The patient is a 58-year-old man with a history of hypertension, diabetes mellitus complicated by neuropathy, and obesity (body mass index of 42 kg/m2) who presented for the evaluation of pain, edema, and numbness in the left hindfoot following a motor vehicle collision. Following the motor vehicle collision, the patient was referred to a podiatrist by his primary care physician for the treatment of pain. Conventional radiographic images at that time were read as negative. The patient experienced an exacerbation of pain in the same foot 8 months later when he felt a pop following a fall from standing. Following this exacerbation, the patient returned to his podiatrist and underwent 6 weeks of casting followed by a course of physical therapy. After these treatments failed to relieve the pain that the patient was experiencing, he underwent magnetic resonance imaging (MRI).
The MRI, per report, revealed diffuse bone marrow edema in the talus and navicular bones, an erosive irregularity at the talonavicular joint, and a large, multiloculated fluid collection. The radiologist included osteonecrosis, stress fractures, advanced erosive arthropathy, and infection in his differential diagnosis. The nuclear scan displayed a focal area of uptake in the anterior aspect of the talus and talar head. Moderate to severe degenerative changes were also noted in the hindfoot and midfoot joints with numerous subchondral cysts present. No fracture or midfoot collapse was noted.
After imaging, the patient was examined in an orthopaedic clinic. Here, he was diagnosed with Charcot arthropathy, and his symptoms were not relieved by a trial of ibuprofen and an air cast boot. Because of the patient’s insistence that his symptoms did not exist prior to his injury, he sought treatment with a foot and ankle specialist 19 months after the motor vehicle collision.
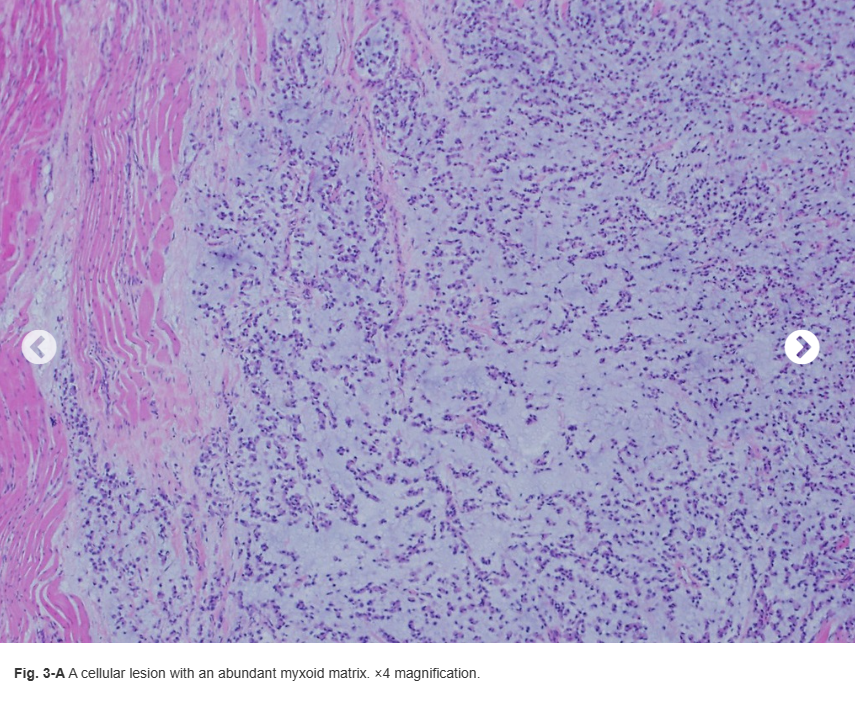
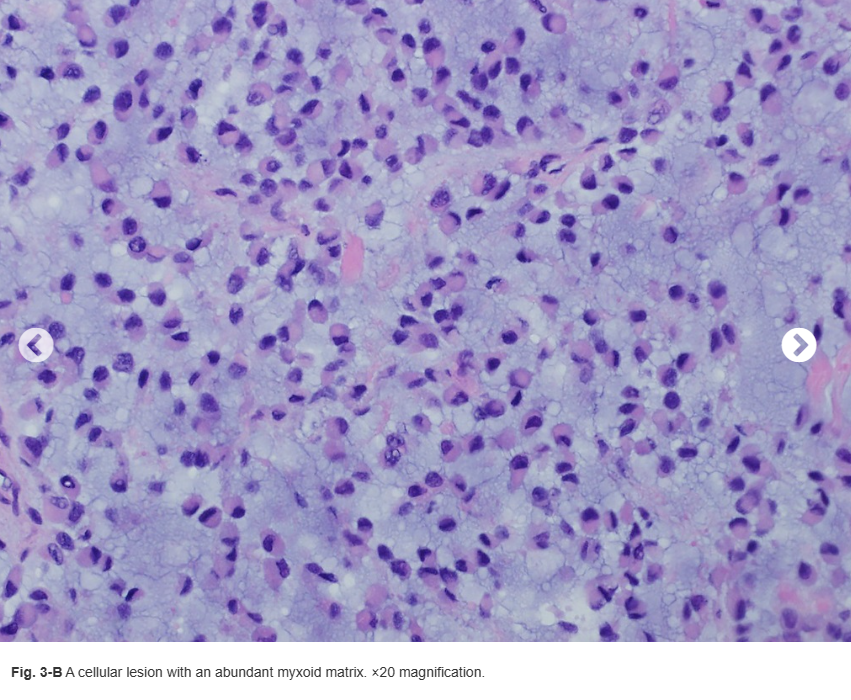
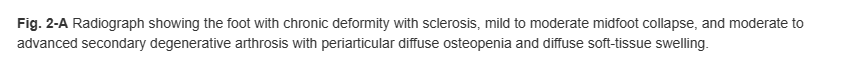
During his initial visit to the foot and ankle clinic, the patient reported numbness and pain over the anterior ankle and the medial and plantar surfaces of the foot. On physical examination, he was tender to palpation over the anterior ankle, lateral talonavicular joint, and sinus tarsi. He was also noted to have some mild edema of the dorsal foot. Radiographs revealed chronic-appearing deformity of the midfoot with some sclerotic changes of the osseous structures, midfoot sag, and advanced degenerative changes of the talonavicular, subtalar, and midfoot joints (Fig. 1).
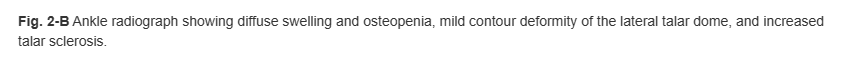
Because of the patient’s clinical picture and preexisting neuropathy, these radiographic findings were believed to be consistent with remote trauma and degenerative Charcot arthropathy. A new MRI of the foot and ankle without contrast was ordered to evaluate for osteonecrosis compared with talar edema, as osteonecrosis would prognosticate poorly for the success of future arthrodeses. Before MRI, potential surgical plans were discussed because of the midfoot degeneration including subtalar, talonavicular, naviculocuneiform, and first tarsometatarsal fusions. Additional imaging studies were obtained (Figs. 2-A and 2-B).
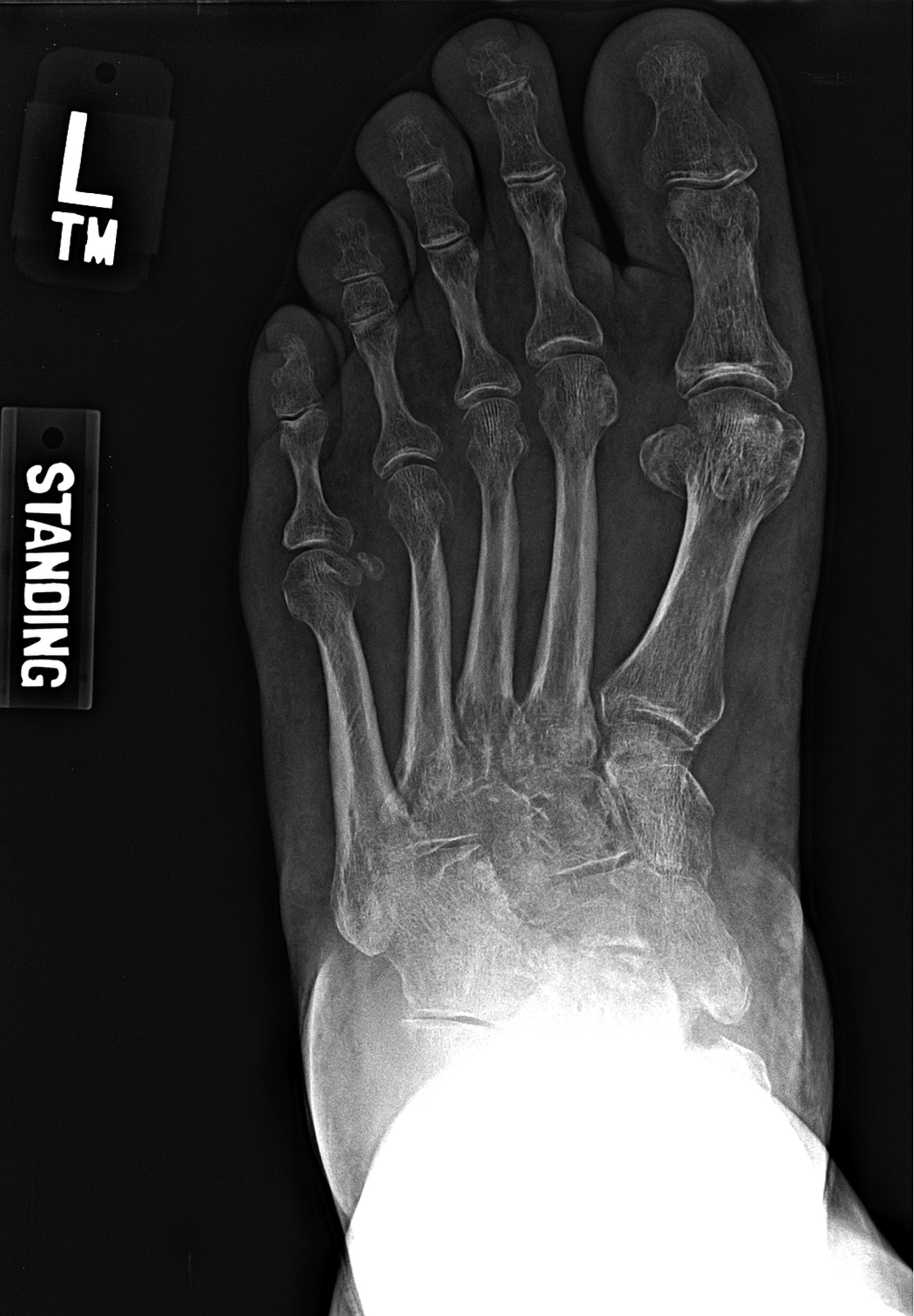

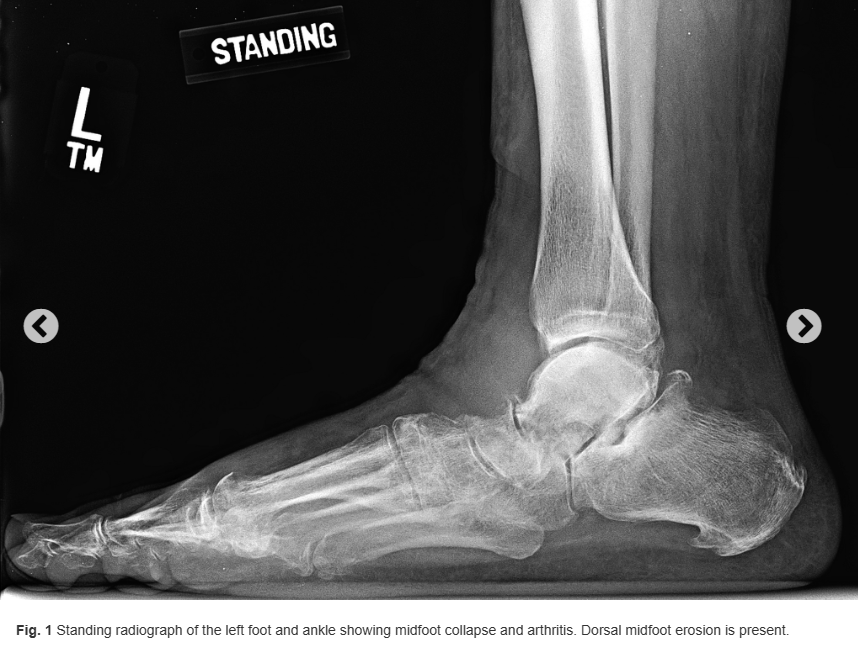
The MRI revealed a T2 hyperintense and T1 hypointense mass that appeared to have an epicenter in the soft tissue of the anterior ankle, contiguous with the talar neck and anterior talar dome. This mass extended from its origin, interdigitating in the syndesmosis, tibiotalar joint, subtalar joint, calcaneonavicular joint, and sinus tarsi. Erosive, invasive changes with associated bony edema and cortical discontinuity were noted in the talus, navicular, calcaneus, cuneiforms, and anterior distal part of the tibia. The patient was referred to an orthopaedic oncologist, who recommended ultrasound-guided core needle biopsy. Histology is shown in Figures 3-A and 3-B.