A 69-year-old, right-hand-dominant woman presented 7 days after sustaining a closed right proximal humeral shaft fracture after a fall from height. Her medical history included myasthenia gravis and right rotator cuff arthropathy. She was a nonsmoker and a community ambulator requiring the use of a walker. She had no previous injuries, no relevant surgical history, and no previous neurological deficits of the right upper extremity. On presentation, she was neurovascularly intact with extensive swelling and ecchymoses of the arm. Radiographs demonstrated substantial displacement of the fracture (Figs. 1-A and 1-B).



The fixation of the fracture was performed 12 days after the injury. Before surgery, the patient was neurovascularly intact but had mild weakness with flexion at the right thumb interphalangeal joint along with persistent swelling of the arm. A standard starting point for intramedullary fixation of the humerus was used. On opening the humeral canal, 100 mL of blood was released, suggestive of a fracture hematoma. The hematoma was completely evacuated, and there was no sign of active arterial bleed. Because the patient had limited mobility of the shoulder, a Shantz pin on the distal fragment and a blunt bone hook on the proximal fragment were used to reduce the fracture via a small lateral incision. A Stryker proximal humeral nail size 8 × 240 mm was used. Postoperatively, she had intact sensation and motor function of the axillary, median, radial, and ulnar nerves as well as a palpable radial pulse.
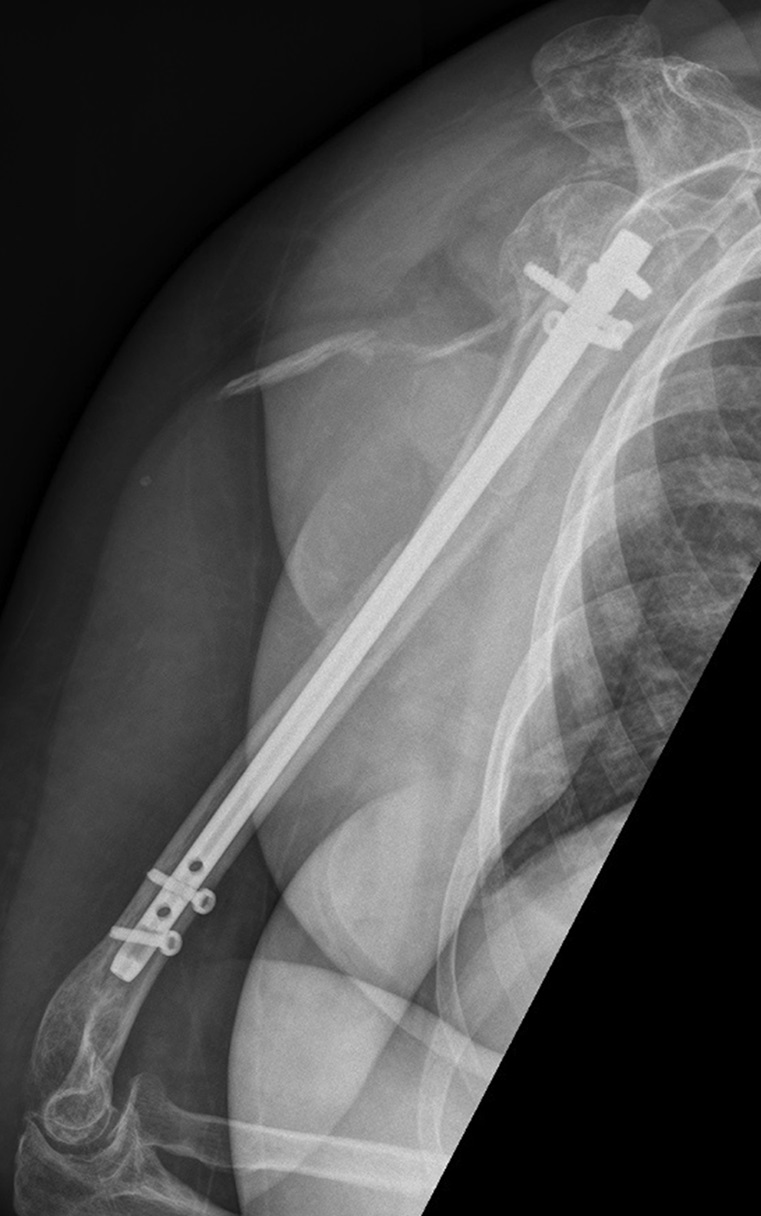
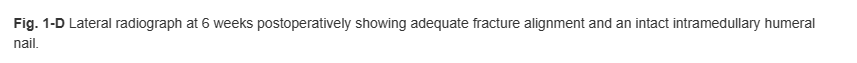
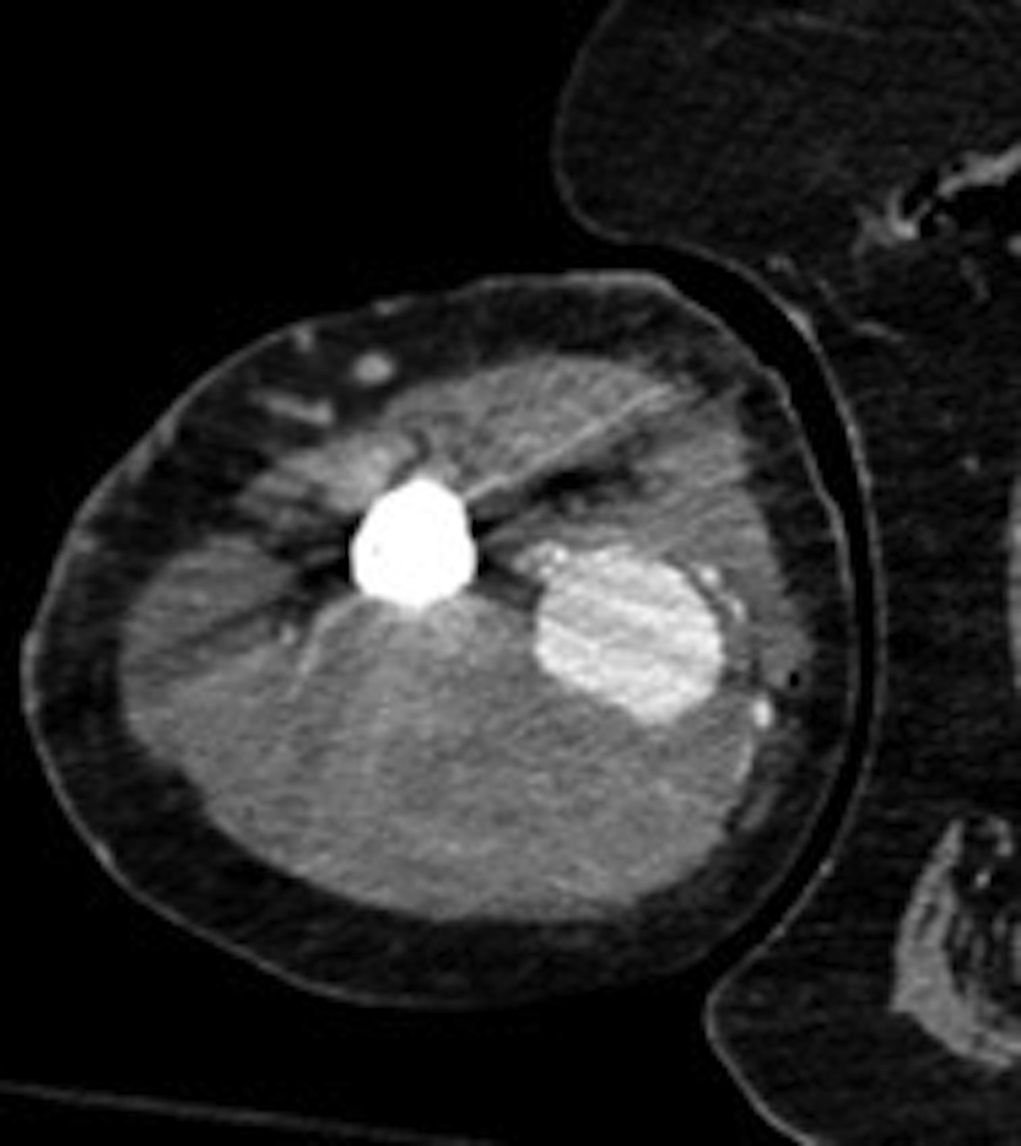
At her 6-week postoperative visit, the patient presented reporting progressive arm swelling, weakness, and loss of sensation in the right hand. Radiographs demonstrated interval healing of the previous fracture and appropriate position of the implant (Figs. 1-C and 1-D). She had a normal vascular examination but had no wrist flexion or extension and was 0/5 for her anterior interosseous and posterior interosseous nerve function. The only motor function that the patient retained was the ability to weakly flex the fourth and fifth digits, as well as active flexion and extension of the elbow. She had no sensation to light touch over the median, radial, and ulnar nerve distributions over the hand. Computed tomography (CT) without contrast of the right arm demonstrated a large compressive hematoma on the medial and posterior aspects of the right upper arm, which measured 71 × 94 mm (Fig. 2-A). CT angiogram was performed (Figs. 2-B through 2-D). Distally, the brachial, radial, and ulnar arteries were patent.







What is the diagnosis?

