1. Introduction
At the turn of 2019 and 2020, the world witnessed the COVID-19 pandemic, which is caused by SARS-CoV-2; this led to a multitude of consequences, starting from immediate closures to drastic changes in our everyday habits [1]. The term “lockdown” has been used extensively in reference to measures, such as confining the population of an entire country to their residential homes and blocking most activities and transportation in an effort to contain the spread of COVID-19 [2]. The need to adapt one’s daily routine to the imposed in-home solution, coupled with the fear of contagion and the potential loss of loved ones, drastically affected people’s mental health; symptoms that are the most associated with this impact include depression, anxiety, and distress [3,4,5,6]. Similarly, “post-lockdown” refers to the period following a lockdown. In the case of COVID-19, it is hard to outline a common time frame, due to the distinct measures adopted in different countries and at different times. As such, it is common to use post-lockdown as a term related to the period following each outbreak wave.
The alternating periods of in-home restrictions and periods with fewer restrictions, combined with a diffuse perception of uncertainty regarding people’s safety and the possibility of returning to a predictable routine, resulted in increased psychological issues [7,8] or, conversely, strengthened resilience, which can be described as the ability to recover from or cope with critical situations [9]. During the first period of the lockdown, Rossi et al. [10] observed a deterioration in mental health in the general Italian population, in terms of post-traumatic stress symptoms, depression, anxiety, insomnia, perceived stress, and adjustment disorder symptoms. However, contradictory results emerged from similar studies that investigated mental health during the lockdown [11]. For instance, Koenig et al. [12] observed no immediate effects on adolescents’ well-being following the initial closure of schools in Germany. Similarly, when using a machine learning approach to investigate the impact of time spent in the lockdown on individuals’ physical well-being, Carollo et al. [13] found that self-perceived loneliness decreased during the first weeks of the lockdown. This result was initially observed in participants living in the United Kingdom and replicated in a sample of participants living in Greece.
To better understand the effects of the COVID-19 pandemic in the post-lockdown periods on people’s mental health, the current work aims to identify the most impactful publications and the main thematic developments of research within the topic. To do so, we analyzed the available scientific literature using a scientometric–bibliometric approach. Scientometrics is a field that involves the integration of scientific mapping (i.e., visualization of the evolution of a research domain in time) and bibliometric analysis (i.e., application of quantitative techniques to bibliometric data) [14,15,16,17]. Compared to other review methods (e.g., narrative review, systematic review, meta-analysis), scientometrics allows identifying the most impactful documents and main thematic domains of research using a data-driven approach applied to examine the existing quantitative relationships between large samples of scientific publications. For these reasons, scientometrics allows reducing the risk of biases when assessing published research in a specific field [18,19]. In the present study, we opted for a document co-citation analysis (DCA) to produce a network of thematic clusters representing the main discussed topics related to mental health in the post-lockdown period. Each cluster, which will be qualitatively developed in detail, includes publications related to specific issues, with the possibility to easily track influential articles.
2. Materials and Methods
This current study follows the pipeline of recent publications in the field of scientometrics (e.g., refs. [20,21,22]). In Scopus, we conducted a literature search on 31st December 2022 using the following string: [TITLE-ABS-KEY((“post lockdown” OR “post lock-down” OR “after lockdown” OR “after lock-down” OR “post pandemic” OR “post-pandemic” OR “following lockdown” OR “following lock-down” OR “following pandemic”) AND (“COVID*” OR “coronavirus” OR “SARS-COV-2”) AND (“depress*” OR “anxi*” OR “stress*” OR “trauma*” OR “mental health” OR “psychiatr*”))]. The terms included in the string reflected the psychological symptoms of the general population after the COVID-19 lockdown. The search yielded 791 documents, which were published or accepted for publication between 2019 and 2023, and included references to 35,816 other documents. We opted to use Scopus over comparable archives (e.g., Web of Science, Medline) due to its broader coverage of recently published documents and indexed journals [23,24]. The downloaded documents were initially analyzed using the bibliometrix package for R developed by Aria and Cuccurullo [25] to uncover the most influential authors, frequent keywords, the most frequent countries appearing in affiliation strings, and the main sources for documents on mental health in the post-lockdown scenario.
2.1. Data Import on CiteSpace
Before proceeding with the scientometric analysis, the file containing 791 publications and their 35,816 references was imported into CiteSpace (version 6.1.R2, 64 bits), according to the suggested guidelines [26,27]. In this phase, all references are screened and regarded as valid only if all of the following pieces of information are available: title, year of publication, author(s), source, volume, pages, DOI [28]. From this initial screening, a total of 34,721 references (96.94% of the total) were recognized as valid. Data loss corresponded to 3.06% of the dataset, which can be considered inconsequential, as it falls below the acceptable range of 1.00–5.00% [29].
2.2. Document Co-Citation Analysis (DCA)
To identify the most impactful publications and main thematic domains of research, a DCA was then computed. DCA is a type of bibliometric analysis that focuses on the patterns of co-citations among documents (i.e., occurrences in which two or more documents are cited together by other publications) [30]. The general assumption behind DCA is that greater co-citation frequencies shared by documents indicate commonalities in terms of research interests and domains of research [31]. To model the patterns of co-citations among documents, DCA creates a network in which documents are included as single nodes and co-citations as edges. In the generated network, the frequencies of co-citations are included as edge weights [32]. Based on the network’s properties, groups of nodes reflecting similar research topics are found and clustered using CiteSpace’s clustering functions.
CiteSpace provides a set of node selection criteria for creating a balanced DCA network that captures the information embedded in the dataset. These criteria are the G-index, top N, and top N%. The G-index is an adaptation of the more popular H-index [33], with the difference that the G-index corresponds to the higher number equivalent to the average number of citations of the author’s most cited g number of publications [34,35]. In CiteSpace, G-index goes along with a scaling factor, k, to change the number of nodes included in the final output [29], where greater k values will generate DCA networks with more nodes. Lastly, top N and top N% have a similar function: the most cited N number or N% of references is selected within a time frame (from here on referred to as time slice) to be nodes. To maximize the amount of retrieved information, the time slice was kept at the value of 1 year for the current work. To determine the best DCA network, the results obtained by using specific selection criteria were compared. DCAs were generated with the following node selection criteria: G-index (k = 15, 25, 50), top N (k = 25, 50, 75), and top N% (k = 5, 10, 15). The network’s structural metrics (explained below), the number of nodes, links, and thematic clusters of research were used to compare the obtained DCAs and to choose the network with the optimal properties.
The steps from the identification of records to the included nodes are presented in Figure 1.
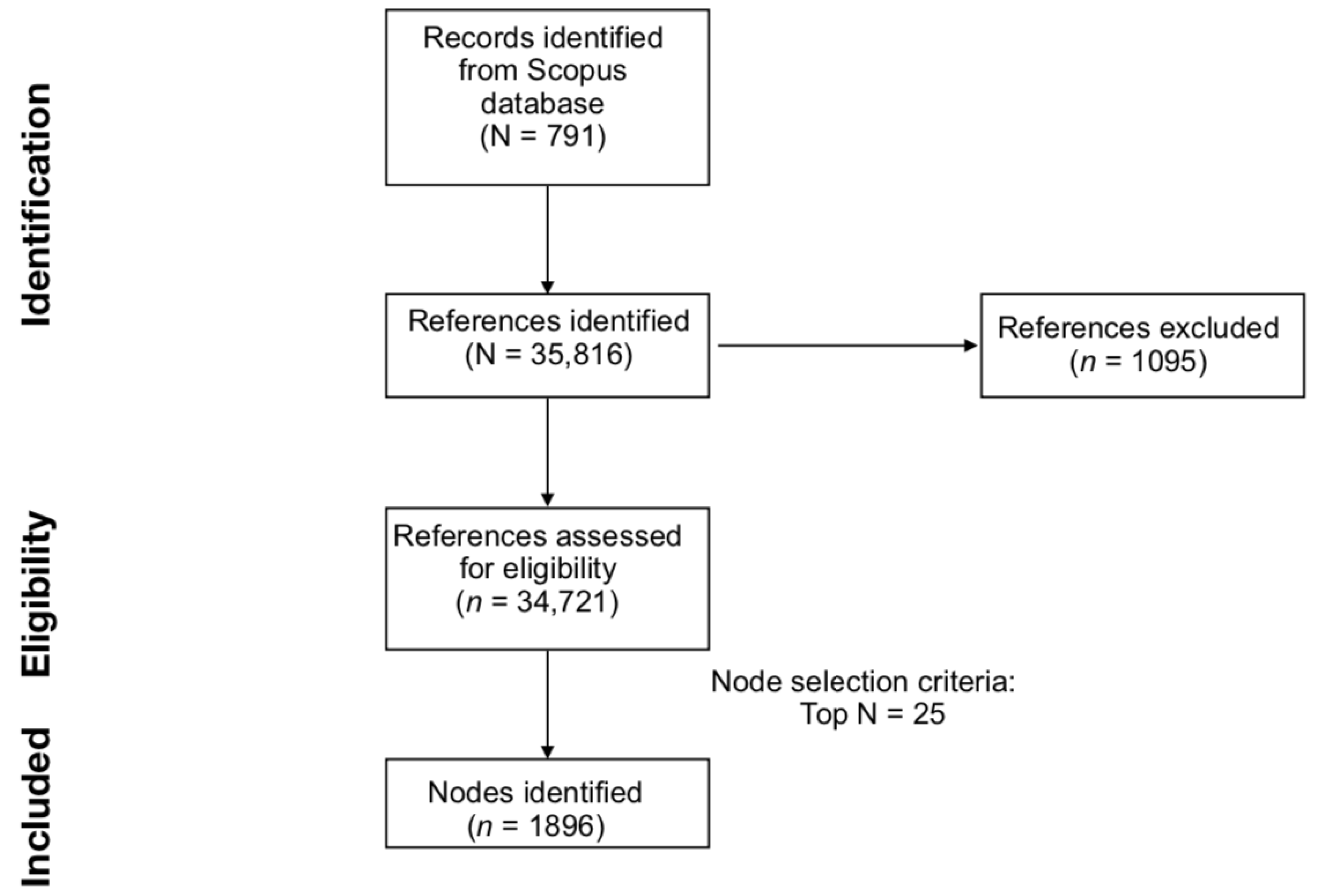
Figure 1. Graphical representation of the literature search, generation of the DCA network generation, and evaluation phases.
Once the optimal network was computed, CiteSpace’s “Find clusters” function was used to divide the network into separate thematic domains of research. Clusters’ labels were automatically generated with CiteSpace’s log-likelihood ratio (LLR) algorithm. The LLR algorithm creates a denomination through the identification of unique terms and expressions included in the titles of the contributing papers [26]. The LLR method provides the most accurate labels when compared to other automatic approaches available in CiteSpace. However, LLR labels, in some cases, might lack accuracy when compared to manually generated labels [36]. For this reason, both LLR and manually generated cluster labels will be provided in the manuscript.
2.3. DCA Network Evaluation Metrics
Many criteria are utilized to assess the created DCA networks. They are categorized as structural or temporal measures. Modularity Q, silhouette, and betweenness centrality are examples of structural metrics. Modularity is a measure of the overall network and its ability to be divided into discrete clusters [37]. The greater its value (ranging from 0 to 1), the more divided or different the network clusters are [31]. Moreover, the silhouette measures the homogeneity of each cluster (i.e., every cluster has its own silhouette measure), where greater estimates (from a minimum of −1 to a maximum of 1) denote a more significant homogeneity of the cluster [38,39]. Furthermore, betweenness centrality quantifies the goodness of the connection between a single node and two other nodes within the network [26,40]. Greater values depict a better connection of the node/publication within the network [39]. Other temporal metrics included in the analyses are citation burstiness and sigma, which evaluate the prominence of each node in the network. Kleinberg’s algorithm was adopted to calculate the citation burstiness [41]. In this computation, greater numbers (with a minimum value of 0) correspond to increased citations of the node (i.e., the publication) in a targeted period (i.e., time slice). As such, a high citation burstiness value depicts publications that have gained significant attention from the scientific community [42]. Sigma is computed through citation burstiness and betweenness centrality values following the formula , where greater scores indicate an elevated impact of the node over the network and, subsequently, suggest the novelty and significance of the publication.
3. Results
3.1. Bibliometric Analysis on the Citing References
The initial bibliometric analysis showed that each citing document obtained an average of 10.28 citations, with a yearly mean of 3.312 citations per document. The documents cited more frequently were authored by Singh et al. [43] (total citations = 644; total citations/year = 161) and Fancourt et al. [44] (total citations = 431; total citations/year = 143.7).
Collectively, 2033 keywords were selected by the authors in the included documents, with the most popular being “COVID-19” (n = 445 appearances), “mental health” (n = 120 appearances), “pandemic” (n = 99 appearances), “lockdown” (n = 81 appearances), “anxiety” (n = 80 appearances), “depression” (n = 77 appearances), “coronavirus” (n = 53 appearances), “COVID-19 pandemic” (n = 47 appearances), “stress” (n = 40 appearances), and “SARS-CoV-2” (n = 23 appearances). Figure 2 includes a graphical representation of the main patterns of co-occurrence between the keywords in the dataset.
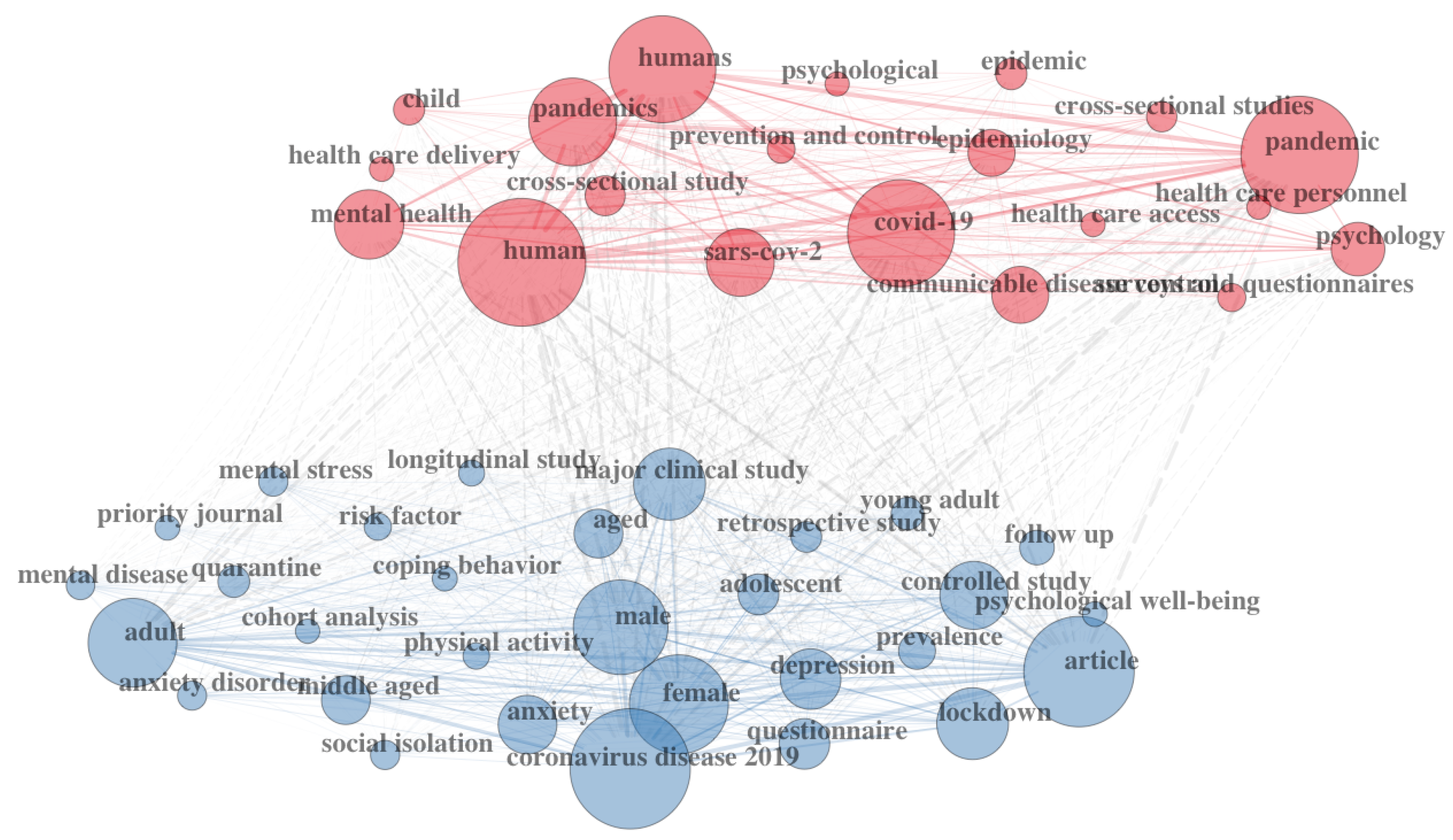
Figure 2. Graphic representation of the co-occurrence of keywords among citing documents.
In the data sample, 4719 distinct authors were identified, with 53 scholars having published 54 single-authored documents. On average, the network included 0.168 documents per author and 6.32 co-authors for each document. The three most productive authors in the data sample were Li J., Liu J., Wang Y., and Wang Y., respectively, with six, five, five, and five published documents.
The corresponding authors were more frequently affiliated with institutions from the United States of America (N = 100; frequency = 0.1464; single-country publications (SCP) = 79; multi-country publications (MCP) = 21), United Kingdom (N = 85; frequency = 0.1245; SCP = 66; MCP = 19), or Italy (N = 77; frequency = 0.1127; SCP = 57; MCP = 20). The graphical results are reported in Figure 3.
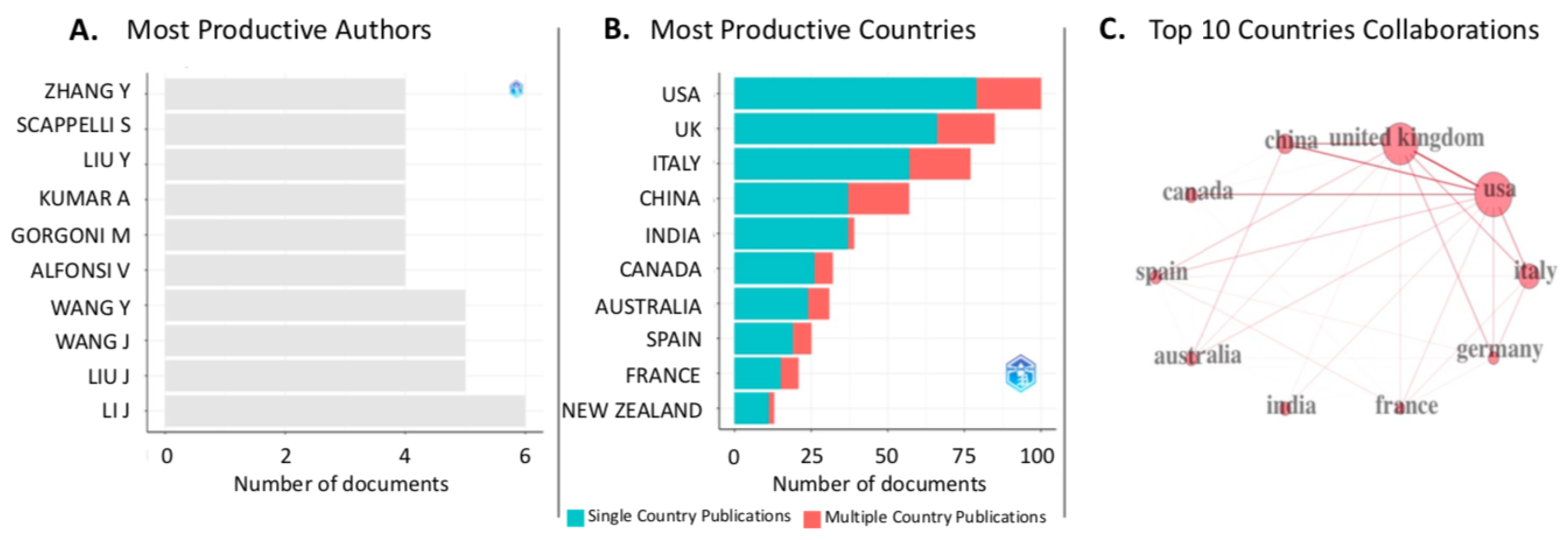
Figure 3. Graphical results of the bibliometric analysis conducted using the bibliometrix package for R [25]. (A) Most productive authors; (B) most productive countries; (C) collaborations among countries are limited to the top 10.
Ultimately, the main sources of documents emerged to be the International Journal of Environmental Research and Public Health (66 documents), Frontiers in Psychiatry (26 documents), and Frontiers in Psychology (24 documents).
3.2. Document Co-Citation Analysis
Following the parameter optimization procedure described in Section 2.2, the final DCA network was created by adopting top N = 25. The DCA network consisted of a total of 1896 nodes and 5776 links (i.e., approximately 3.05 links per node; see Figure 4). Looking at the structural metrics of the network, modularity Q was 0.9447, and the average silhouette was 0.9517. Based on these values, it is possible to infer that the network is highly divisible into highly coherent clusters.

Figure 4. Document co-citation analysis network of the literature found in Scopus about mental health in the post-lockdown period. The network is divided into 8 thematic clusters of research.
Eight major thematic clusters were identified in the network. All eight clusters had their mean publication year in 2020. The largest cluster was cluster no. 1 (mean publication year = 2020), with a size of 86 documents. The most homogeneous clusters were no. 4, no. 11, no. 18, no. 43, and no. 47, all with a maximum silhouette score of (=1.00). This score is probably due to the fact that in all of these clusters, there is only one citing article. Details of the distinct clusters are reported in . presents both the labels computed with the LLR method (LLR Label) and the ones created manually (suggested label).
Proceeding with the results, 43 documents displayed a significant citation burstiness within the network; however, 4 of these turned out to be repetitions of other documents already within this list (i.e., refs. [45,46,47,48]). For this reason, the final number of documents with significant burstiness strength was 39. In , the top 20 documents are presented, which are the most relevant to the discussion. The three articles showing the greatest values of citation burstiness are as follows: Brooks et al. [45] (citation burstiness = 29.18), which is a review debating the psychological impact of the lockdown; Xiong et al. [49] (citation burstiness = 15.99), which is a systematic review that synthesizes the literature on the psychological outcomes of COVID-19 on the general population and the associated risk factors; Holmes et al. [46] (citation burstiness = 8.43), which is an exploration of the psychological, social, and neuropsychological effects of COVID-19, discussing the most prominent priorities and identifying long-term strategies for scientific research in mental health.
4. Discussion
The purpose of this report is to review the research on the consequences of the COVID-19 epidemic on mental health following the lockdown. A DCA network with eight clusters was created using a scientometric approach. Furthermore, 39 documents with substantial citation bursts are identified.
Each cluster will be presented qualitatively, from the largest to the smallest, according to the cluster size (i.e., the number of documents included in the cluster). The citing papers included in each cluster are distinguished by their coverage (amount of references in that cluster reported in that paper) and overall citing score (GCS, meaning the total amount of citations retrieved by Scopus for that paper). The labels are named using a manual approach as it provides a more accurate representation of the clusters’ research themes [21].
4.1. Cluster No. 1: Long-Term Effects and Resilience
The main citing articles for cluster no. 1 (LLR title = ”Resilience”; silhouette = 0.853) are reported in . Within the macro-topic concerning the long-term effects of COVID-19 and resilience, the documents included in this cluster present a variety of arguments that can be grouped into sub-topics. As such, the documents will be discussed in narrower sections to facilitate the comprehension of the state of the art.
4.2. Cluster No. 4: Novelty Seeking and Support System
This cluster (LLR title = ”Resilience”; silhouette = 1.000), consisting of two citing articles, focuses on two different themes: novelty seeking and support system, each addressed by one of the two documents.
Li et al. [64] conducted a longitudinal study to examine changes in novelty seeking over three distinct time periods: before, during, and after the lockdown. Across all time points, higher levels of novelty seeking were associated with fewer depressive, anxious, and stress-related symptoms. Novelty-seeking reached its peak in the post-lockdown period. Stress, anxiety, and depression decreased during the lockdown and increased again in the post-lockdown period. Overall, the results seem to suggest that novelty-seeking acts as a protective personal factor against negative mental health outcomes. However, the causal direction of the relationship between the levels of novelty seeking and mental health cannot be determined from the cross-sectional design of the study [64].
Suhail et al. [88] showed that, in the Indian population, support from families, friends, and significant others, functioned as a protective factor in reducing the risk of developing psychiatric symptoms (e.g., somatic symptoms, anxiety, and depression) during the COVID-19 pandemic. Other studies in the literature have highlighted the importance of social support against negative mental health outcomes. For instance, Elmer et al. [122] observed that isolation in social networks, the lack of interaction and emotional support, and physical isolation were associated with negative mental health trajectories in a sample of Swiss undergraduate students.
4.3. Cluster No. 11: Pediatric Hospitalization
This cluster (LLR title = ”During”; silhouette = 1.000) consists of only one citing article authored by Chong et al. [123]. The authors focused on the admissions at pediatric hospital services due to the impact of COVID-19. Specifically, the investigation concerned access to the emergency department, diagnostic resources, and the use of hospital facilities in Singapore. The findings highlighted a considerable drop in admissions related to the virus contagion, which was most likely due to the lockdown, as well as an increase in the relative share of trauma-related attendances. A reduction in admissions at pediatric hospitals during lockdown was observed worldwide both in regards to infectious diseases as well as other conditions [129].
4.4. Cluster No. 17: Emotion Impact and Transmission
Cluster no. 17 (LLR title = ”Dynamics”, silhouette = 0.999), consisting of two citing papers, was renamed “Emotion Impact and Transmission”. The article by Presti et al. [124] discussed the dynamics of fear during the pandemic from a theoretical perspective. For instance, the authors noted that we react to fear symbolically and that we link emotions to other things and events using linguistic associations. Thus, language can modify the way we experience events and, as a result, affect how functionally or dysfunctionally oriented we are in the context that surrounds us.
Reference [125] explored the effects of COVID-19 (from before, during, and after the outbreak) on the psychological symptoms in school-age children and their mothers by using self-report instruments. The authors created two experimental groups: mothers at-risk for psychopathology and non-at-risk mothers. In doing so, the authors aimed to test whether the psychopathological risk of parents was associated with increases in behavioral problems among children during the pandemic. At-risk mothers exhibited a generally decreasing trajectory of psychopathological symptoms and related behaviors over time. However, there were no significant changes in children’s aggression or depression levels when comparing the three time-points. In the group with non-at-risk mothers, children’s aggression levels were lower after the quarantine period, while scores related to depressive symptoms were significantly higher during and after the lockdown. Taking these findings together, it appears that maternal risk for psychopathology does not affect specific aspects of children’s emotional and behavioral functioning; rather, it impacts the overall psychological well-being of their offspring.
4.5. Cluster No. 18: Mental Health Services
Cluster no. 18 (LLR title = mental health service; silhouette = 1.000), consists of one citing article [65]. The paper evaluated the medium-term influence of COVID-19 on admissions to mental health centers in secondary care. According to the results, after an initial decrease in mental health referrals, an acceleration in the referrals—meaning access and permanence in hospital wards—was observed. This acceleration was defined as the variation of daily referrals, computed as follows:
4.6. Cluster No. 43: Adolescents
This cluster (LLR title = ”Spanish Adolescent” silhouette = 1.000) consists of one citing article [126]. Ezpeleta et al. [126] investigated the mental health of adolescents following the period of in-home closure in a sample of Spanish adolescents. The results of the study report worsened mental health in terms of behavioral conduct, prosociality, and peer relationships. In addition, higher conduct problems (e.g., fights, bullying of other children, lying, cheating, tantrums) were linked to maladaptive relationships in adolescents (e.g., deteriorated connections with family members, failure when communicating with friends online), parental behavior at home (e.g., arguing, giving up enforcing rules), and adolescent activities (e.g., difficulties in keeping up with daily routines, excessive screen time exposure). However, the authors noted that the results might not be generalizable to adolescents with lower socioeconomic statuses [126].
4.7. Cluster No. 47: Healthcare Workers
Cluster no. 47 (LLR title = ”Healthcare Worker”, silhouette = 1.000), consists of one citing article [127]. Allan et al. [127] investigated the prevalence of psychological symptoms in healthcare workers servicing wards where COVID-19 patients were treated. The authors adopted a longitudinal study consisting of 3 time periods: 1.5–6.9 months after the pandemic’s peak, 6–11.9 months after the peak, and at least 12 months after the peak of infections. According to the results, the predominant symptoms included post-traumatic stress symptoms and general psychiatric caseness. Similarly, Rossi et al. [130] observed that almost half of the recruited healthcare workers reported post-traumatic stress symptoms. In the same study, almost a quarter of the sample reported symptoms of depression, while one-fifth reported symptoms of anxiety.
4.8. Cluster No. 51: Physical Activity and Substance Use
Cluster no. 51 (LLR title = ”Change”, silhouette = 0.998) consists of two citing articles and focuses on behavioral changes during the lockdown, especially physical activity and substance use. In particular, Anyan et al. [128] analyzed the correlation between changes in physical activity and the corresponding anxiety and depressive symptoms, as well as the levels of resilience found in response to the restrictions adopted during COVID-19. The authors found that lower levels of physical activity were associated with a higher risk for depression and anxiety symptoms, especially for younger participants. However, higher resilience was a protective factor against depression and anxiety symptoms. With a review of studies conducted during the first year of COVID-19, Marconcin et al. [131] found similar results, with higher physical activity being associated with higher well-being, quality of life, and lower depressive symptoms, anxiety, and stress, independent of age.
Reference [100] investigated the relationship between changes in seeking and using substances, such as alcohol, during the first COVID-19 closure, and related psychological symptoms, in terms of depression, anxiety, and resilience. In the post-pandemic phase, people reported higher use of tobacco and cannabis. Lower cannabis usage was associated with higher anxiety symptoms and lower resilience scores.
5. Limitations of the Study
It is essential to mention that the present work has some limitations. First, one limitation of the study is the Scopus document selection mode. To retrieve documents, we searched for specific key terms in publication titles, abstracts, and keywords. For this reason, the present analysis might have unintentionally excluded some relevant documents that were not captured by the adopted key terms in the search string. This is especially relevant considering the challenge of finding a homogeneous set of key terms to retrieve literature studies on mental health in the post-lockdown period. This challenge was amplified by the relatively recent nature of the post-lockdown period as well as the temporal diversities across countries, in terms of contagious waves and lockdown restrictions. For this reason, among the 791 documents retrieved, some dealt with the period following the first lockdown, others were related to a subsequent lockdown, and others were related to both.
Another limitation regards the choice of the platform used for conducting the literature search, which was Scopus, in our case. Some relevant documents might have been unintentionally excluded because they were published in journals or books that are not indexed in Scopus [132].
Furthermore, the temporal sequence of events did not make it possible to create a study with stable and well-defined data. Parameters, such as citation bursts, were temporally incomplete and, therefore, needed to be interpreted cautiously, as the network documents were very recent. From this point of view, most of them present a burstiness time frame that began in 2020 or 2021 and may not have ended yet. As such, it would be interesting to replicate the scientometric analysis in a few years, to assess the consideration by other scientific works in the longer term.
Lastly, while the DCA provides a quantitative analysis of co-citation frequencies, no information about the qualitative relationships among documents can be obtained from the software [27]. For this reason, scientometric experts advise integrating a qualitative discussion, as was conducted in this study, to better understand the content of the clusters [133].
6. Conclusions
Despite the novelty of the COVID-19 phenomenon, many research studies on the psychological and psychiatric consequences of the pandemic were published during the time frame considered in this study. The implications of the present study in the clinical setting can be extended to the analyzed symptom classes in the various clusters. The pandemic has widely affected well-being, and it would be relevant to continue monitoring the mental health of the population, including both clinical and healthy individuals. Furthermore, more research is needed to understand the impact of COVID-19 restrictions on populations with lower socioeconomic status. Looking closer at the articles that emerged from the scientometric analysis, it appears that, while the common thread is represented by mental health conditions related to the pandemic, the topics are diversified and include efforts to find more accessible treatment solutions and prevention strategies in case of further global challenges. As such, it appears that social connectedness acts as a common denominator when facing worldwide adversities, suggesting that both individual and collective factors should be taken into account. Accordingly, social connectedness played a protective role during COVID-19 lockdown restrictions by reducing negative physical and mental health outcomes [134]. On the organizational level, the pandemic emergency exposed the vulnerabilities of national health systems and the planning of international guidelines, leading to even more severe consequences [135]. This emergency presents an opportunity for future research to assess and improve healthcare systems [136,137]. Future studies should also focus on the developmental trajectories of children and adolescents to determine the long-term consequences of the pandemic and post-lockdown period on education, relationships, and mental health.
References
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef]
- Mækelæ, M.J.; Reggev, N.; Dutra, N.; Tamayo, R.M.; Silva-Sobrinho, R.A.; Klevjer, K.; Pfuhl, G. Perceived efficacy of COVID-19 restrictions, reactions and their impact on mental health during the early phase of the outbreak in six countries. R. Soc. Open Sci. 2020, 7, 200644. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Husky, M.M.; Kovess-Masfety, V.; Swendsen, J.D. Stress and anxiety among university students in France during Covid-19 mandatory confinement. Compr. Psychiatry 2020, 102, 152191. [Google Scholar] [CrossRef]
- Serafini, G.; Parmigiani, B.; Amerio, A.; Aguglia, A.; Sher, L.; Amore, M. The psychological impact of COVID-19 on the mental health in the general population. QJM Int. J. Med. 2020, 113, 531–537. [Google Scholar] [CrossRef]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Prati, G.; Mancini, A.D. The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021, 51, 201–211. [Google Scholar] [CrossRef]
- Khubchandani, J.; Sharma, S.; Webb, F.J.; Wiblishauser, M.J.; Bowman, S.L. Post-lockdown depression and anxiety in the USA during the COVID-19 pandemic. J. Public Health 2021, 43, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Silveira, S.; Hecht, M.; Matthaeus, H.; Adli, M.; Voelkle, M.C.; Singer, T. Coping with the COVID-19 Pandemic: Perceived Changes in Psychological Vulnerability, Resilience and Social Cohesion before, during and after Lockdown. Int. J. Environ. Res. Public Health 2022, 19, 3290. [Google Scholar] [CrossRef] [PubMed]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Di Marco, A.; Rossi, A.; Siracusano, A.; Di Lorenzo, G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatry 2020, 11, 790. [Google Scholar] [CrossRef] [PubMed]
- Richter, D.; Riedel-Heller, S.; Zürcher, S.J. Mental health problems in the general population during and after the first lockdown phase due to the SARS-CoV-2 pandemic: Rapid review of multi-wave studies. Epidemiol. Psychiatr. Sci. 2021, 30, e27. [Google Scholar] [CrossRef] [PubMed]
- Koenig, J.; Kohls, E.; Moessner, M.; Lustig, S.; Bauer, S.; Becker, K.; Thomasius, R.; Eschenbeck, H.; Diestelkamp, S.; Gillé, V.; et al. The impact of COVID-19 related lockdown measures on self-reported psychopathology and health-related quality of life in German adolescents. Eur. Child Adolesc. Psychiatry 2021, 32, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Carollo, A.; Bizzego, A.; Gabrieli, G.; Wong, K.K.Y.; Raine, A.; Esposito, G. I’m alone but not lonely. U-shaped pattern of self-perceived loneliness during the COVID-19 pandemic in the UK and Greece. Public Health Pract. 2021, 2, 100219. [Google Scholar] [CrossRef]
- Carollo, A.; Montefalcone, P.; Bornstein, M.H.; Esposito, G. A Scientometric Review of Infant Cry and Caregiver Responsiveness: Literature Trends and Research Gaps over 60 Years of Developmental Study. Children 2023, 10, 1042. [Google Scholar] [CrossRef]
- Donthu, N.; Kumar, S.; Mukherjee, D.; Pandey, N.; Lim, W.M. How to conduct a bibliometric analysis: An overview and guidelines. J. Bus. Res. 2021, 133, 285–296. [Google Scholar] [CrossRef]
- Nakagawa, S.; Samarasinghe, G.; Haddaway, N.R.; Westgate, M.J.; O’Dea, R.E.; Noble, D.W.; Lagisz, M. Research weaving: Visualizing the future of research synthesis. Trends Ecol. Evol. 2019, 34, 224–238. [Google Scholar] [CrossRef]
- Sabe, M.; Pillinger, T.; Kaiser, S.; Chen, C.; Taipale, H.; Tanskanen, A.; Tiihonen, J.; Leucht, S.; Correll, C.U.; Solmi, M. Half a century of research on antipsychotics and schizophrenia: A scientometric study of hotspots, nodes, bursts, and trends. Neurosci. Biobehav. Rev. 2022, 136, 104608. [Google Scholar] [CrossRef]
- Chen, C. CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. J. Am. Soc. Inf. Sci. Technol. 2006, 57, 359–377. [Google Scholar] [CrossRef]
- Mulchenko, Z. Measurement of science, study of the development of science as an information process. In USAF Foreign Technology Division Translation AD735634; U.S. Air Force Systems Command, Foreign Technology Division: Washington, DC, USA, 1969. [Google Scholar]
- Neoh, M.J.Y.; Carollo, A.; Lim, M.; Corazza, O.; Coppola, A.; Esposito, G. The Novel Psychoactive Substances Epidemic: A Scientometric Perspective. Addict. Neurosci. 2022, 5, 100060. [Google Scholar] [CrossRef]
- Bonacina, G.; Carollo, A.; Esposito, G. The Genetic Side of the Mood: A Scientometric Review of the Genetic Basis of Mood Disorders. Genes 2023, 14, 352. [Google Scholar] [CrossRef]
- Lim, M.; Carollo, A.; Neoh, M.J.Y.; Esposito, G. Mapping miRNA Research in Schizophrenia: A Scientometric Review. Int. J. Mol. Sci. 2023, 24, 436. [Google Scholar] [CrossRef]
- Falagas, M.E.; Pitsouni, E.I.; Malietzis, G.A.; Pappas, G. Comparison of PubMed, Scopus, web of science, and Google scholar: Strengths and weaknesses. FASEB J. 2008, 22, 338–342. [Google Scholar] [CrossRef]
- Cataldo, I.; Lieu, A.A.; Carollo, A.; Bornstein, M.H.; Gabrieli, G.; Lee, A.; Esposito, G. From the cradle to the web: The growth of “sharenting”—A scientometric perspective. Hum. Behav. Emerg. Technol. 2022, 2022, 5607422. [Google Scholar] [CrossRef]
- Aria, M.; Cuccurullo, C. bibliometrix: An R-tool for comprehensive science mapping analysis. J. Inf. 2017, 11, 959–975. [Google Scholar] [CrossRef]
- Chen, C. The citespace manual. Coll. Comput. Inform. 2014, 1, 1–84. [Google Scholar]
- Lim, M.; Carollo, A.; Dimitriou, D.; Esposito, G. Recent Developments in Autism Genetic Research: A Scientometric Review from 2018 to 2022. Genes 2022, 13, 1646. [Google Scholar] [CrossRef] [PubMed]
- Chen, C. The CiteSpace Manual; College of Computing and Informatics: Philadelphia, PA, USA, 2014; pp. 1–84. [Google Scholar]
- Chen, C. CiteSpace: A Practical Guide for Mapping Scientific Literature; Nova Science Publishers: Hauppauge, NY, USA, 2016. [Google Scholar]
- Small, H. Co-citation context analysis and the structure of paradigms. J. Doc. 1980, 36, 183–196. [Google Scholar] [CrossRef]
- Chen, C.; Ibekwe-SanJuan, F.; Hou, J. The structure and dynamics of cocitation clusters: A multiple-perspective cocitation analysis. J. Am. Soc. Inf. Sci. Technol. 2010, 61, 1386–1409. [Google Scholar] [CrossRef]
- Trujillo, C.M.; Long, T.M. Document co-citation analysis to enhance transdisciplinary research. Sci. Adv. 2018, 4, e1701130. [Google Scholar] [CrossRef]
- Egghe, L. An improvement of the h-index: The g-index. ISSI Newsl. 2006, 2, 8–9. [Google Scholar]
- Bornmann, L.; Daniel, H.D. What do we know about the h index? J. Am. Soc. Inf. Sci. Technol. 2007, 58, 1381–1385. [Google Scholar] [CrossRef]
- Alonso, S.; Cabrerizo, F.J.; Herrera-Viedma, E.; Herrera, F. h-Index: A review focused in its variants, computation and standardization for different scientific fields. J. Inf. 2009, 3, 273–289. [Google Scholar] [CrossRef]
- Carollo, A.; Lim, M.; Aryadoust, V.; Esposito, G. Interpersonal Synchrony in the Context of Caregiver-Child Interactions: A Document Co-citation Analysis. Front. Psychol. 2021, 12, 701824. [Google Scholar] [CrossRef]
- Newman, M.E. Modularity and community structure in networks. Proc. Natl. Acad. Sci. USA 2006, 103, 8577–8582. [Google Scholar] [CrossRef]
- Rousseeuw, P.J. Silhouettes: A graphical aid to the interpretation and validation of cluster analysis. J. Comput. Appl. Math. 1987, 20, 53–65. [Google Scholar] [CrossRef]
- Aryadoust, V.; Ang, B.H. Exploring the frontiers of eye tracking research in language studies: A novel co-citation scientometric review. Comput. Assist. Lang. Learn. 2019, 34, 898–933. [Google Scholar] [CrossRef]
- Freeman, L.C. A set of measures of centrality based on betweenness. In Sociometry; American Sociological Association: Washington, DC, USA, 1977; pp. 35–41. [Google Scholar]
- Kleinberg, J. Bursty and hierarchical structure in streams. Data Min. Knowl. Discov. 2003, 7, 373–397. [Google Scholar] [CrossRef]
- Chen, C. Science mapping: A systematic review of the literature. J. Data Inf. Sci. 2017, 2, 1–40. [Google Scholar] [CrossRef]
- Singh, S.; Roy, D.; Sinha, K.; Parveen, S.; Sharma, G.; Joshi, G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 2020, 293, 113429. [Google Scholar] [CrossRef]
- Fancourt, D.; Steptoe, A.; Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. Lancet Psychiatry 2021, 8, 141–149. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef] [PubMed]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatry 2020, 52, 102066. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Casagrande, M.; Favieri, F.; Tambelli, R.; Forte, G. The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020, 75, 12–20. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; North, C.S. Mental health and the COVID-19 pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef]
- Fiorillo, A.; Gorwood, P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry 2020, 63, e32. [Google Scholar] [CrossRef] [PubMed]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef]
- Wang, G.; Zhang, Y.; Zhao, J.; Zhang, J.; Jiang, F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 2020, 395, 945–947. [Google Scholar] [CrossRef] [PubMed]
- Odriozola-González, P.; Planchuelo-Gómez, Á.; Irurtia, M.J.; de Luis-García, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020, 290, 113108. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 1–11. [Google Scholar] [CrossRef]
- Galea, S.; Merchant, R.M.; Lurie, N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Intern. Med. 2020, 180, 817–818. [Google Scholar] [CrossRef]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.A.; McGuire, P.; Fusar-Poli, P.; Zandi, M.S.; Lewis, G.; David, A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef]
- Jiao, W.Y.; Wang, L.N.; Liu, J.; Fang, S.F.; Jiao, F.Y.; Pettoello-Mantovani, M.; Somekh, E. Behavioral and emotional disorders in children during the COVID-19 epidemic. J. Pediatr. 2020, 221, 264–266. [Google Scholar] [CrossRef]
- Schnell, T.; Krampe, H. Meaning in life and self-control buffer stress in times of COVID-19: Moderating and mediating effects with regard to mental distress. Front. Psychiatry 2020, 11, 983. [Google Scholar] [CrossRef]
- Li, W.W.; Yu, H.; Miller, D.J.; Yang, F.; Rouen, C. Novelty seeking and mental health in Chinese university students before, during, and after the COVID-19 pandemic lockdown: A longitudinal study. Front. Psychol. 2020, 11, 600739. [Google Scholar] [CrossRef]
- Chen, S.; She, R.; Qin, P.; Kershenbaum, A.; Fernandez-Egea, E.; Nelder, J.R.; Ma, C.; Lewis, J.; Wang, C.; Cardinal, R.N. The medium-term impact of COVID-19 lockdown on referrals to secondary care mental health services: A controlled interrupted time series study. Front. Psychiatry 2020, 11, 585915. [Google Scholar] [CrossRef] [PubMed]
- Min, S.; Jeong, Y.H.; Kim, J.; Koo, J.W.; Ahn, Y.M. The Aftermath: Post-pandemic Psychiatric Implications of the COVID-19 Pandemic, a South Korean Perspective. Front. Psychiatry 2021, 12, 671722. [Google Scholar] [CrossRef] [PubMed]
- Dumitrache, L.; Stănculescu, E.; Nae, M.; Dumbrăveanu, D.; Simion, G.; Taloș, A.M.; Mareci, A. Post-Lockdown effects on students’ mental health in romania: Perceived stress, missing daily social interactions, and boredom proneness. Int. J. Environ. Res. Public Health 2021, 18, 8599. [Google Scholar] [CrossRef] [PubMed]
- Charbonnier, E.; Le Vigouroux, S.; Goncalves, A. Psychological vulnerability of French university students during the COVID-19 pandemic: A four-wave longitudinal survey. Int. J. Environ. Res. Public Health 2021, 18, 9699. [Google Scholar] [CrossRef]
- Zapata-Ospina, J.P.; Patiño-Lugo, D.F.; Vélez, C.M.; Campos-Ortiz, S.; Madrid-Martínez, P.; Pemberthy-Quintero, S.; Pérez-Gutiérrez, A.M.; Ramírez-Pérez, P.A.; Vélez-Marín, V.M. Mental health interventions for college and university students during the COVID-19 pandemic: A critical synthesis of the literature. Rev. Colomb. Psiquiatr. 2021, 50, 199–213. [Google Scholar] [CrossRef]
- Morris, G.; Groom, R.; Schuberg, E.; Atkinson, J.; Atkinson, C.; Ungunmerr-Baumann, M.R. Mitigating Contemporary Trauma Impacts Using Ancient Applications. Front. Psychol. 2022, 13, 645397. [Google Scholar] [CrossRef]
- Liu, J.; Peng, Z.; Cai, X.; Peng, Y.; Li, J.; Feng, T. Students’ intention of visiting urban green spaces after the COVID-19 lockdown in China. Int. J. Environ. Res. Public Health 2021, 18, 8601. [Google Scholar] [CrossRef]
- Leightley, D.; Lavelle, G.; White, K.M.; Sun, S.; Matcham, F.; Ivan, A.; Oetzmann, C.; Penninx, B.W.; Lamers, F.; Siddi, S.; et al. Investigating the impact of COVID-19 lockdown on adults with a recent history of recurrent major depressive disorder: A multi-Centre study using remote measurement technology. BMC Psychiatry 2021, 21, 1–11. [Google Scholar] [CrossRef]
- Anindyajati, G.; Wiguna, T.; Murtani, B.J.; Christian, H.; Wigantara, N.A.; Putra, A.A.; Hanafi, E.; Minayati, K.; Ismail, R.I.; Kaligis, F.; et al. Anxiety and its associated factors during the initial phase of the COVID-19 pandemic in Indonesia. Front. Psychiatry 2021, 12, 253. [Google Scholar] [CrossRef]
- Stallard, P.; Pereira, A.I.; Barros, L. Post-traumatic growth during the COVID-19 pandemic in carers of children in Portugal and the UK: Cross-sectional online survey. BJPsych Open 2021, 7, e37. [Google Scholar] [CrossRef]
- Daniels, J.; Rettie, H. The Mental Health Impact of the COVID-19 Pandemic Second Wave on Shielders and Their Family Members. Int. J. Environ. Res. Public Health 2022, 19, 7333. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, Y.; Lin, H.; Chen, X.; Wang, H.; Liang, H.; Guo, X.; Fu, C. Mental health problems among school-aged children after school reopening: A cross-sectional study during the COVID-19 post-pandemic in east China. Front. Psychol. 2021, 12, 773134. [Google Scholar] [CrossRef] [PubMed]
- Fioretti, A.; Natalini, E.; Triggianese, G.; Eibenstein, R.; Angelone, A.M.; Lauriello, M.; Eibenstein, A. Impact of the COVID-19 Lockdown on Patients with Chronic Tinnitus—Preliminary Results. Audiol. Res. 2022, 12, 327–336. [Google Scholar] [CrossRef]
- Dalkner, N.; Wagner-Skacel, J.; Ratzenhofer, M.; Fellendorf, F.; Lenger, M.; Maget, A.; Tmava-Berisha, A.; Pilz, R.; Queissner, R.; Hamm, C.; et al. Psychological symptoms during and after Austrian first lockdown in individuals with bipolar disorder? A follow-up control-group investigation. Int. J. Bipolar Disord. 2021, 9, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Siddi, S.; Giné-Vázquez, I.; Bailon, R.; Matcham, F.; Lamers, F.; Kontaxis, S.; Laporta, E.; Garcia, E.; Arranz, B.; Dalla Costa, G.; et al. Biopsychosocial Response to the COVID-19 Lockdown in People with Major Depressive Disorder and Multiple Sclerosis. J. Clin. Med. 2022, 11, 7163. [Google Scholar] [CrossRef] [PubMed]
- Khanna, A.; Jones, G.B. Envisioning post-pandemic digital neurological, psychiatric and mental health care. Front. Digit. Health 2021, 3, 803315. [Google Scholar] [CrossRef]
- Gorgoni, M.; Scarpelli, S.; Mangiaruga, A.; Alfonsi, V.; Bonsignore, M.R.; Fanfulla, F.; Ferini-Strambi, L.; Nobili, L.; Plazzi, G.; De Gennaro, L.; et al. Persistence of the effects of the COVID-19 lockdown on sleep: A longitudinal study. Brain Sci. 2021, 11, 1520. [Google Scholar] [CrossRef]
- Sirikul, W.; Ongprasert, K.; Piankusol, C.; Siviroj, P. Maternal mental health under COVID-19 pandemic in Thailand. Int. J. Environ. Res. Public Health 2021, 19, 347. [Google Scholar] [CrossRef]
- Campos, J.A.D.B.; Campos, L.A.; Bueno, J.L.; Martins, B.G. Emotions and mood swings of pharmacy students in the context of the coronavirus disease of 2019 pandemic. Curr. Pharm. Teach. Learn. 2021, 13, 635–642. [Google Scholar] [CrossRef]
- Žuljević, M.F.; Jeličić, K.; Viđak, M.; Đogaš, V.; Buljan, I. Impact of the first COVID-19 lockdown on study satisfaction and burnout in medical students in Split, Croatia: A cross-sectional presurvey and postsurvey. BMJ Open 2021, 11, e049590. [Google Scholar] [CrossRef]
- Samy, A.L.; Awang Bono, S.; Tan, S.L.; Low, W.Y. Mental health and COVID-19: Policies, guidelines, and initiatives from the Asia-Pacific region. Asia Pac. J. Public Health 2021, 33, 839–846. [Google Scholar] [CrossRef] [PubMed]
- Hawton, K.; Casey, D.; Bale, E.; Brand, F.; Ness, J.; Waters, K.; Kelly, S.; Geulayov, G. Self-harm during the early period of the COVID-19 pandemic in England: Comparative trend analysis of hospital presentations. J. Affect. Disord. 2021, 282, 991–995. [Google Scholar] [CrossRef] [PubMed]
- Mariani Wigley, I.L.C.; Mascheroni, E.; Bulletti, F.; Bonichini, S. COPEWithME: The Role of Parental Ability to Support and Promote Child Resilient Behaviors during the COVID-19 Emergency. Front. Psychol. 2021, 12, 732745. [Google Scholar] [CrossRef] [PubMed]
- Suhail, A.; Dar, K.A.; Iqbal, N. COVID-19 related fear and mental health in Indian sample: The buffering effect of support system. Curr. Psychol. 2022, 41, 480–491. [Google Scholar] [CrossRef]
- Pellerin, N.; Raufaste, E.; Corman, M.; Teissedre, F.; Dambrun, M. Psychological resources and flexibility predict resilient mental health trajectories during the French COVID-19 lockdown. Sci. Rep. 2022, 12, 10674. [Google Scholar] [CrossRef]
- Bao, X.; Xu, J.; Meng, Q.; Gan, J.; Wang, X.D.; Wu, H.; Liu, S.; Ji, Y. Impact of the COVID-19 Pandemic and Lockdown on Anxiety, Depression and Nursing Burden of Caregivers in Alzheimer’s Disease, Dementia with Lewy Bodies and Mild Cognitive Impairment in China: A 1-Year Follow-up Study. Front. Psychiatry 2022, 13, 921535. [Google Scholar] [CrossRef]
- Khan, T.A.; Mohsin, A.; Din, S.; Qayum, S.; Farooqi, I. Last Honors and Life Experiences of Bereaved Families in the Context of COVID-19 in Kashmir: A Qualitative Inquiry About Exclusion, Family Trauma, and Other Issues. OMEGA-J. Death Dying 2022. [Google Scholar] [CrossRef]
- Costanza, A.; Macheret, L.; Folliet, A.; Amerio, A.; Aguglia, A.; Serafini, G.; Prada, P.; Bondolfi, G.; Sarasin, F.; Ambrosetti, J. COVID-19 Related Fears of Patients Admitted to a Psychiatric Emergency Department during and Post-Lockdown in Switzerland: Preliminary Findings to Look Ahead for Tailored Preventive Mental Health Strategies. Medicina 2021, 57, 1360. [Google Scholar] [CrossRef]
- Brandizzi, M.; Polselli, A.; Corigliano, V.; Tamorri, S.M.; Venturini, P.; Azzoni, A.; Grasso, S.; Onofri, A.; Pesce, S.; Romani, F.; et al. Psychiatric emergencies during, after, and before the COVID-19 lockdown: What happened to our patients? A naturalistic observational study. Ann. Gen. Psychiatry 2022, 21, 1–10. [Google Scholar] [CrossRef]
- Brindisi, G.; Di Marino, V.P.; Olivero, F.; De Canditiis, D.; De Castro, G.; Zicari, A.M.; Anania, C. Effects of COVID-19 lockdown on weight in a cohort of allergic children and adolescents. Ital. J. Pediatr. 2022, 48, 1–7. [Google Scholar] [CrossRef]
- Caballero-Apaza, L.M.; Vidal-Espinoza, R.; Curaca-Arroyo, S.; Gomez-Campos, R.; Callata-Gallegos, Z.; Fuentes-López, J.; Cossio-Bolaños, M. Bibliometric study of scientific productivity on the impacts on mental health in times of pandemic. Medicina 2021, 58, 24. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Yue, S.; Hu, X.; Zhu, J.; Wu, Z.; Wang, J.; Wu, Y. Associations between feelings/behaviors during COVID-19 pandemic lockdown and depression/anxiety after lockdown in a sample of Chinese children and adolescents. J. Affect. Disord. 2021, 284, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Gavin, B.; Lyne, J.; McNicholas, F. The global impact on mental health almost 2 years into the COVID-19 pandemic. Ir. J. Psychol. Med. 2021, 38, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Molnar, D.S.; Methot-Jones, T.; Moore, J.; O’Leary, D.D.; Wade, T.J. Perfectionistic cognitions pre-pandemic predict greater anxiety symptoms during the pandemic among emerging adults: A two-wave cross-lagged study. J. Ration.-Emotive Cogn. Behav. Ther. 2021, 40, 474–492. [Google Scholar] [CrossRef]
- Escudero-Castillo, I.; Mato-Díaz, F.J.; Rodriguez-Alvarez, A. Furloughs, teleworking and other work situations during the COVID-19 lockdown: Impact on mental well-being. Int. J. Environ. Res. Public Health 2021, 18, 2898. [Google Scholar] [CrossRef]
- Carlyle, M.; Leung, J.; Walter, Z.C.; Juckel, J.; Salom, C.; Quinn, C.A.; Davidson, L.; Ellem, R.; Newland, G.; Hides, L. Changes in Substance Use among People Seeking Alcohol and Other Drug Treatment during the COVID-19 Pandemic: Evaluating Mental Health Outcomes and Resilience. Subst. Abus. Res. Treat. 2021, 15, 11782218211061746. [Google Scholar] [CrossRef]
- Cui, Y.; Han, Y. The Impact of the COVID-19 Pandemic on the Mental Health of Urban Residents—Evidence from China. Int. J. Environ. Res. Public Health 2022, 19, 16190. [Google Scholar] [CrossRef]
- Wang, J.; Chen, Y.; Guo, X.; Lin, H.; Richards, M.; Wang, H.; Chen, X.; Fu, C. Impact of COVID-19 Related Knowledge and Precautions on Emotional and Behavioral Problems among Children during the Post-pandemic in China: The Explanatory Value of Emotional Problems among Caregivers. Front. Psychol. 2021, 12, 712529. [Google Scholar] [CrossRef]
- Xu, Z.; Fan, J.; Ding, J.; Feng, X.; Tao, S.; Zhou, J.; Qian, L.; Tao, K.; Hambly, B.D.; Bao, S. The Impact of COVID-19 on Primary care general practice consultations in a teaching hospital in Shanghai, China. Front. Med. 2021, 8, 642496. [Google Scholar] [CrossRef]
- Iodice, F.; Cassano, V.; Rossini, P.M. Direct and indirect neurological, cognitive, and behavioral effects of COVID-19 on the healthy elderly, mild-cognitive-impairment, and Alzheimer’s disease populations. Neurol. Sci. 2021, 42, 455–465. [Google Scholar] [CrossRef]
- Leonangeli, S.; Michelini, Y.; Montejano, G.R. Depression, anxiety and stress in college students before and during the first three months of COVID-19 lockdown. Rev. Colomb. Psiquiatr. 2022. [CrossRef]
- Hildersley, R.; Easter, A.; Bakolis, I.; Carson, L.; Howard, L.M. Changes in the identification and management of mental health and domestic abuse among pregnant women during the COVID-19 lockdown: Regression discontinuity study. BJPsych Open 2022, 8, e96. [Google Scholar] [CrossRef]
- Dodge, K.A.; Skinner, A.T.; Godwin, J.; Bai, Y.; Lansford, J.E.; Copeland, W.E.; Goodman, W.B.; McMahon, R.J.; Goulter, N.; Bornstein, M.H.; et al. Impact of the COVID-19 pandemic on substance use among adults without children, parents, and adolescents. Addict. Behav. Rep. 2021, 14, 100388. [Google Scholar] [CrossRef] [PubMed]
- Chatterji, S.; McDougal, L.; Johns, N.; Ghule, M.; Rao, N.; Raj, A. COVID-19-Related financial hardship, job loss, and mental health symptoms: Findings from a cross-sectional study in a rural agrarian community in India. Int. J. Environ. Res. Public Health 2021, 18, 8647. [Google Scholar] [CrossRef] [PubMed]
- Passarelli, M.; Casetta, L.; Rizzi, L.; Perrella, R.; Maniaci, G.; La Barbera, D. Changes in Touch Avoidance, Stress, and Anxiety During the COVID-19 Pandemic in Italy. Front. Psychol. 2022, 13, 854110. [Google Scholar] [CrossRef]
- Yang, L.; Yang, Z.; Xia, Y. Relationship between negative coping style and fear of COVID-19 among Wuhan college students during the post-pandemic period: A moderated chain mediation model. Front. Psychiatry 2022, 13, 994685. [Google Scholar] [CrossRef]
- Sempere, L.; Bernabeu, P.; Cameo, J.; Gutierrez, A.; Laveda, R.; García, M.F.; Aguas, M.; Zapater, P.; Jover, R.; Ruiz-Cantero, M.T.; et al. Evolution of the emotional impact in patients with early inflammatory bowel disease during and after COVID-19 lockdown. Gastroenterol. Hepatol. 2021, 45, 123–133. [Google Scholar] [CrossRef]
- Corley, J.; Okely, J.A.; Taylor, A.M.; Page, D.; Welstead, M.; Skarabela, B.; Redmond, P.; Cox, S.R.; Russ, T.C. Home garden use during COVID-19: Associations with physical and mental wellbeing in older adults. J. Environ. Psychol. 2021, 73, 101545. [Google Scholar] [CrossRef]
- Gorgoni, M.; Scarpelli, S.; Alfonsi, V.; Annarumma, L.; Pellegrini, E.; Fasiello, E.; Cordone, S.; D’atri, A.; Salfi, F.; Amicucci, G.; et al. The oneiric activity during and after the COVID-19 total lockdown in Italy: A longitudinal study. Int. J. Environ. Res. Public Health 2022, 19, 3857. [Google Scholar] [CrossRef]
- Mariani, R.; Renzi, A.; Di Monte, C.; Petrovska, E.; Di Trani, M. The impact of the COVID-19 pandemic on primary emotional systems and emotional regulation. Int. J. Environ. Res. Public Health 2021, 18, 5742. [Google Scholar] [CrossRef]
- Dewa, L.H.; Crandell, C.; Choong, E.; Jaques, J.; Bottle, A.; Kilkenny, C.; Lawrence-Jones, A.; Di Simplicio, M.; Nicholls, D.; Aylin, P. CCopeY: A mixed-methods coproduced study on the mental health status and coping strategies of young people during COVID-19 UK lockdown. J. Adolesc. Health 2021, 68, 666–675. [Google Scholar] [CrossRef] [PubMed]
- Sommerlad, A.; Marston, L.; Huntley, J.; Livingston, G.; Lewis, G.; Steptoe, A.; Fancourt, D. Social relationships and depression during the COVID-19 lockdown: Longitudinal analysis of the COVID-19 Social Study. Psychol. Med. 2022, 52, 3381–3390. [Google Scholar] [CrossRef] [PubMed]
- Fancourt, D.; Steptoe, A.; Bu, F. Trajectories of depression and anxiety during enforced isolation due to COVID-19: Longitudinal analyses of 59,318 adults in the UK with and without diagnosed mental illness. Lancet Psychiatry 2020, 8, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Jones, P.B.; Underwood, B.R.; Moore, A.; Bullmore, E.T.; Banerjee, S.; Osimo, E.F.; Deakin, J.B.; Hatfield, C.F.; Thompson, F.J.; et al. The early impact of COVID-19 on mental health and community physical health services and their patients’ mortality in Cambridgeshire and Peterborough, UK. J. Psychiatr. Res. 2020, 131, 244–254. [Google Scholar] [CrossRef] [PubMed]
- Pignon, B.; Gourevitch, R.; Tebeka, S.; Dubertret, C.; Cardot, H.; Dauriac-Le Masson, V.; Trebalag, A.K.; Barruel, D.; Yon, L.; Hemery, F.; et al. Dramatic reduction of psychiatric emergency consultations during lockdown linked to COVID-19 in Paris and suburbs. Psychiatry Clin. Neurosci. 2020, 74, 557. [Google Scholar] [CrossRef]
- Smalley, C.M.; Malone, D.A., Jr.; Meldon, S.W.; Borden, B.L.; Simon, E.L.; Muir, M.R.; Fertel, B.S. The impact of COVID-19 on suicidal ideation and alcohol presentations to emergency departments in a large healthcare system. Am. J. Emerg. Med. 2021, 41, 237. [Google Scholar] [CrossRef]
- Sasaki, Y.; Aida, J.; Tsuji, T.; Koyama, S.; Tsuboya, T.; Saito, T.; Kondo, K.; Kawachi, I. Pre-disaster social support is protective for onset of post-disaster depression: Prospective study from the Great East Japan Earthquake & Tsunami. Sci. Rep. 2019, 9, 19427. [Google Scholar]
- Elmer, T.; Mepham, K.; Stadtfeld, C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE 2020, 15, e0236337. [Google Scholar] [CrossRef]
- Chong, S.L.; Soo, J.S.L.; Allen, J.C.; Ganapathy, S.; Lee, K.P.; Tyebally, A.; Yung, C.F.; Thoon, K.C.; Ng, Y.H.; Oh, J.Y.; et al. Impact of COVID-19 on pediatric emergencies and hospitalizations in Singapore. BMC Pediatr. 2020, 20, 562. [Google Scholar] [CrossRef]
- Presti, G.; McHugh, L.; Gloster, A.; Karekla, M.; Hayes, S.C. The dynamics of fear at the time of COVID-19: A contextual behavioral science perspective. Clin. Neuropsychiatry 2020, 17, 65. [Google Scholar]
- Cimino, S.; Di Vito, P.; Cerniglia, L. The impact of COVID-19 pandemic on psychopathological symptoms in mothers and their school-age children before, during and after the COVID-19 pandemic peak. Curr. Psychol. 2022, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ezpeleta, L.; Navarro, J.B.; de la Osa, N.; Trepat, E.; Penelo, E. Life conditions during COVID-19 lockdown and mental health in Spanish adolescents. Int. J. Environ. Res. Public Health 2020, 17, 7327. [Google Scholar] [CrossRef] [PubMed]
- Allan, S.M.; Bealey, R.; Birch, J.; Cushing, T.; Parke, S.; Sergi, G.; Bloomfield, M.; Meiser-Stedman, R. The prevalence of common and stress-related mental health disorders in healthcare workers based in pandemic-affected hospitals: A rapid systematic review and meta-analysis. Eur. J. Psychotraumatol. 2020, 11, 1810903. [Google Scholar] [CrossRef] [PubMed]
- Anyan, F.; Hjemdal, O.; Ernstsen, L.; Havnen, A. Change in physical activity during the coronavirus disease 2019 lockdown in norway: The buffering effect of resilience on mental health. Front. Psychol. 2020, 11, 598481. [Google Scholar] [CrossRef] [PubMed]
- Kruizinga, M.D.; Peeters, D.; van Veen, M.; van Houten, M.; Wieringa, J.; Noordzij, J.G.; Bekhof, J.; Tramper-Stranders, G.; Vet, N.J.; Driessen, G.J. The impact of lockdown on pediatric ED visits and hospital admissions during the COVID19 pandemic: A multicenter analysis and review of the literature. Eur. J. Pediatr. 2021, 180, 2271–2279. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Pacitti, F.; Di Lorenzo, G.; Di Marco, A.; Siracusano, A.; Rossi, A. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw. Open 2020, 3, e2010185. [Google Scholar] [CrossRef]
- Marconcin, P.; Werneck, A.O.; Peralta, M.; Ihle, A.; Gouveia, É.R.; Ferrari, G.; Sarmento, H.; Marques, A. The association between physical activity and mental health during the first year of the COVID-19 pandemic: A systematic review. BMC Public Health 2022, 22, 209. [Google Scholar] [CrossRef]
- Cortese, S.; Sabé, M.; Chen, C.; Perroud, N.; Solmi, M. Half a century of research on Attention-Deficit/Hyperactivity Disorder: A scientometric study. Neurosci. Biobehav. Rev. 2022, 140, 104769. [Google Scholar] [CrossRef]
- Hicks, D.; Wouters, P.; Waltman, L.; De Rijcke, S.; Rafols, I. Bibliometrics: The Leiden Manifesto for research metrics. Nature 2015, 520, 429–431. [Google Scholar] [CrossRef]
- Nitschke, J.P.; Forbes, P.A.; Ali, N.; Cutler, J.; Apps, M.A.; Lockwood, P.L.; Lamm, C. Resilience during uncertainty? Greater social connectedness during COVID-19 lockdown is associated with reduced distress and fatigue. Br. J. Health Psychol. 2021, 26, 553–569. [Google Scholar] [CrossRef]
- Vincent, J.L.; Wendon, J.; Martin, G.S.; Juffermans, N.P.; Creteur, J.; Cecconi, M. COVID-19: What we’ve done well and what we could or should have done better—the 4 Ps. Crit. Care 2021, 25, 1–5. [Google Scholar] [CrossRef] [PubMed]
- George, I.; Salna, M.; Kobsa, S.; Deroo, S.; Kriegel, J.; Blitzer, D.; Shea, N.J.; D’Angelo, A.; Raza, T.; Kurlansky, P.; et al. The rapid transformation of cardiac surgery practice in the coronavirus disease 2019 (COVID-19) pandemic: Insights and clinical strategies from a centre at the epicentre. Eur. J. Cardio-Thorac. Surg. 2020, 58, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Simonelli, C.; Paneroni, M.; Fokom, A.G.; Saleri, M.; Speltoni, I.; Favero, I.; Garofali, F.; Scalvini, S.; Vitacca, M. How the COVID-19 infection tsunami revolutionized the work of respiratory physiotherapists: An experience from Northern Italy. Monaldi Arch. Chest Dis. 2020, 90, 292–298. [Google Scholar] [CrossRef] [PubMed]

