A 70-year-old man with no history of trauma visited our hospital because he was experiencing shoulder and elbow pain. He had been treated for multiple sclerosis with pulse steroid therapy using 1,000 mg of methylprednisolone sodium succinate. At the time of the initial visit, his body temperature was 37.4°C and tenderness and local heat were positive around the lateral side of the elbow. The shoulder forward elevation was restricted to 20° due to pain. The elbow range of motion was −10° for extension and 90° for flexion.
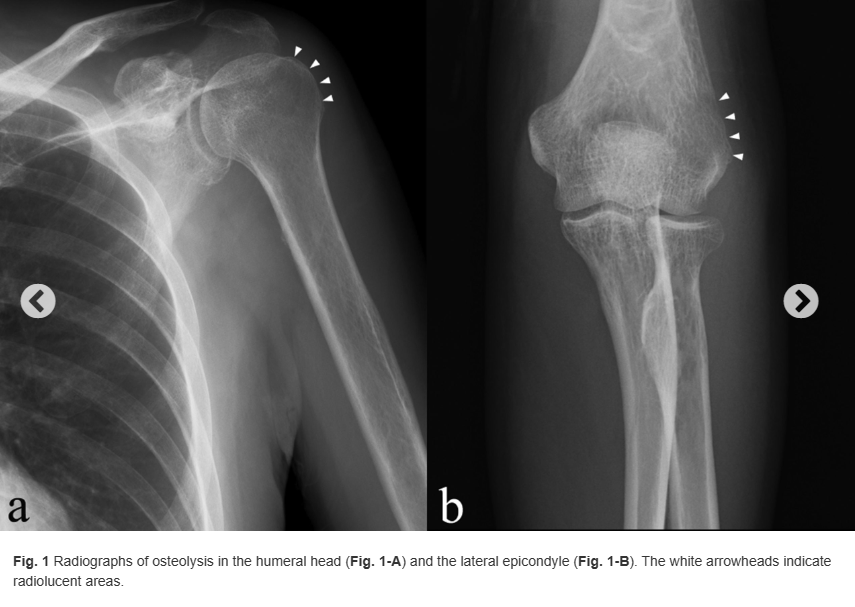
Blood tests showed the C-reactive protein (CRP) concentration to be 5.28 mg/dL (reference range, 0 to 0.14 mg/dL), and the radiographs showed osteolysis in the proximal part of the humerus and the lateral epicondyle (Fig. 1). Fat-suppression techniques in magnetic resonance imaging (MRI) scans revealed diffuse high-signal change in the medullary cavity in both the proximal and the distal epiphyses of the humerus (Fig. 2). The serum beta-d-glucan test was negative.

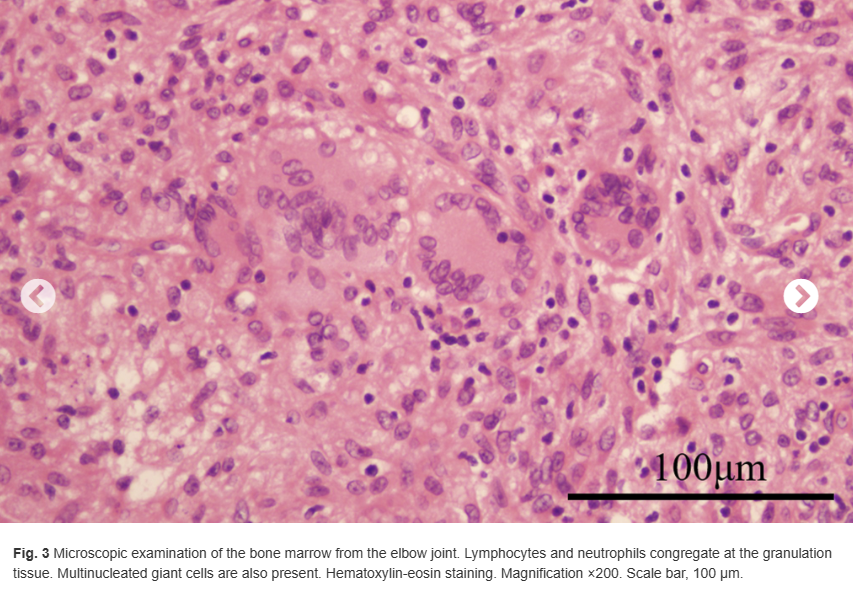
To obtain tissue for diagnosis, surgical debridement of the elbow was performed as ambulatory surgery. A 3-cm skin incision was made on the lateral epicondyle, and serous yellow fluid was found under the subcutaneous tissue. Two samples of the tissue were obtained from the medullary cavity of the humerus through the vulnerable portion of the lateral epicondyle. Afterward, the wound and the elbow joint were lavaged with saline. The wound healed well, and the sutures were removed 10 days after the surgical procedure. There were no complications observed. The pathologic examination revealed lymphocytes and neutrophils congregating in granulation tissue, along with multinucleated giant cells (Fig. 3). The fluid and the tissue sample culture test results were negative.
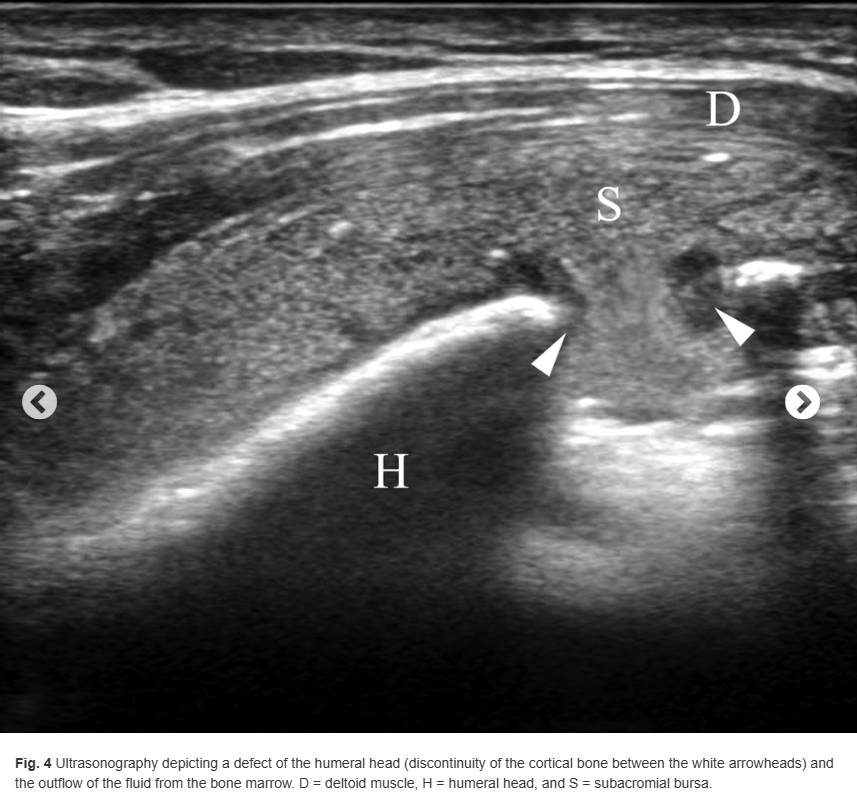
Based on a presumptive diagnosis of septic osteomyelitis, 3-g cefazolin sodium per day was administered intravenously. Subsequently, cephalexin at a dose of 1,500 mg was administered orally for 3 months until the CRP concentration decreased to 0.05 mg/dL. The elbow and shoulder pain subsided, but the shoulder pain recurred 10 days after the antibiotics treatment was completed. Although no signs of inflammation were found in the left elbow, redness, swelling, and tenderness were observed in the left shoulder. Thereafter, the CRP concentration increased to 1.12 mg/dL. Ultrasonography of the shoulder joint depicted discontinuity of the cortical bone of the humeral head (Fig. 4). Furthermore, MRI revealed multiple diffused lesions in the entire humerus (Fig. 5). The cortical bone of the humeral head had a partial defect.

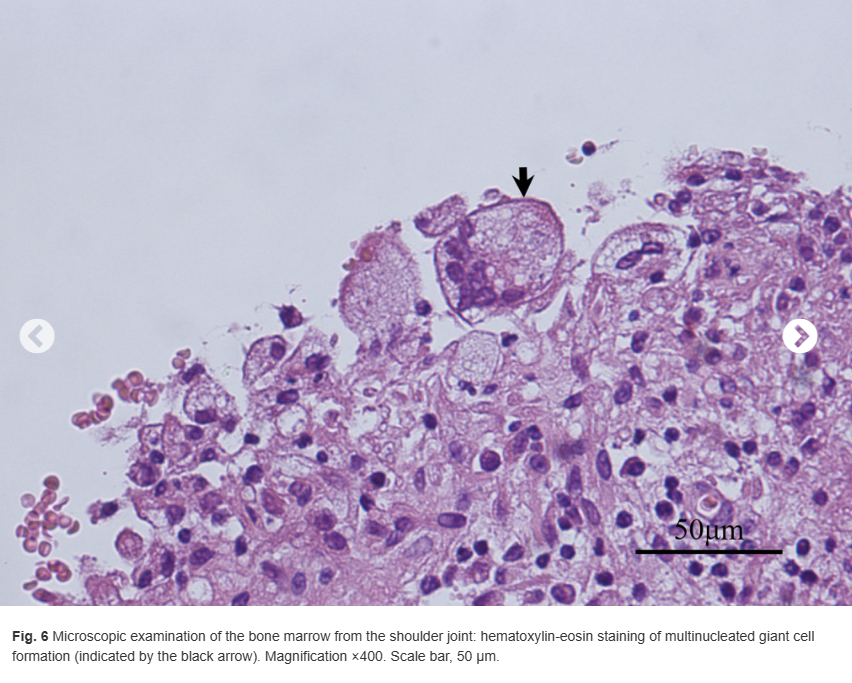
The patient underwent open shoulder debridement, and a 7-cm deltoid-splitting approach was used. Granulation tissue was noted in the subacromial space. After removal of the granulation tissue with electrocautery, the cortical defect (5 mm in diameter) was observed in the humeral head. The granulation tissue and necrotic bone and marrow were curetted. The wound and the shoulder joint were lavaged with saline. The wound healed well, and the skin staples were removed 8 days after the surgical procedure. No complications were observed.
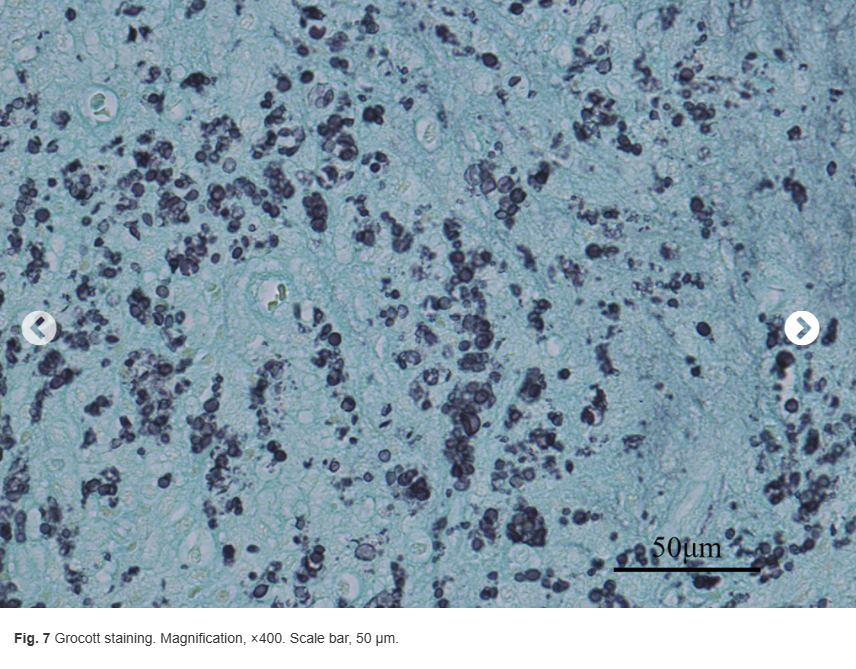
Multinucleated giant cells were observed on microscopic examination of the hematoxylin eosin-stained bone marrow slides in all the samples obtained from the surgical site (Fig. 6). Further pathological examinations were performed with Grocott, periodic acid-Schiff, and Ziehl-Neelsen staining (Fig. 7).
What is the diagnosis?

