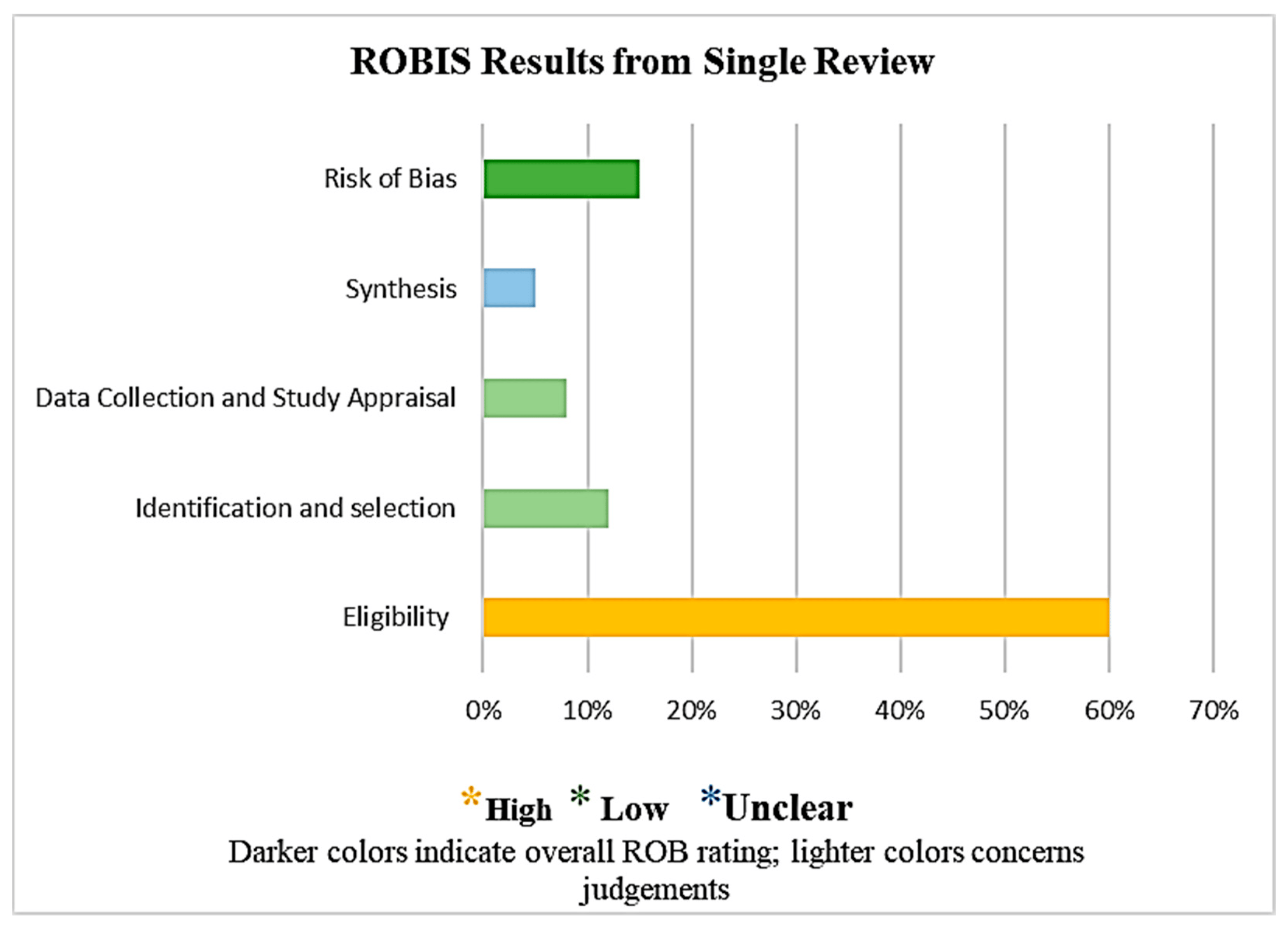
Figure 1. ROBIS results.
2.7. Risk of Bias–Assessment Tool
ROBIS (Risk of Bias in Systematic Reviews) criteria were also implemented to minimize the risk of bias to an extent because it assesses both the risk of bias in a review and (where appropriate) the relevance of a review to the research question. Identifying the scope, reviewing the evidence, holding a face-to-face meeting, and piloting the tool were the four stages comprising the design of ROBIS. Concern levels for each phase 2 domain and the proportion of reviews with high- or low-bias risk range from low to high or were unclear [29]. The use of signaling questions, when combined with a domain-based strategy, stand in line with the most recent techniques to generate the risk of bias tools, as shown in Figure 1. In order to resolve disagreements, the viewpoint of an additional reviewer was sought.
Figure 1 ROBIS findings from a single review are presented in the graphical format as follows: The final section (shaded darker) shows the risk of bias phase assessment. The colored segments show the concerns for each phase 2 ROBIS domain.
Furthermore, the risk assessment was performed by two reviewers based on the study objective, study design, study outcomes, justification by results, study limitations, ethical approval, informed consent from participants, funding, and relevance to this study. The third reviewer’s opinion was also taken to reduce the risk of bias. Risk analysis was performed for the studies included in this review. The reviewer’s risk concerns were low for this study’s objective, low for its relevance to this study, unclear for its limitations, high for funding, unclear for its design and outcomes, and low for its findings, conclusions, ethical approval, and informed consent.
A few concerns were identified with the review process for the phase 2 domain, as shown in the tables below. Concerns of the reviewers range between low, high, and unclear risks, whereas symbols such as Y/PY/PN/N/NI stand for Yes, Probably Yes, Probably No, No, and No information, respectively [29].
Phase 1. Assessing relevance [30].
Phase 2. Identifying concerns with the review process [30].
3. Results
Study Selection
At first, 17,000 results were yielded, upon which search filters such as year of publication, the field of expertise, and article type were applied. The search for publications concerning respectful maternity care in low- and middle-income countries and their comparison or effect of income on maternity care yielded 6000 papers, from which 5300 results were extracted for various reasons, and 700 studies were selected as discussed in Figure 2. However, two relevant articles were separated for future reference. The review articles were further analyzed to ensure they were pertinent to assessing the impact of income on maternity care. Around 215 references were examined for their potential applicability to the medical field of obstetric-led or maternity care. A total of 24 articles were included, with preference given to those published during the last 14 years, from 2010 to 2023. Figure 2 illustrates the PRISMA 2023 article identification flowchart, displaying this systematic review’s many stages in identifying studies.
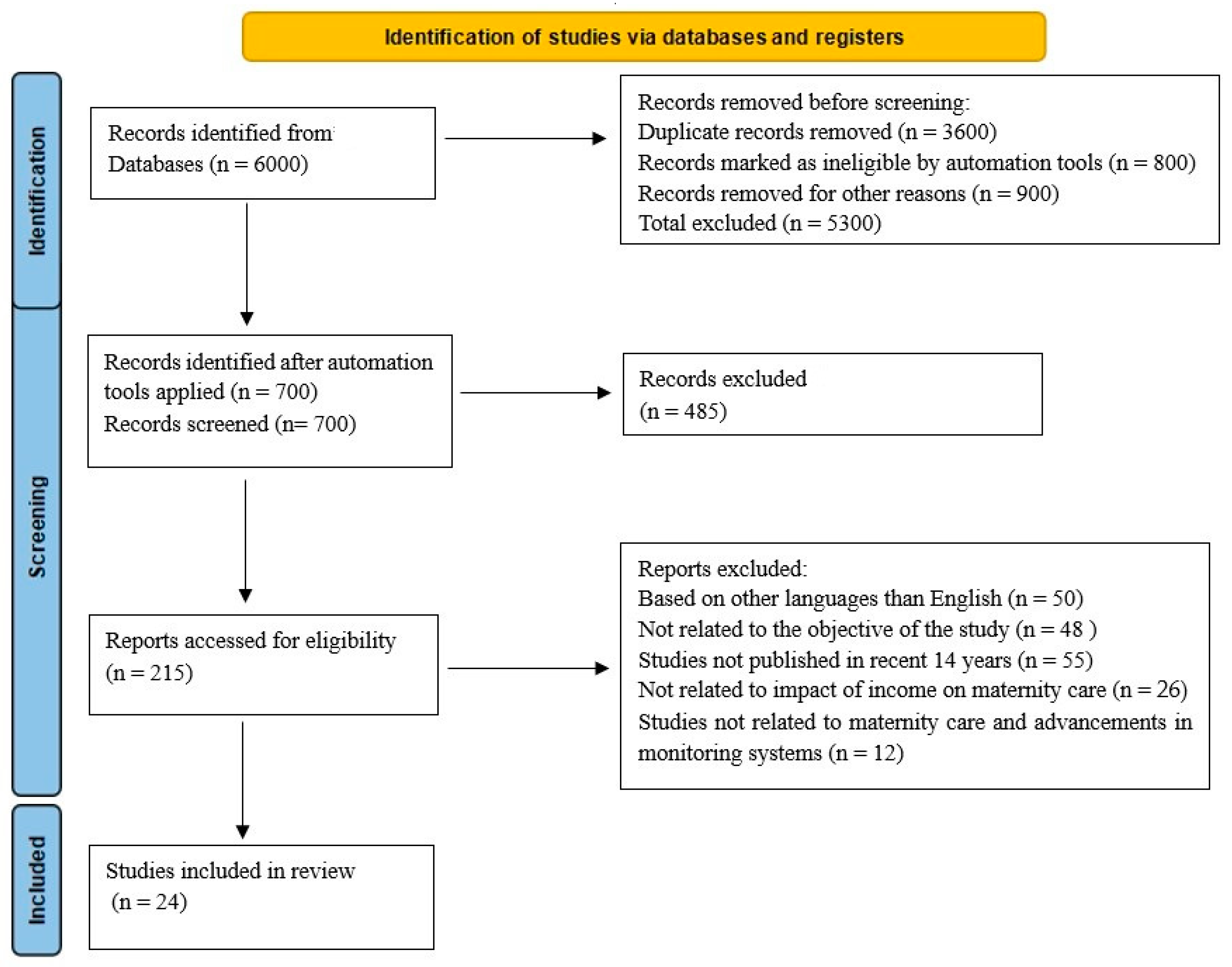
Figure 2. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
It comprises the flowchart for the studies that were reviewed. A search of the reviewed literature resulted in 6000 articles, with 5300 duplicates being removed. A total of 700 records were identified after automation tools were used, from which 485 articles were excluded after screening the titles and abstract. There were 215 reports accessed for eligibility. Based on languages other than English, 50 studies were excluded. Moreover, 141 studies were removed for other reasons, leaving 24 eligible studies for inclusion.
It indicates the strategies involved in systematic review writing. Research study types include systematic reviews. By integrating the findings from all previous scientific studies, a study aims to respond to a particular research question. This offers evidence that is more convincing and reliable than the findings of individual investigations. When performing systematic reviews, the objective is to analyze the thorough, systematic, exact, and clear literature. Additionally, a method based on and modified from Cochrane’s method was employed, as shown in Figure 3. These 15 steps are essential for effectively determining the concept and objective of the research topic. The details of findings from the studies are described as follows:
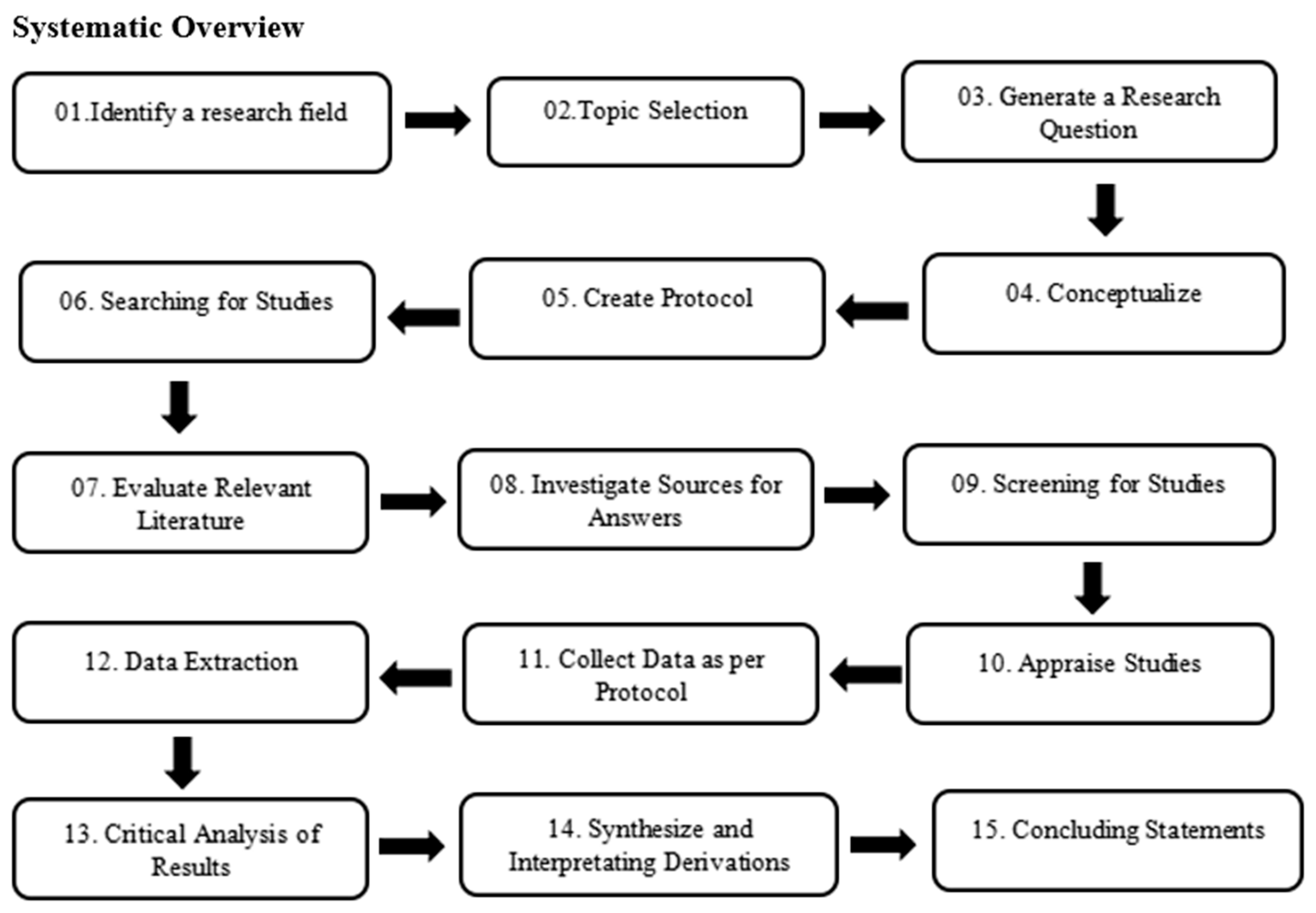
Figure 3. Flow diagram of strategies of systematic overview.
A total of 81.2% pregnant women received respectful care overall. Age of mothers [AOR = 2.54; 95% CI(1.01–6.43)]; prenatal care follow-ups (AOR = 2.86; 95% CI (1.01–8.20); and maternal occupation (AOR = 5.23; 95% CI (1.15–23.72)). The most important elements of respectful maternity care were found to be conversations with the provider concerning the place of delivery during the antenatal care follow-up [AOR = 5.58; 95% CI: (2.12–14.70)] [31]. From the RMC categories, 76.5% of the women are shielded from physical harm/ill treatment, and 89.2% received fair care devoid of prejudice. The right of women to knowledge, informed consent, and preference protection was upheld in only 39.3% of cases. Birthing at a medical facility (AOR:5.44), discussion of the delivery location (AOR:4.42), daytime delivery (AOR:5.56), longer length of stay (13 h) (AOR:2.10), and delivery time (AOR:2.10). Participation in decision making (AOR: 8.24), obtaining consent prior to the surgery (AOR: 3.45), unplanned pregnancy at the moment (AOR:5.56), three healthcare professionals present during labor (AOR:2.23), and satisfied with the length of time it took to be seen (AOR:2.08) [13]. The continuum of care (CoC) completion rate is low in this study’s site. Only 8.0% of the population had completed CoC. The biggest void, which contributed to the poor CoC, was found between delivery and postnatal care within 48 h after delivery. At six weeks after giving birth, 95% of women had received postnatal care and at least four prenatal visits. A total of 25% of women had postnatal care within 48 h, and 75% had competent assistance with delivery [32]. South Asia shows a decline in service use as women move along the care continuum from pregnancy to childbirth [33]. From “adequate antenatal care” to “adequate delivery care” (0.32) and “adequate child’s immunization” (0.36); from “adequate delivery care” to “adequate postnatal care” (0.78) and “adequate child’s immunization” (0.15)—all along the continuum of care for MNCH—were positively associated and statistically significant at p 0.001. The only route association that was adversely associated and significant at p 0.001 was the one between “adequate postnatal care” and “adequate child’s immunization” [34]. Despite maternal health and human rights stakeholders’ agreed importance of achieving respectful, non-abusive birth care for all women, there has been a relative lack of formal research on this topic [35]. As natural childbirth ideologies attracted growing North American attention from the mid-1940s, many Canadians sought less-medicalized births [36]. No measure was sufficient to determine women’s experiences of disrespectful and respectful maternity care in low- and middle-income countries. New valid and reliable measures using rigorous approaches to the development of tools are required [37]. A total of 316 of the 321 sampled respondents took part in this study, representing a response rate of 98.4%. Respect and maltreatment were present in 78.2% of cases (95% CI: 73.5–83.2). Unconsented care (86.1%), non-dignified care (37.3%), lack of privacy (33.9%), physical abuse (21.5%), and neglectful care (13.3%) were the most frequent kinds of disrespect and abuse experienced by the mothers. Respect and abuse during facility-based childbirth were strongly correlated with the mothers’ work, an increase in antenatal care visits, and giving birth in a hospital. According to an objective assessment, almost all women (99.7%) experienced D and A during labor. However, only 27.2% of respondents “reported D & A” in terms of their subjective experiences. Facility-based childbirth (OR = 13.49; 10.10–100.16) and lower socioeconomic strata (OR = 2.89; 1.63–5.11) were the primary predictors of reported D and A. In comparison to private health institutions, the chance of reporting D and A was twice as high in public facilities. Women who had previously reported D and A were more likely to choose to give birth somewhere different the second time around (OR = 4.37, 95% CI = 2.41–7.90) [38]. The mean score for respectful maternity care was 62.58, with a range of 15 to 75, while the average score for the entire delivery experience was 3.29, with a range of 1 to 4. A statistically significant direct link between respectful maternity care and a satisfying birthing experience was discovered after accounting for sociodemographic and obstetrical factors (p 0.001) [39]. Only 39.4% of women (95% confidence interval: 35.4–43.2) received considerate maternity care, according to this study. Having a high school diploma (adjusted odds ratio 2.47, 95% confidence interval: 1.35–4.50), and receiving follow-up prenatal care adjusted the odds that the pregnancy that was intended (adjusted odds ratio: 3.21, 95% confidence interval: 0.098, 0.03–0.34). Daytime delivery (adjusted odds ratio: 0.47, 95% confidence interval: 0.25–0.89), cesarean section (adjusted odds ratio: 0.69–6.08), and other factors. Respectful maternity care was substantially linked with (adjusted odds ratio: 1.9, 95% confidence interval: 1.33–2.72) [40]. Only 7% women had a negative birth experience. Moreover, factors related to unexpected medical problems were as follows: emergency operative delivery, induction, augmentation of labor, and infant transfer to neonatal care; related to the woman’s social life, such as unwanted pregnancy and lack of support from partner; related to the woman’s feelings during labor, such as pain and lack of control; and related to easier to influence by the caregivers [28]. The proportion of women who had respectful maternity care as a whole was 56.3%. An adjusted odds ratios (AOR) of 2.53 (95% CI: 1.094, 5.867), 2.46 (95% CI: 1.349, 4.482), and 3.092 (95% CI: 1.676, 5.725) for an antenatal care follow-up and above were found to be substantially linked with respectful maternity care [41]. Overall, it is encouraging to see that clinicians treated women with respect and care, yet many of them had unpleasant contacts with them and did not know much about their care. During this study, we saw women being abused verbally and physically. In the unstructured remarks, abandonment and neglect were the forms of disrespect and abuse that were most frequently cited. Except for the Tanzania mainland survey, which had a more evenly distributed mix of facilities with health centers and clinics. Observations were conducted predominantly at hospitals in all countries (80% of deliveries or greater were at hospitals) [42].
4. Discussion
4.1. Respectful Maternity Care
Respectful maternity care (RMC) is a term that recognizes that safe motherhood needs to extend beyond preventing mortality or morbidity by including respect for women’s fundamental human rights, such as respect for their autonomy, dignity, feelings, choices, and preferences, and such as having a companion as often as possible [43]. The United States Agency for International Development (USAID) adopted a three-pronged strategy of advocacy, study, and support for the implementation in awareness of the significance of this issue. The Maternal and Child Health Integrated Program (MCHIP) has prioritized funding for field-level implementation, while the White Ribbon Alliance and the Translating Research into Action (TRAction) initiative have concentrated on RMC advocacy and research, respectively [33]. In this instance, MCHIP performed the RMC survey to gain more from significant stakeholders about their experiences implementing interventions to promote RMC. A survey about disrespectful treatment and abuse in maternity care, methods for prevention, and strategies for promoting RMC received responses from a convenience group of 48 people from 19 different nations [43].
4.2. Respectful Maternity Care Method
The RMC method is individual-focused and founded on moral values and regard for human rights. The White Ribbon Alliance and RMC partners created the Respectful Maternity Care Charter as a reaction to the increasing body of evidence demonstrating disrespect and abuse of childbearing women. It is based on a framework of human rights [43]. Inadequate treatment at all stages has been associated with poor maternal and newborn health outcomes. Disparities in low- and middle-income countries (LMICs) continue to be substantial despite improvements in reproductive, maternal, newborn, and pediatric health [13]. For example, only 14% of women in Sub-Saharan Africa experienced every medical procedure, including at least one antenatal care (ANC), four or more ANC, childbirth with the assistance of a trained birth attendant, a postnatal check (PNC) within 24 h, and family planning assistance within a year of giving birth [13].
4.3. Disrespectful and Abusive Childbirth Medical Care
Additionally, throughout the world, women endured disrespectful and abusive childbirth medical care [37]. Consequently, in another study, Freedman et al. 2014 described that respectful and abusive care are interactions or facility conditions that are locally or culturally agreed to be experienced as humiliating or undignified [40]. Physical abuse, non-consent, discrimination, abandonment, and detention in health institutions are all examples of disrespectful and obnoxious treatment in a medical facility [35]. Disrespectful and abusive childbirth care can additionally lead to mental health issues such as childbirth fear, diminished sexuality, post-traumatic stress disorder, and postnatal depression [41]. Even in high-income countries, disrespectful and abusive behavior is not uncommon [36]. However, in middle- to low-income countries (LMICs), where gender inequality is even more severe, it tends to be more prevalent and obvious [44].
4.4. Measures to Ensure Respectful Maternity Care in LMIC
The experience of a woman, which is fundamental to RMC, is greatly influenced by the interpersonal interactions with those who are giving medical care or, to put it another way, by a set of behaviors of the providers [45]. The facility’s characteristics and the system the woman interacts with, including the culture, inevitably impact these behaviors [45]. It has been proposed that implementation science frameworks help create behavior change interventions because they can help create a structure for identifying the targets for a program and developing and testing programs that specifically target embedded constructs [45]. However, most RMC interventions do not base their intervention methods on implementation science or behavior change frameworks [38]. Interestingly, most maternal health initiatives do not employ implementation science frameworks, which could aid in the spread of evidence-based practices [45].
4.5. Medical Procedures Enhancing RMC
The World Health Organization (WHO) has identified respectful maternity care (RMC) as a fundamental human right since it affects both the mother’s and the child’s health [46,47]. Measures for care or medical procedures that can enhance respectful maternity care include
Finally, it can be summarized that by establishing quality development teams, keeping track of incidents of poor treatment, providing mentorship, and improving staff working conditions, health facilities may establish enabling environments. Health facilities and health systems must be set up to support and respect practitioners and ensure sufficient infrastructure and maternity ward structure to provide respectful care to pregnant women [2]. Following these measures, maternity care can be made respectful in low- and middle-income countries.
4.6. Rules of Ethics and Respectful Maternity Care
In order to encourage active participation by professional associations, governments, non-governmental organizations, and civil society in improving quality of care and reducing abuse, neglect, and extortion of childbearing women in facilities, the International Federation of Gynecology and Obstetrics (FIGO) launched the International Childbirth Initiative in cooperation with colleagues from the International Confederation of Midwives, White Ribbon Alliance, the International Paediatrics Association, and the World Health Organization (WHO). Abuse of women, their newborns, and their families, whether physical, verbal, or emotional, is never permitted. Transparent pricing and free or inexpensive healthcare should be provided. Along the whole parenting spectrum, respect each woman’s right to nondiscriminatory, free, or cheap care Respectful maternity care (RMC) is a strategy that places an emphasis on the person, is founded on moral values and respect for human rights, and encourages behaviors that take women’s preferences into account, as well as their needs and those of their unborn children [51,52,53].
4.7. Data Analysis
The topics covered in the articles and the developed template aligned with this review’s goal and were used to summarize the general characteristics of the included studies. The template included categories for the title, authors, publishing year, reference number, and conclusions of the included studies. In this repetitive process, literature from the included studies was reviewed, annotated, highlighted, and evaluated. Detailed systematic review is shown in .
5. Conclusions
Concluding this study’s findings, it can be estimated that there is a direct association between income and maternity care. In lower- and middle-income countries, maternity care is substandard compared to high-income countries. Moreover, it is determined that the evidence for medical procedures that can enhance respectful maternity care is sparse. Potential growth of providers’ skills has included transforming attitudes, training on values, and interpersonal communication. Enabling environments can be established within a health facility by establishing quality improvement teams, monitoring poor treatment experiences, mentorship, and improving working circumstances for staff. To provide respectful care, health systems and health facilities must be organized to support and respect clinicians while ensuring sufficient infrastructure and maternity ward organization. Finally, it can be stated that respectful maternity care is a fundamental element of high-quality care and a human right.
6. Limitations
This review may have some limitations.
7. Strengths
8. Research Gap
This review acknowledges the limited evidence and research gaps in interventions to enhance respectful maternity care. By identifying these gaps, this study highlights the need for further research and contributes to advancing knowledge in this area.
9. Novelty of Research
The research focuses on respectful maternity care in low-income countries (LMICs) and its implementation, highlighting the limited evidence and understanding of this concept. It identifies gaps, challenges, and potential strategies for promoting respectful maternity care in LMICs. This review emphasizes the need for further research to evaluate interventions, assess effectiveness, and understand their impact on maternal and neonatal health outcomes. This research acknowledges the limited risk of bias in studies and emphasizes the importance of context-specific approaches and methodological rigor in future studies.
10. Future Research Directions
Future research directions for respectful maternity care in LMICs include intervention studies, implementation strategies, health system integration, measurement and evaluation, cultural sensitivity, equity and social determinants, and longitudinal studies. These will contribute to the evidence base, inform policy, and improve the provision of respectful maternity care, leading to better maternal and neonatal health outcomes and enhanced patient experiences.
References
- Cranfield, K.; Horner, D.; Vasco, M.; Victory, G.; Lucas, D. Current perspectives on maternity critical care. Anaesthesia 2023, 78, 758–769. [Google Scholar] [CrossRef] [PubMed]
- Bohren, M.A.; Tunçalp, Ö.; Miller, S. Transforming intrapartum care: Respectful maternity care. Best Pract. Res. Clin. Obstet. Gynaecol. 2020, 67, 113–126. [Google Scholar] [CrossRef] [PubMed]
- Caroline, S.E.; Homer, M.A.B.; Wilson, A.; Vogel, J.P. Elements of Professional Care and Support Before, during and after Pregnancy (Achieving Inclusive and Respectful Maternity Care); Glown: London, UK, 2021; Volume 3. [Google Scholar]
- Simkin, P. The experience of maternity in a woman’s life. J. Obstet. Gynecol. Neonatal Nurs. 1996, 25, 247–252. [Google Scholar] [CrossRef] [PubMed]
- UN, Office of the High Commissioner for Human Rights. Technical Guidance on the Application of a Human Rights-Based Approach to the Implementation of Policies and Programmes to Reduce Preventable Maternal Mortality and Morbidity: Report of the Office of the United Nations High Commissioner for Human Rights (No. (A/HRC/21/22)); UN, Office of the High Commissioner for Human Rights: Geneva, Switzerland, 2012. [Google Scholar]
- Respectful Maternity Care Charter Assets. Available online: https://whiteribbonalliance.org/resources/rmc-charter/ (accessed on 3 March 2023).
- ten Hoope-Bender, P.; de Bernis, L.; Campbell, J.; Downe, S.; Fauveau, V.; Fogstad, H.; Homer, C.S.; Kennedy, H.P.; Matthews, Z.; McFadden, A. Improvement of maternal and newborn health through midwifery. Lancet 2014, 384, 1226–1235. [Google Scholar] [CrossRef]
- Renfrew, M.J.; McFadden, A.; Bastos, M.H.; Campbell, J.; Channon, A.A.; Cheung, N.F.; Silva, D.R.A.D.; Downe, S.; Kennedy, H.P.; McCormick, F. Midwifery and quality care: Findings from a new evidence-informed framework for maternal and newborn care. Lancet 2014, 384, 1129–1145. [Google Scholar] [CrossRef]
- Jansen, L.; Gibson, M.; Bowles, B.C.; Leach, J. First do no harm: Interventions during childbirth. J. Perinat. Educ. 2013, 22, 83–92. [Google Scholar] [CrossRef]
- Quinn, A.C.W.; Masterson, G.; Gauntlett, R.; Banerjee, A.; Quinn, A.; Litchfield, K. Care of the Critically Ill Woman in Childbirth; Enhanced Maternal Care; Royal College of Obstericians & Gynaecologists: London, UK, 2018. [Google Scholar]
- Sakala, C.; Corry, M.P.; Childbirth Connection; The Reforming States Group; Milbank Memorial Fund. Evidence-Based Maternity Care: What It Is and What It Can Achieve; Milbank Memorial Fund: New York, NY, USA, 2008. [Google Scholar]
- Miller, S.; Abalos, E.; Chamillard, M.; Ciapponi, A.; Colaci, D.; Comandé, D.; Diaz, V.; Geller, S.; Hanson, C.; Langer, A. Beyond too little, too late and too much, too soon: A pathway towards evidence-based, respectful maternity care worldwide. Lancet 2016, 388, 2176–2192. [Google Scholar] [CrossRef]
- Kitila, S.B.; Feyissa, G.T.; Olika, A.K.; Wordofa, M.A. Maternal Healthcare in Low- and Middle-Income Countries: A Scoping Review. Health Serv. Insights 2022, 15, 11786329221100310. [Google Scholar] [CrossRef]
- Kim, M.K.; Lee, S.M.; Bae, S.-H.; Kim, H.J.; Lim, N.G.; Yoon, S.-J.; Lee, J.Y.; Jo, M.-W. Socioeconomic status can affect pregnancy outcomes and complications, even with a universal healthcare system. Int. J. Equity Health 2018, 17, 2. [Google Scholar] [CrossRef]
- Bo, S.; Menato, G.; Bardelli, C.; Lezo, A.; Signorile, A.; Repetti, E.; Massobrio, M.; Pagano, G.F. Low socioeconomic status as a risk factor for gestational diabetes. Diabetes Metab. 2002, 28, 139–140. [Google Scholar]
- Benova, L.; Tunçalp, Ö.; Moran, A.C.; Campbell, O.M.R. Not just a number: Examining coverage and content of antenatal care in low-income and middle-income countries. BMJ Glob. Health 2018, 3, e000779. [Google Scholar] [CrossRef] [PubMed]
- Syed, U.; Kinney, M.V.; Pestvenidze, E.; Vandy, A.O.; Slowing, K.; Kayita, J.; Lewis, A.F.; Kenneh, S.; Moses, F.L.; Aabroo, A. Advancing maternal and perinatal health in low-and middle-income countries: A multi-country review of policies and programmes. Front. Glob. Women’s Health 2022, 3, 909991. [Google Scholar] [CrossRef] [PubMed]
- Gage, A.D.; Carnes, F.; Blossom, J.; Aluvaala, J.; Amatya, A.; Mahat, K.; Malata, A.; Roder-DeWan, S.; Twum-Danso, N.; Yahya, T. In low-and middle-income countries, is delivery in high-quality obstetric facilities geographically feasible? Health Aff. 2019, 38, 1576–1584. [Google Scholar] [CrossRef] [PubMed]
- Larson, C.P. Poverty during pregnancy: Its effects on child health outcomes. Paediatr Child Health 2007, 12, 673–677. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, R.L.; McClure, E.M.; Saleem, S. Improving pregnancy outcomes in low-and middle-income countries. Reprod. Health 2018, 15, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Bauserman, M.; Lokangaka, A.; Thorsten, V.; Tshefu, A.; Goudar, S.; Esamai, F. Risk factors for maternal death in low-and middle-income countries: A prospective longitudinal cohort analysis. Reprod. Health 2015, 12, 1–9. [Google Scholar] [CrossRef]
- Castro, A. Witnessing obstetric violence during fieldwork: Notes from Latin America. Health Hum. Rights 2019, 21, 103. [Google Scholar]
- Dickinson, F.M.; Madaj, B.; Muchemi, O.M.; Ameh, C. Assessing quality of care in maternity services in low and middle-income countries: Development of a Maternity Patient Reported Outcome Measure. PLoS Glob. Public Health 2022, 2, e0000062. [Google Scholar] [CrossRef]
- WHO. Ending Preventable Maternal Mortality (EPMM): A Renewed Focus for Improving Maternal and Newborn Health and Well-Being; WHO: Geneva, Switzerland, 2021.
- WHO. Every Newborn: An Action Plan to End Preventable Deaths; WHO: Geneva, Switzerland, 2014.
- Graham, W.; Woodd, S.; Byass, P.; Filippi, V.; Gon, G.; Virgo, S.; Chou, D.; Hounton, S.; Lozano, R.; Pattinson, R. Diversity and divergence: The dynamic burden of poor maternal health. Lancet 2016, 388, 2164–2175. [Google Scholar] [CrossRef]
- Wood, W. ‘Put Right Under’: Obstetric Violence in Post-war Canada. Soc. Hist. Med. 2018, 31, 796–817. [Google Scholar] [CrossRef]
- Schroll, A.-M.; Kjærgaard, H.; Midtgaard, J. Encountering abuse in health care; lifetime experiences in postnatal women-a qualitative study. BMC Pregnancy Childbirth 2013, 13, 74. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.; Savović, J.; Higgins, J.P.T.; Caldwell, D.M.; Reeves, B.C.; Shea, B.; Davies, P.; Kleijnen, J.; Churchill, R. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J. Clin. Epidemiol. 2016, 69, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Penny Whiting, J.S.; Higgins, J.; Caldwell, D.; Reeves, B.; Shea, B.; Davies, P.; Kleijnen, J.; Churchill, R. ROBIS: Tool to Assess Risk of Bias in Systematic Reviews. In Guidance on How to Use ROBIS; NCCMT: Hamilton, ON, Canada, 2016; pp. 1–39. Available online: https://www.bristol.ac.uk/media-library/sites/social-community-medicine/robis/robisguidancedocument.pdf (accessed on 3 March 2023).
- Adugna, A.; Kindie, K.; Abebe, G.F. Respectful maternity care and associated factors among mothers who gave birth in three hospitals of Southwest Ethiopia: A cross-sectional study. Front. Public Health 2023, 10, 1055898. [Google Scholar] [CrossRef] [PubMed]
- Bulto, G.A.; Demissie, D.B.; Tulu, A.S. Respectful maternity care during labor and childbirth and associated factors among women who gave birth at health institutions in the West Shewa zone, Oromia region, Central Ethiopia. BMC Pregnancy Childbirth 2020, 20, 443. [Google Scholar] [CrossRef]
- Mohan, D.; E LeFevre, A.; George, A.; Mpembeni, R.; Bazant, E.; Rusibamayila, N.; Killewo, J.; Winch, P.J.; Baqui, A.H. Analysis of dropout across the continuum of maternal health care in Tanzania: Findings from a cross-sectional household survey. Health Policy Plan. 2017, 32, 791–799. [Google Scholar] [CrossRef]
- Yeji, F.; Shibanuma, A.; Oduro, A.; Debpuur, C.; Kikuchi, K.; Owusu-Agei, S.; Gyapong, M.; Okawa, S.; Ansah, E.; Asare, G.Q.; et al. Continuum of care in a maternal, newborn and child health program in ghana: Low completion rate and multiple obstacle factors. PLoS ONE 2015, 10, e0142849. [Google Scholar] [CrossRef]
- Alva, S.; Wang, W.; Koblinsky, M. The continuum of care for maternal and newborn health in south Asia: Determining the gap and its implications. In Proceedings of the Annual Meeting of the Population Association of America, Washington, DC, USA, 31 March–2 April 2011. [Google Scholar]
- Owili, P.O.; Muga, M.A.; Chou, Y.J.; Hsu, Y.H.E.; Huang, N.; Chien, L.Y. Associations in the continuum of care for maternal, newborn and child health: A population-based study of 12 sub-Saharan Africa countries. BMC Public Health 2016, 16, 414. [Google Scholar]
- Mgawadere, F.; Shuaibu, U. Enablers and barriers to respectful maternity care in low and middle-income countries: A literature review of qualitative research. Int. J. Clin. Med. 2021, 12, 224–249. [Google Scholar] [CrossRef]
- Azhar, Z.; Oyebode, O.; Masud, H. Disrespect and abuse during childbirth in district Gujrat, Pakistan: A quest for respectful maternity care. PLoS ONE 2018, 13, e0200318. [Google Scholar] [CrossRef]
- Hajizadeh, K.; Vaezi, M.; Meedya, S.; Mohammad Alizadeh Charandabi, S.; Mirghafourvand, M. Respectful maternity care and its relationship with childbirth experience in Iranian women: A prospective cohort study. BMC Pregnancy Childbirth 2020, 20, 468. [Google Scholar] [CrossRef]
- Ferede, W.Y.; Gudayu, T.W.; Gessesse, D.N.; Erega, B.B. Respectful maternity care and associated factors among mothers who gave birth at public health institutions in South Gondar Zone, Northwest Ethiopia 2021. Womens Health 2022, 18, 17455057221116505. [Google Scholar] [CrossRef] [PubMed]
- Yosef, A.; Kebede, A.; Worku, N. Respectful Maternity Care and Associated Factors Among Women Who Attended Delivery Services in Referral Hospitals in Northwest Amhara, Ethiopia: A Cross-Sectional Study. J. Multidiscip. Healthc. 2020, 13, 1965–1973. [Google Scholar] [CrossRef] [PubMed]
- Rosen, H.E.; Lynam, P.F.; Carr, C.; Reis, V.; Ricca, J.; Bazant, E.S.; Bartlett, L.A.; Quality of Maternal and Newborn Care Study Group of the Maternal and Child Health Integrated Program. Direct observation of respectful maternity care in five countries: A cross-sectional study of health facilities in East and Southern Africa. BMC Pregnancy Childbirth 2015, 15, 306. [Google Scholar] [CrossRef] [PubMed]
- Bekele, W.; Bayou, N.B.; Garedew, M.G. Magnitude of disrespectful and abusive care among women during facility-based childbirth in Shambu town, Horro Guduru Wollega zone, Ethiopia. Midwifery 2020, 83, 102629. [Google Scholar] [CrossRef]
- Diamond-Smith, N.; Walker, D.; Afulani, P.A.; Donnay, F.; Peca, E.; Stanton, M.E. The Case for Using a Behavior Change Model to Design Interventions to Promote Respectful Maternal Care. Glob. Health Sci. Pract. 2023, 11, e2200278. [Google Scholar] [CrossRef]
- Dhakal, P.; Gamble, J.; Creedy, D.K.; Newnham, E. Quality of measures on respectful and disrespectful maternity care: A systematic review. Nurs. Health Sci. 2021, 23, 29–39. [Google Scholar] [CrossRef]
- Adeyemo, A.C. Respectful Maternity Care: Fundamental Human Right in Labour and Delivery. Int. J. Med. Nurs. Health Sci. 2022, 3, 36–47. [Google Scholar] [CrossRef]
- Palet-Rodríguez, M.; Torrubia-Pérez, E. The usefulness of complementary therapies in pain management during childbirth: An integrative review. Enfermería Glob. 2023, 70, 481. [Google Scholar]
- Smith, P.B. Social determinants of health and their relationships to reproductive outcomes. Bull. Menn. Clin. 2023, 87, 189–208. [Google Scholar] [CrossRef]
- Frayne, J.; Ellies, R.; Nguyen, T. Experiences of decision making about psychotropic medication during pregnancy and breastfeeding in women living with severe mental illness: A qualitative study. Arch. Women’s Ment. Health 2023, 26, 379–387. [Google Scholar] [CrossRef]
- Maldie, M.; Egata, G.; Chanie, M.G.; Muche, A.; Dewau, R.; Worku, N.; Alemu, M.D.; Ewunetie, G.E.; Birhane, T.; Addisu, E.; et al. Magnitude and associated factors of disrespect and abusive care among laboring mothers at public health facilities in Borena District, South Wollo, Ethiopia. PLoS ONE 2021, 16, e0256951. [Google Scholar] [CrossRef] [PubMed]
- Freedman, L.P.; Ramsey, K.; Abuya, T.; Bellows, B.; Ndwiga, C.; Warren, C.E.; Kujawski, S.; Moyo, W.; Kruk, M.E.; Mbaruku, G. Defining disrespect and abuse of women in childbirth: A research, policy and rights agenda. Bull. World Health Organ. 2014, 92, 915–917. [Google Scholar] [CrossRef] [PubMed]
- Bowser, D.; Hill, K. Exploring Evidence for Disrespect and Abuse in Facility-Based Childbirth: Report of a Landscape Analysis; USAID-TRAction Project; University Research Co., LLC.: Chevy Chase, MD, USA, 2010. [Google Scholar]
- FIGO. Ethical Framework for Respectful Maternity Care During Pregnancy and Childbirth | Figo 2021. Available online: https://www.figo.org/resources/figo-statements/ethical-framework-respectful-maternity-care-during-pregnancy-and-childbirth (accessed on 9 September 2023).
- Lusambili, A.M.; Wisofschi, S.; Wade, T.J.; Temmerman, M.; Obure, J. A qualitative enquiry of health care workers’ narratives on knowledge and sources of information on principles of Respectful Maternity Care (RMC). PLoS Glob. Public Health 2023, 3, e0000157. [Google Scholar] [CrossRef] [PubMed]

