A 64-year-old man with a 40-pack-year smoking history (he had stopped smoking 5 years earlier), hypertension, diabetes mellitus type II, hyperlipidemia, obesity, and pulmonary embolism was referred to our clinic for the evaluation of persistent medial left knee pain and an apparent periprosthetic fracture. He had undergone revision total knee arthroplasty (TKA) for aseptic loosening at another institution 4 months previously. Before referral, he underwent a workup for infection that included serum markers and fluoroscopically guided aspiration, reportedly within normal limits. However, the fluoroscopy reportedly highlighted a medial femoral condyle fracture, which, together with the persistent pain, prompted the referral to this center. On presentation at our clinic, there was notable focal tenderness over the left medial femoral condyle on the initial physical examination. Radiographs demonstrated a well-positioned, well-fixed prosthesis without obvious fractures (Fig. 1). The patient was prescribed nonsteroidal anti-inflammatory drugs and was instructed to return for follow-up.

At a follow-up appointment 3 months after the initial evaluation at our clinic, the patient reported no changes in symptoms. Repeat physical examination and radiographs were similarly unremarkable. The patient requested conservative management and was referred to interventional pain management. Diagnosed initially with complex regional pain syndrome, he underwent spinal cord stimulation at the left L3-4 dorsal root ganglion. The patient reported an immediate reduction in left knee pain after the spinal cord stimulation trial and later underwent final implantation of the spinal cord stimulation device.
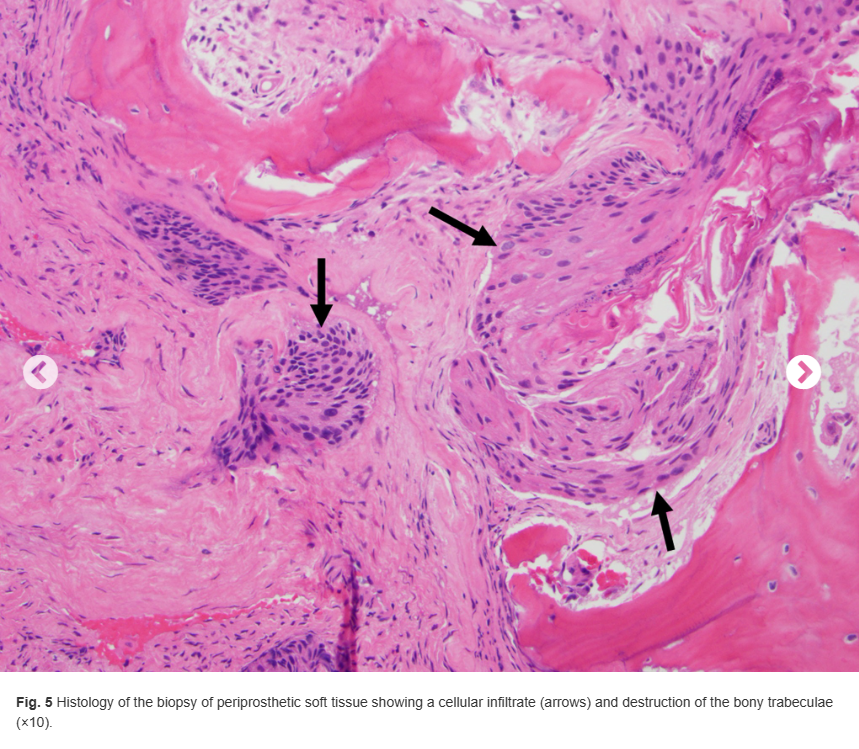
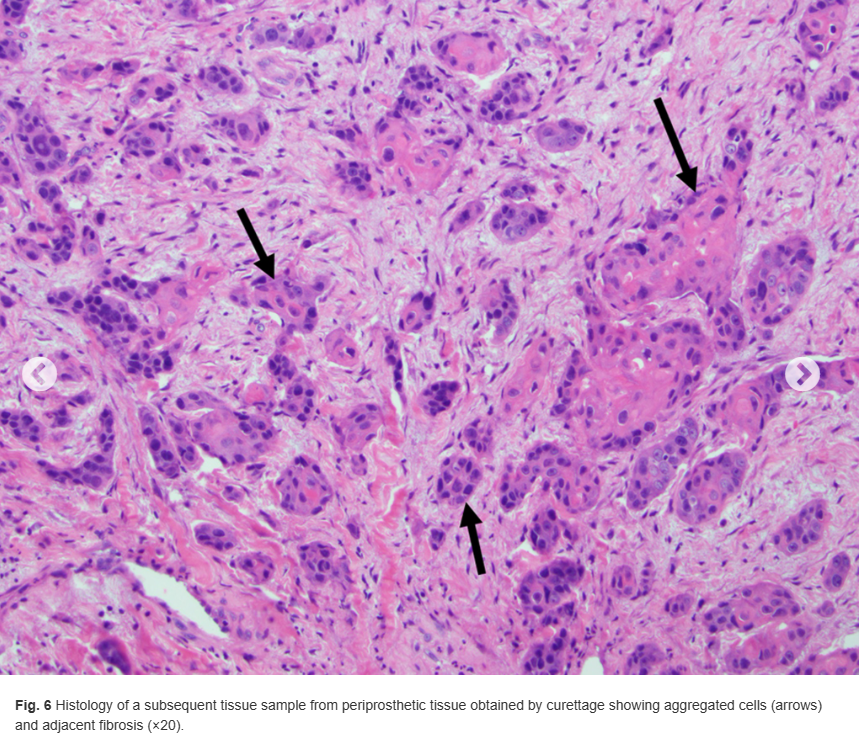
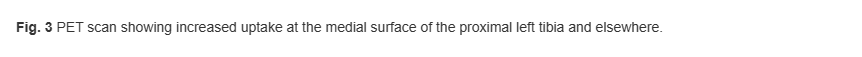
At 7 months after his initial visit, the patient experienced a pop in the left knee while walking. It was followed by an acute increase in knee pain and repeated falls due to an inability to bear weight on the left extremity. When he presented to clinic, the radiograph of the left knee revealed substantial lysis along the medial aspect of the proximal left tibia (Fig. 2). Laboratory studies revealed an elevated C-reactive protein level (35.70 mg/L), an elevated erythrocyte sedimentation rate (55 mm/hour), and normal levels of gamma-globulin in protein electrophoresis. Whole-body positron emission tomography (PET) showed increased radiotracer uptake in the left proximal medial tibia and elsewhere (Fig. 3). Computed tomographic (CT) scans of the left knee revealed a 4-cm destructive lesion in the medial tibial condyle underlying the tibial tray (Fig. 4). Based on the imaging findings and due to concern for a periprosthetic infection, the patient underwent an intraoperative percutaneous biopsy of the tibial lesion with frozen section. This procedure was later followed by curettage.


The histology of the lesion from the biopsy is shown in Figure 5, and the histology of the lesion from curettage is shown in Figure 6.