A 21-year-old healthy man presented with a 1-year history of persistent right plantar fasciitis despite nonoperative treatment for over a year. On physical examination, he was experiencing pain over the plantar medial heel and had a gastrocnemius contracture based on the Silfverskiöld test with maximum dorsiflexion of 0° with the knee extended and 20° with the knee flexed. The patient elected to undergo a gastrocnemius recession.
In the operating room, a thigh tourniquet was used, and the right lower extremity was prepped with chlorhexidine gluconate 2% wt/vol and isopropyl alcohol 70% vol/vol and was sterilely draped. A 4-cm incision was made over the posterior medial lower limb at the gastrocsoleus junction, and a standard Strayer procedure was performed. Adequate release was evident with the ankle obtaining 15° of dorsiflexion with the knee extended. The wound was irrigated with normal saline, the deep layer was closed with Vicryl, and the skin was closed with nylon sutures. Xeroform and sterile 4 × 4 bandages were applied over the wound, and the patient was placed in a plaster posterior splint and was instructed to be non-weight-bearing for 2 weeks.
The patient returned to the office on postoperative day 10 with reports of subjective fever and calf pain. He had no objective temperature on office assessment. His splint was removed, and mild erythema was noted around the wound. The skin edges were darkened, but this was thought to be due to the blue surgical marking pen. The patient was placed back in a splint, was given a 7-day oral cephalexin course, and was scheduled to return in 3 days for a wound check.
Two days later, the patient presented to the emergency department with increasing calf pain, and the area of darkness had expanded beyond the sutured edges (Fig. 1). Radiographs of the lower limb were normal, and there was no gas in the tissues based on the radiographs and the clinical examination for crepitus. He was afebrile and had a white blood cell count of 17,000/μL. Given the severity of the presentation of the wound despite clear etiology, the patient was taken to the operating room for surgical debridement and wound vacuum placement and was administered intravenous vancomycin and piperacillin with tazobactam. The area of necrosis surrounding the surgical wound was debrided, and there was no gross purulence, but the wound was soupy with brown discharge. Tissue samples were sent for Gram stain and culture and to the pathology department for microscopic evaluation.
The histology of the debrided tissue is shown in Figures 2-A and 2-B.

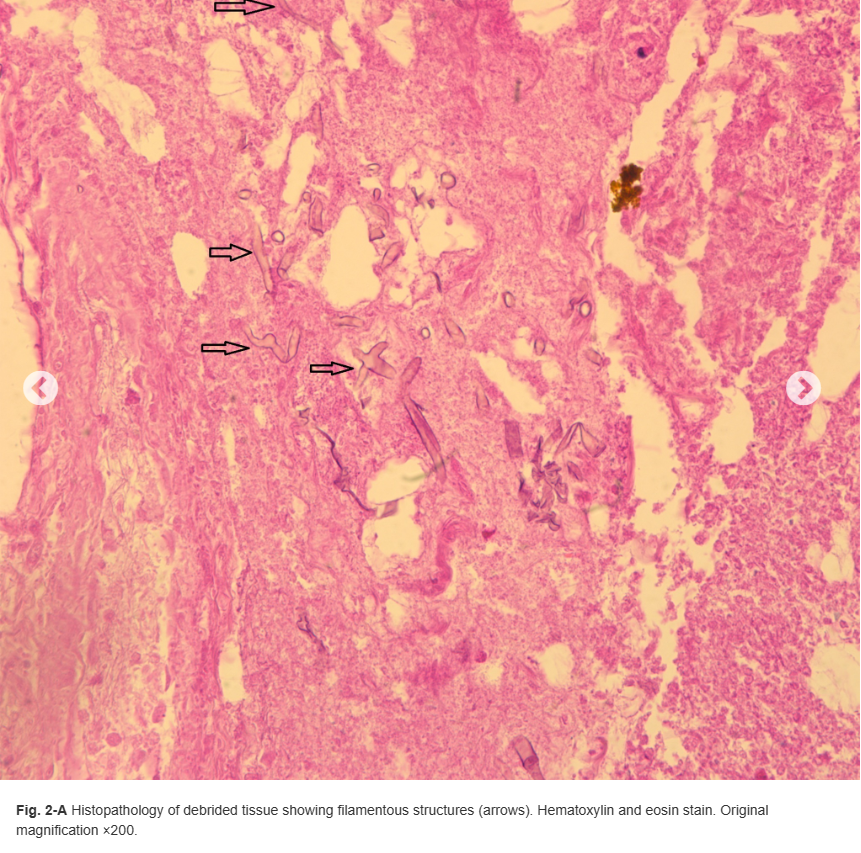
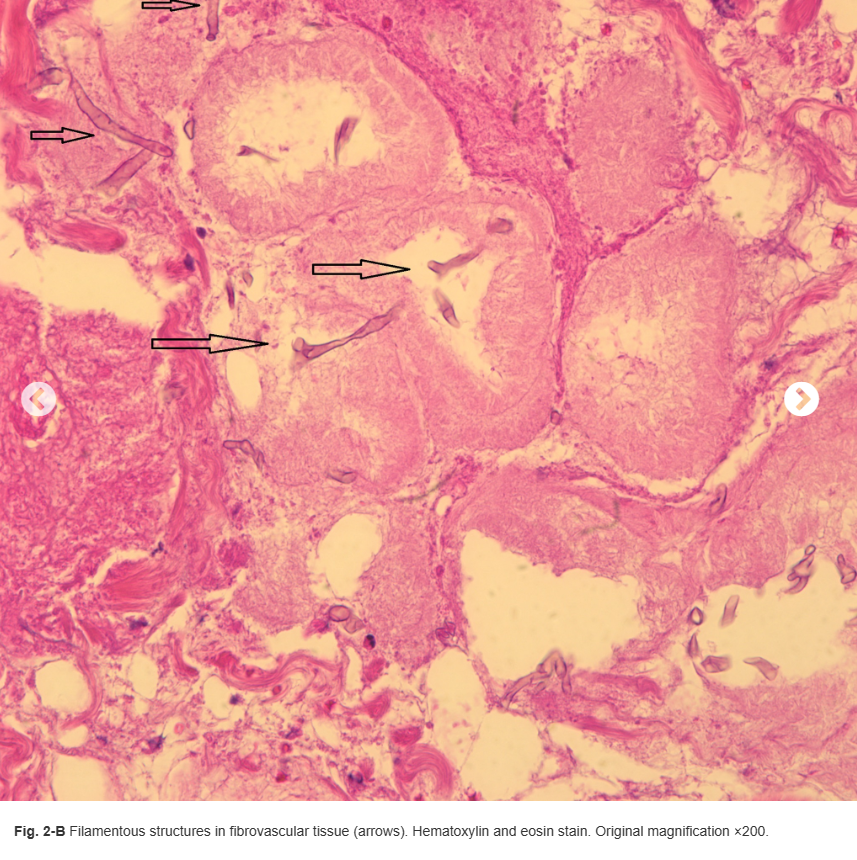
What is the diagnosis?

