1. Introduction
Cardiovascular disease (CVD) includes all diseases that affect the cardiovascular system (the heart and blood vessels). CVD is the leading cause of disability and mortality globally [1] and accounts for the highest proportion (44%) of chronic non-communicable disease deaths annually [2] and 32% of all deaths globally [3,4]. CVDs are associated with severe social consequences, including reduced quality of life and economic growth, and consume many health service resources in developing and developed countries [5,6].
Annually, approximately 15 million people globally suffer a stroke [7], estimated to rise to 77 million by 2030 [8]. The cumulative risk of stroke recurrence at five years is 1.3%, and at ten years is 39.2% [9], with a higher death and disability rate associated with recurrent stroke [10]. Chronic non-communicable diseases are associated with multiple risk factors, including genetic and environmental factors, metabolic factors (hypertension, diabetes, abnormal lipids, obesity), and behavioural factors (tobacco use, unhealthy diet, physical inactivity) [11]. These risk factors are drivers of the global CVD epidemic [6,12]. A global study in 52 countries identified similar risk factors for heart diseases in low- and high-income countries [12]. However, over three-quarters of the global burden of CVD is from low- and middle-income countries (LMICs), with a rising incidence [13,14].
The effectiveness of lifestyle changes and physical interventions is well established in the primary, secondary, and tertiary prevention of CVDs [15,16]. Primary prevention aims to reduce the incidence of an index cardiovascular event, especially in at-risk people [11,17]. Secondary and tertiary prevention programmes are often provided at specialised cardiac rehabilitation centres and directed towards reducing the recurrence of cardiac events, restoring patients’ quality of life, improving functional capacity, stress, and self-management techniques, and promoting a healthy lifestyle [18]. There is evidence that cardiovascular mortality can be reduced and signs and symptoms of established CVD improved by addressing behavioural risk factors such as an unhealthy diet [19], physical inactivity [20], harmful use of alcohol [21], tobacco use [22], inadequate sleep [23], and poor stress management [3,24,25]. Adopting these preventive strategies may reduce the incidence of heart disease [26,27].
Physiotherapists play a role in reducing risk and managing patients at risk or with established CVD (pwCVDs) [28,29,30]. Despite the substantial burden of CVDs and the evidence supporting cardiac rehabilitation in preventing and managing CVDs, many LMICs do not have existing structures and programmes promoting the prevention and rehabilitation of pwCVDs [18,31,32]. Cardiac rehabilitation services are available in 80% of European countries, but only 17% of African countries [31]. It is therefore important to scale up rehabilitation for pwCVDs in accordance with the WHO call for action “Rehabilitation 20230 [33]. Cardiac rehabilitation services are rare in LMICs for several reasons, including lack of personnel resources, competing priorities, affordability issues, and insurance coverage [32]. Physiotherapists in LMIC settings receive pwCVDs in their practice, providing an opportunity to provide cardiac rehabilitation-related interventions through health prevention and promotion. The contact time and frequent visits make them well-placed to provide physiotherapy-led health promotion (PLHP). PLHP refers to the approach within the field of physiotherapy that focuses on promoting overall health and well-being through education, lifestyle modification, and preventive strategies beyond acute care [34]. Both promotive and preventive strategies, such as health education and the use of exercise in disease prevention and management, are at the core of physiotherapy practice. Given the rising incidence of CVDs and the lack of cardiac rehabilitation services in LMICs, it is essential that physiotherapists from these countries are able to deliver health promotion strategies effectively given the lack of advanced treatment opportunities for these patients. However, no evidence exists to inform or enhance PLHP practice globally.
Previous reviews on PLHP are limited and focused on health education strategies for lifestyle-related conditions in general [35], promoting physical activities [28,36], entry-level training and physical activity promotion [36], and physical activity in cystic fibrosis patients [37]. There are no reviews investigating PLHP strategies for pwCVDs. Consequently, a review is warranted to systematically scope and map out the existing evidence in this area. This review summarises the available literature with the following objectives:
- To assess the characteristics of existing evidence on PLHP for pwCVDs globally.
- To identify the interventional approaches that have been used in PLHP strategies for pwCVDs.
- To evaluate the type of population groups included in the PLHP research.
2. Methodology
A scoping review was used to identify and synthesise data on PHLP strategies and interventions in the literature and map existing evidence’s characteristics without critically appraising the methodological quality [38,39]. The methodological framework published by Arksey and O’Malley and the methodological advancement by Levac and colleagues were adopted for this study [40,41]. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR) recommendations were used for reporting this systematic scoping review [42,43]. The proposed stages in this framework are: (1) Identifying the research questions, (2) identifying relevant studies, (3) study selection, (4) charting the data, and (5) collating, summarising and reporting [41]. The template for intervention description and replication (TIDieR) framework was used to extract intervention data from the included studies. The study protocol was registered on the Open Science Frame (OSF) (OSF.IO/BFZ6Y). This review involved no direct contact with patients or healthcare professionals but reviewed and synthesised already-published data, and therefore was not subject to ethical approval.
2.1. Identifying the Research Question
Scoping review questions are generally broad and aim to summarise the available evidence of interest [43]. Based on the overall project aims, the following questions were identified for the present study: (1) What are the characteristics of existing evidence of PLHP for pwCVDs globally? (2) What interventional approaches have been used in PLHP strategies for pwCVDs globally? (3) What population groups have been included in the PLHP research globally?
2.2. Identifying Relevant Studies (Database and Search Strategy)
The following electronic databases, registries, and search engines were searched for eligible articles from the inception of the database to June 2023: MEDLINE, PubMed Web of Science, Cochrane Central Register of Controlled Trials, EMBASE, CINAHL, PEDro, Google Scholar, the EU clinical trial register, African Index Medicus, World Physiotherapy Conference proceedings, trials registries, and the World Health Organisation International Clinical Trials Registry Platform portal. A search strategy that considered relevant index terms and keywords was developed with assistance from an experienced librarian from Sheffield Hallam University . A subject librarian at Sheffield Hallam University further reviewed this. The search strategy for MEDLINE (final) was adapted for searches in other included databases. Search filters such as publication in the English language, human species, and primary studies were used in relevant databases. References to identified previous and adjacent reviews and included papers were also screened. A complete MEDLINE search strategy can be found in .
2.3. Eligibility Criteria
Studies were included if they reported or evaluated health promotion for pwCVDs, were led by physiotherapists, and were published in English. Studies with a focus on specific clinical or therapeutic outcomes rather than health promotion were excluded. Details on inclusion and exclusion criteria are provided in .
2.4. Study Selection (Screening)
Studies identified through searches were imported to Covidence, and duplicates were removed. Two independent reviewers (ENN, CG) individually screened studies using a three-step process: First titles, then abstracts (Cohen’s kappa score = 0.43), and finally, full text was screened based on the inclusion and exclusion criteria . The full texts of selected studies were reviewed in detail against the inclusion criteria by two independent reviewers (Cohen’s kappa score = 0.35) (ENN, SM). All reasons for excluding potential studies that did not meet the inclusion criteria are reported on the PRISMA flowchart. Any disagreements between the reviewers at each stage of the study selection process were resolved through discussion, and where an agreement was not met, a third reviewer (AL) was consulted.
2.5. Data Charting (Data Extraction)
Data charting is the method for extracting data for scoping reviews [40,42]. The chart included information about study participants and the design. Data about the nature of the intervention(s) were extracted based on the TIDieR framework, including the theoretical framework (why), intervention type (what), intervention duration (when), intervention provider (who), delivery format (how), intervention location (where), number of intervention sessions (how much), personalised intervention (tailoring), and fidelity (how well). Intervention duration of less than 12 months was described as short and more than 12 months as long. Total intervention sessions less than 15 sessions and 16 sessions and above were described as low and high volume, respectively. In cases of missing data or insufficiently described processes, the corresponding authors were contacted to clarify or provide the missing information. Screening and data extraction were completed in Covidence.
2.6. Quality Appraisal
Based on current guidance for conducting scoping reviews, quality appraisal was not considered necessary to achieve the aims of this study [40,43].
2.7. Consultation
We consulted relevant stakeholders, experts in the field, and key informants in the later stages of this review to clarify missing information, identify relevant studies that are ongoing, or identify interventions/concepts not considered in the review [44].
2.8. Collating, Summarising, and Reporting
Results are synthesised narratively and presented in a table format based on elements of the TIDier framework.
3. Results
3.1. Literature Search and Included Studies
The PRISMA flow chart (Figure 1) summarises search results and the methodological steps to arrive at the included studies. The search yielded 4381 articles with the respective numbers for each database, as shown on the PRISMA flow chart (Figure 1). After removing the duplicates, 1716 studies remained and were screened for eligibility. After screening titles and abstracts, 227 articles were deemed potentially eligible. Following full-text screening, 20 studies were included in this review. Reasons for exclusions are documented on the PRISMA flow chart.
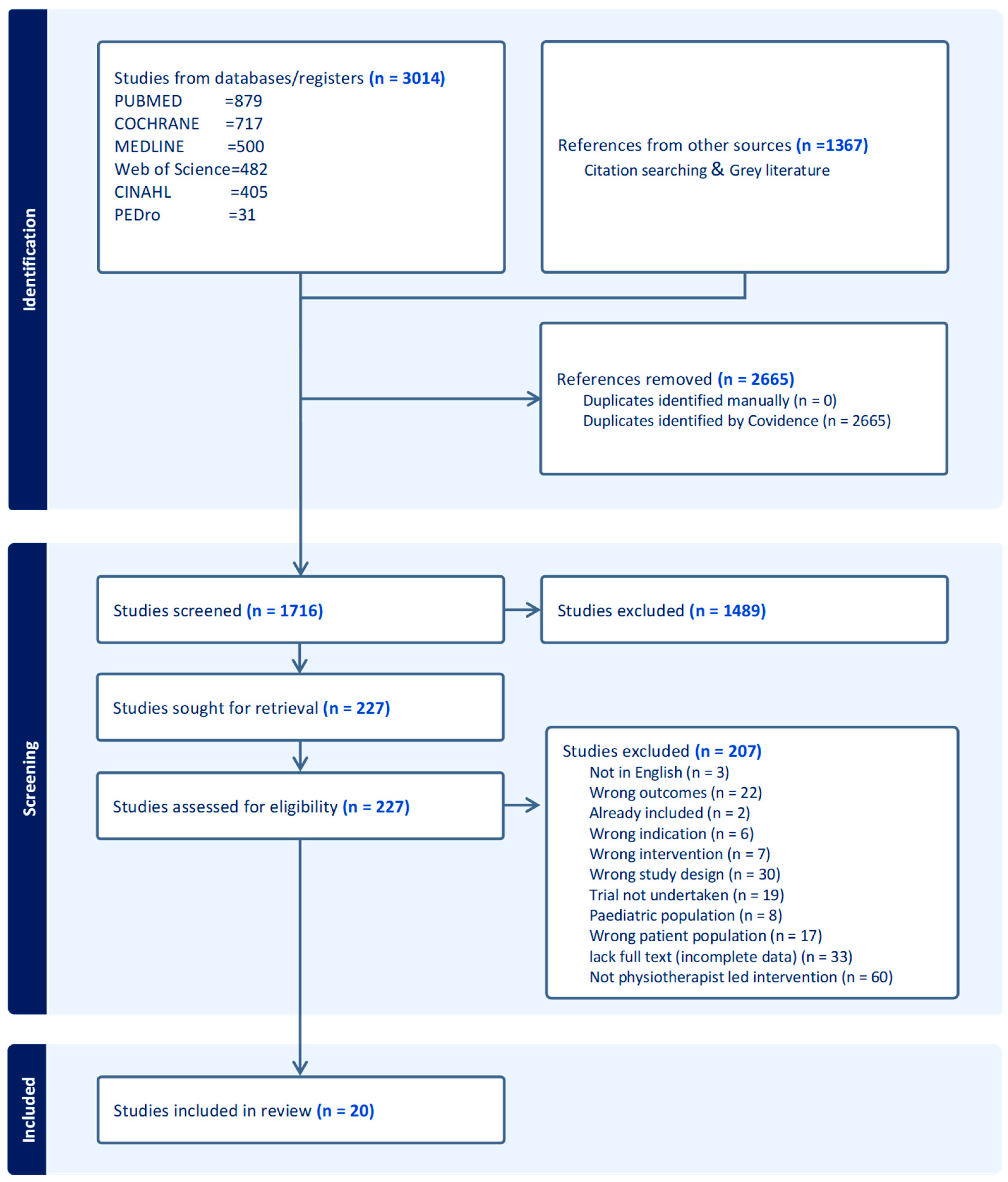
Figure 1. PRISMA flow chart for searches.
3.2. Characteristics of Included Studies
summarises the characteristics of the included studies. Of the twenty included studies, 12 were randomised controlled trials (RCTs) [45,46,47,48,49,50,51,52,53,54,55,56], seven were quasi-experimental studies [57,58,59,60,61,62,63], and one was a secondary analysis of trial data. All included studies were published between 2002 and 2022. Thirty percent of the included studies were published between 2016 and 2020 [55,57,58,59,64,65]. Studies were conducted on patients with stroke (n = 4) [53,57,58,59], risk factors for CVD (n = 4) [47,50,54,62], coronary heart diseases (n = 3) [51,52,63], peripheral arterial diseases (n = 2) [45,56], diabetes (n = 3) [48,52,60], weight/obesity (n = 2) [49,61], and hypertension (n = 2) [46,55]. The sample size of the included studies ranged from 18 to 882 participants [45,46]. The included studies were conducted in 15 countries, with England [56,61], Australia [45,57], Spain [46,63], The Netherlands [48,49], and Norway [58,64] having two studies each and the remaining countries having one study each . The majority of studies were from high-income countries (HICs), with 47% from Europe alone, and only two publications [54,55] from two LMICs (Brazil and China). No studies were identified from the African continent.
3.3. Characteristics of the Included Interventions
All studies were either solely implemented by physiotherapists (n=13) [45,46,48,50,52,53,54,55,56,57,58,59,61] or in combination with other healthcare professionals (nurses, physicians, and dieticians/nutritionists), with physiotherapists leading defined components of the intervention (n = 7) [47,49,54,60,62,63,65]. The identified interventions were heterogeneous and reported according to the TIDieR framework in . 85% of studies used multimodal intervention strategies, with only 15% of studies using a single intervention strategy [46,51,56]. Seven (35%) of the 20 publications employed behaviour change approaches and psychological models such as the theory of planned behaviour and the common-sense model of illness representations (n = 1) [56], health belief model and transtheoretical model to promote participant exercise behaviours (n = 1) [50], Bandura’s self-efficacy theory (n = 1) [63], and motivational interviewing (n = 4) [51,56,58,62]. The majority of interventions included exercise or physical activity (n = 18), education on lifestyle (n = 2) [52,59], and dietary education in combination with another physiotherapists’ led intervention (n = 6) [47,49,50,52,55,63]. Seven studies employed behaviour change programmes focused on physical activity uptake (n = 5) [51,56,57,61,63] and diabetes management (n = 2) [55,60] with only two underpinned by behaviour change theory [56,63]. Self-management and home programmes were also identified (n = 4) [48,52,57,62]. Individualised coaching on physical activity and exercise (n = 5) [49,58,60,62,64] and use of the health improvement card (HIC) (n = 1) [54] were also used by physiotherapists to enhance activity and reduce cardiovascular risks, with only two studies (n = 2) reporting employing behavioural change techniques [62,64]. Six studies were characterised by the provision of educational materials/resources, including brochures on healthy lifestyle practices and lifestyle behaviour change (n = 2) [45,54], written instructions and recommendations (n = 2) [47,59], workbooks (n = 1) [55], and handouts following each session (n = 1) [61]. Technology-based strategies were also used to deliver interventions for weight management (video-conferencing sessions with real-time communications and the use of remote monitoring using Fitbit) (n = 1) [60], video/television programme called Sit and Be Fit during the exercise phase (n = 1) [62], and videos on specific exercises and techniques (n = 1) [50]). Six studies were supplemented by telephone calls (n = 6) [48,50,51,52,56,58]. Adherence to interventions was reported in nine studies [49,50,56,57,58,59,60,62,63].
4. Discussion
This review identified the nature of the evidence and the types of interventions used and implemented by physiotherapists for pwCVDs within their scope of practice. This involved opportunistic advice, discussions, encouragement, and strategies that physiotherapists are able to use for disease prevention and health promotion within their profession in addition to their therapeutic role. While health promotion and therapeutic interventions are within the scope of physiotherapy practice, much attention has not been given to physiotherapy health promotion globally. This is the first review explicitly exploring PLHP for pwCVDs globally, providing an opportunity for discussion and future research in this area.
No grey literature was found, and all included studies were published between 2002 and 2022. Given that there were no restrictions in the search period, this is a small volume of literature. This could be explained in two ways. Firstly, the inclusion was based on physiotherapists leading or implementing the intervention, focusing on primary and secondary prevention of CVDs to heart disease risk factors. Based on this criterion, many studies were excluded as not physiotherapist led (n = 60) (Figure 1). Secondly, earlier attention to physiotherapists’ interventions was directed towards therapeutic and curative treatment rather than prevention. Over the last two decades, physiotherapy preventive roles have been increasing with the rising burden of CVDS [65,66]. This aligns with the global call for physiotherapists to contribute to preventing lifestyle-related conditions [65,66,67]. The increasing trend in research output indicates that more evidence will emerge in the coming years as physiotherapists gain skills and autonomy in leading prevention programmes.
Currently, most studies have emerged from Europe (55%), with no studies from the African continent. Given the vast burden of CVDs in African countries with unique ethnic, cultural, and context-specific determinants [68,69] and the lack of CR programmes on this continent [31,70], it is essential to see more research investigating PLHP for pwCVDs in African countries to facilitate effective preventive interventions. Only two studies (10%) from LMICs were included in this review, and both were supported with research funding [54,55]. Generally, PLHP research may be difficult to realise in LMIC settings due to a lack of research priorities, funding problems, and a lack of infrastructure and researchers with relevant skills [71,72]. Addressing funding issues by budgeting for the prevention of NCDs in LMICs, among other potential barriers, may contribute positively to data generation for pwCVDs in low-resource settings.
Many of the included studies were RCTs (60%), followed by different quasi-experimental designs (35%). The available data provides an opportunity for follow-up studies, such as a systematic review of effectiveness. This is necessary to determine whether PLHPs are effective for wider-scale adoption. No qualitative work on PLHP was identified, and there is a gap in our understanding of patient perceptions and experiences of PLHP approaches. More research is necessary for designing and implementing PLHP in the future.
Diverse interventional approaches have been used in PLHP for pwCVDs . CVD PLHP interventions are likely to be complex, and therefore require a multimodal approach, due to different populations, multiple risk factors for CVD, and non-adherence to recommendations for managing these risk factors [66]. This review included studies focused mainly on exercise and physical activity uptake, weight management, and diet. Other components of health promotion for pwCVDs, such as sleep hygiene, smoking cessation, and alcohol abuse, among others, were not reported. These components are within the scope of physiotherapists, and it is necessary that physiotherapists receive adequate training that can enable them to confidently tackle the multiple risk factors associated with CVD. Qualified physiotherapists should be familiar with assessment tools related to general health measures, lifestyle-related behaviours, and NCD risk factors in general, including how to assess self-efficacy for behaviour change and readiness to change a lifestyle behaviour [65,66]. This should include counselling skills and the use of behaviour change strategies for specific populations. Physiotherapists should work in synergy with other health professions, making appropriate referrals and identifying relevant resources to improve outcomes.
Three studies employed theory-based behaviour change models supported by evidence-based behaviour change techniques such as motivational interviewing to inform and complement their interventions. These behaviour change theories and techniques were adopted in more recent studies published between 2011 and 2022. This indicates an increased understanding of the importance of including behaviour change techniques and theories for effective health education to strengthen patients’ motivation and adherence during and beyond the active rehabilitation period. More rigorous, theoretically informed approaches to support behaviour change for pwCVDs should be included in intervention strategies that facilitate change in lifestyle risk factors. This is also necessary in clinical practice and should be integrated into physiotherapy training [66]. In delivering broad health promotion strategies for pwCVDs, physiotherapists need to receive broader training in addressing these risk factors.
4.1. Implications for Clinical Practice
It is sensible to consider PLHP strategies incorporating interventions beyond exercise and physical activity. Understanding and increasing competence in implementing behaviour change in stress management, sleep, nutrition, and weight management through appropriate strategies is necessary for effective PLHP. Dean and colleagues highlighted the need to raise the priority of lifestyle prevention strategies for NCDs [67] and competency standards, including relevant behaviour change approaches [66], to improve practice adequately. Considering the different study populations and the multiple risk factors addressed in the included studies, it is necessary that physiotherapists collaborate with other healthcare providers to optimise health promotion and prevention programmes. Digital and technological monitoring and other interventions have been used successfully in some trials and contexts [60,73]. This can be useful in other contexts while considering local challenges and possible barriers.
4.2. Research Implications
The findings of this review demonstrate the lack of studies from Africa and other LMICs, which is concerning given the rising burden of pwCVDs in these regions. For effective interventions to be developed, it is necessary to consider increasing research output in these contexts.
PLHP interventions ought to be multimodal, theoretically informed and supported by behaviour change theories and techniques and delivered by physiotherapists who have been adequately trained and, where necessary, optimised by appropriate health care professionals who complement the physiotherapists’ skills and knowledge. These optimised interventions should also be reported in further trials following the TIDier framework. There is no evidence to characterise the optimal intensity and critical characteristics of weight management programmes for specific populations.
Findings highlight the increased use of digital technology at different levels of PLHP interventions with varied levels of adherence [60,62]. Digital or technological devices that are attractive, affordable, easy to use, and sensitive to specific outcomes in different contexts for better adherence and output should be considered.
Most of the included trials reported short-term follow-up. Despite the prevailing challenges, PLHP interventions are warranted to demonstrate longer-term clinical outcomes.
4.3. Strengths and Limitations
Scoping reviews provide breadth and the inclusion of all study designs, which makes this realistic about a topic. This study employed the recommended guidelines for conducting a scoping review with multiple reviewers for data screening and extraction, making the findings rigorous. The broad scope provides a complete overview of PLHP, which has been trialled in primary, secondary, and tertiary health promotion in low- and high-income countries. This provides researchers with clear directions about developing the PLHP based on evidence and where further research needs to be undertaken. Additionally, the results of this scoping review may apply to clinicians employing the identified strategies/approaches as CVDs and their risk factors share and pose similar risks to other CNCDs. This review considers only literature published in English. This might have limited the scope of this review to articles published in or from non-English-speaking countries.
5. Conclusions
Based on the literature, physiotherapists are trying to address the growing burden of CVDs through various PLHP strategies. PLHP strategies are focused on exercise and physical activity, and there is a need to tackle CVD beyond addressing sedentary behaviour, considering the multiple risk factors. Assessing the risks and needs, tailoring the interventions to individuals, and monitoring appear central and consistent with practical preventive principles and strategies. It is crucial that physiotherapists work together with other healthcare professionals to optimise relevant components of health promotion effectively. Health behaviour change theories and techniques should be commonly used to support positive health behaviour change, and it may be necessary to provide comprehensive training to integrate lifestyle management approaches in physiotherapy practice. This is even more compelling for physiotherapy practice in Africa and LMICs with huge CVD burdens. Further study is needed to elucidate the effectiveness of existing PLHP interventions for pwCVDs. Avenues for future research have been highlighted.
References
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practiceThe Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef]
- Non Communicable Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 19 July 2021).
- Tulu, S.N.; Al Salmi, N.; Jones, J. Understanding cardiovascular disease in day-to-day living for African people: A qualitative metasynthesis. BMC Public Health 2021, 21, 745. [Google Scholar] [CrossRef] [PubMed]
- Cardiovascular Diseases (CVDs). Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 21 November 2021).
- Gaziano, T.A. Reducing the Growing Burden of Cardiovascular Disease in The Developing World. Health Aff. 2007, 26, 13–24. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.J.; Chin, S.L.; Rangarajan, S.; Xavier, D.; Liu, L.; Zhang, H.; Rao-Melacini, P.; Zhang, X.; Pais, P.; Agapay, S.; et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): A case-control study. Lancet 2016, 388, 761–775. [Google Scholar] [CrossRef] [PubMed]
- Feigin, V.L.; Roth, G.A.; Naghavi, M.; Parmar, P.; Krishnamurthi, R.; Chugh, S.; Mensah, G.A.; Norrving, B.; Shiue, I.; Ng, M.; et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016, 15, 913–924. [Google Scholar] [CrossRef] [PubMed]
- Strong, K.; Mathers, C.; Bonita, R. Preventing stroke: Saving lives around the world. Lancet Neurol. 2007, 6, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Mohan, K.M.; Wolfe, C.D.A.; Rudd, A.G.; Heuschmann, P.U.; Kolominsky-Rabas, P.L.; Grieve, A.P. Risk and Cumulative Risk of Stroke Recurrence: A Systematic Review and Meta-Analysis. Stroke 2011, 42, 1489–1494. [Google Scholar] [CrossRef] [PubMed]
- Dhamoon, M.S.; Sciacca, R.R.; Rundek, T.; Sacco, R.L.; Elkind, M.S.V. Recurrent stroke and cardiac risks after first ischemic stroke: The Northern Manhattan Study. Neurology 2006, 66, 641–646. [Google Scholar] [CrossRef]
- Ruan, Y.; Guo, Y.; Zheng, Y.; Huang, Z.; Sun, S.; Kowal, P.; Shi, Y.; Wu, F. Cardiovascular disease (CVD) and associated risk factors among older adults in six low-and middle-income countries: Results from SAGE Wave 1. BMC Public Health 2018, 18, 778. [Google Scholar] [CrossRef]
- Yusuf, S.; Hawken, S.; Ôunpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J.; et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- Bigna, J.J.; Noubiap, J.J. The rising burden of non-communicable diseases in sub-Saharan Africa. Lancet Glob. Health 2019, 7, e1295–e1296. [Google Scholar] [CrossRef] [PubMed]
- Bowry, A.D.K.; Lewey, J.; Dugani, S.B.; Choudhry, N.K. The Burden of Cardiovascular Disease in Low- and Middle-Income Countries: Epidemiology and Management. Can. J. Cardiol. 2015, 31, 1151–1159. [Google Scholar] [CrossRef] [PubMed]
- 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease—American College of Cardiology. Available online: https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2019/03/07/16/00/2019-acc-aha-guideline-on-primary-prevention-gl-prevention (accessed on 15 August 2020).
- Li, D.; Jia, Y.; Yu, J.; Liu, Y.; Li, F.; Liu, Y.; Wu, Q.; Liao, X.; Zeng, Z.; Wan, Z.; et al. Adherence to a Healthy Lifestyle and the Risk of All-Cause Mortality and Cardiovascular Events in Individuals with Diabetes: The ARIC Study. Front. Nutr. 2021, 8, 698608. [Google Scholar] [CrossRef] [PubMed]
- Schuett, K.A.; Lehrke, M.; Marx, N.; Burgmaier, M. High-Risk Cardiovascular Patients: Clinical Features, Comorbidities, and Interconnecting Mechanisms. Front. Immunol. 2015, 6, 591. [Google Scholar] [CrossRef] [PubMed]
- Bellmann, B.; Lin, T.; Greissinger, K.; Rottner, L.; Rillig, A.; Zimmerling, S. The Beneficial Effects of Cardiac Rehabilitation. Cardiol. Ther. 2020, 9, 35–44. [Google Scholar] [CrossRef]
- Dietary Restrictions and Nutrition in the Prevention and Treatment of Cardiovascular Disease|Circulation Research. Available online: https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.118.313352 (accessed on 1 August 2021).
- Darden, D.; Richardson, C.; Jackson, E.A. Physical Activity and Exercise for Secondary Prevention among Patients with Cardiovascular Disease. Curr. Cardiovasc. Risk Rep. 2013, 7, 411–416. [Google Scholar] [CrossRef]
- Smyth, A.; Teo, K.K.; Rangarajan, S.; O’Donnell, M.; Zhang, X.; Rana, P.; Leong, D.P.; Dagenais, G.; Seron, P.; Rosengren, A.; et al. Alcohol consumption and cardiovascular disease, cancer, injury, admission to hospital, and mortality: A prospective cohort study. Lancet 2015, 386, 1945–1954. [Google Scholar] [CrossRef]
- Tobacco Smoking and Risk of 36 Cardiovascular Disease Subtypes: Fatal and Non-Fatal Outcomes in a Large Prospective Australian Study|BMC Medicine|Full Text. Available online: https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-019-1351-4 (accessed on 1 August 2021).
- Nagai, M.; Hoshide, S.; Kario, K. Sleep Duration as a Risk Factor for Cardiovascular Disease—A Review of the Recent Literature. CCR 2010, 6, 54–61. [Google Scholar] [CrossRef]
- Gomes, M.J.; Pagan, L.U.; Okoshi, M.P. Non-Pharmacological Treatment of Cardiovascular Disease|Importance of Physical Exercise. Arq. Bras. Cardiol. 2019, 113, 9–10. [Google Scholar] [CrossRef]
- How Is Stress and Heart Disease Related?—Cleveland Clinic. Available online: https://health.clevelandclinic.org/how-is-stress-and-heart-disease-related/ (accessed on 1 August 2021).
- Kisling, L.A.; Das, J.M. Prevention Strategies. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. Available online: http://www.ncbi.nlm.nih.gov/books/NBK537222/ (accessed on 10 August 2021).
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. J. Am. Coll. Cardiol. 2019, 74, e177–e232. [Google Scholar] [CrossRef]
- Lowe, A.; Gee, M.; McLean, S.; Littlewood, C.; Lindsay, C.; Everett, S. Physical activity promotion in physiotherapy practice: A systematic scoping review of a decade of literature. Br. J. Sports Med. 2018, 52, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Korn, L.; Ben-Ami, N.; Azmon, M.; Einstein, O.; Lotan, M. Evaluating the Effectiveness of a Health Promotion Intervention Program Among Physiotherapy Undergraduate Students. Med. Sci. Monit. 2017, 23, 3518–3527. [Google Scholar] [CrossRef] [PubMed]
- Maguire, A. Physiotherapy and Cardiovascular Disease: What Can It Do to Help? Ballsbridge Physiotherapy Clinic. 2015. Available online: https://ballsbridgephysio.ie/news/physiotherapy-and-cardiovascular-disease-what-can-it-do-to-help/ (accessed on 10 August 2021).
- Turk-Adawi, K.; Supervia, M.; Lopez-Jimenez, F.; Pesah, E.; Ding, R.; Britto, R.R.; Bjarnason-Wehrens, B.; Derman, W.; Abreu, A.; Babu, A.S.; et al. Cardiac Rehabilitation Availability and Density around the Globe. EClinicalMedicine 2019, 13, 31–45. [Google Scholar] [CrossRef]
- Ragupathi, L.; Stribling, J.; Yakunina, Y.; Fuster, V.; McLaughlin, M.A.; Vedanthan, R. Availability, Use, and Barriers to Cardiac Rehabilitation in LMIC. Glob. Heart 2017, 12, 323. [Google Scholar] [CrossRef] [PubMed]
- Gimigliano, F.; Negrini, S. The World Health Organization “Rehabilitation 2030: A call for action”. Eur. J. Phys. Rehabil. Med. 2017, 53, 155–168. [Google Scholar] [CrossRef] [PubMed]
- Bäck, M.; Öberg, B.; Krevers, B. Important aspects in relation to patients’ attendance at exercise-based cardiac rehabilitation—Facilitators, barriers and physiotherapist’s role: A qualitative study. BMC Cardiovasc. Disord. 2017, 17, 77. [Google Scholar] [CrossRef] [PubMed]
- Alexander, J.; Bambury, E.; Mendoza, A.; Reynolds, J.; Veronneau, R.; Dean, E. Health education strategies used by physical therapists to promote behaviour change in people with lifestyle-related conditions: A systematic review. Hong Kong Physiother. J. 2012, 30, 57–75. [Google Scholar] [CrossRef]
- Kunstler, B.E.; Cook, J.L.; Freene, N.; Finch, C.F.; Kemp, J.L.; O’Halloran, P.D.; Gaida, J.E. Physiotherapists use a small number of behaviour change techniques when promoting physical activity: A systematic review comparing experimental and observational studies. J. Sci. Med. Sport 2018, 21, 609–615. [Google Scholar] [CrossRef]
- Cox, N.S.; Alison, J.A.; Holland, A.E. Interventions for promoting physical activity in people with cystic fibrosis. Cochrane Database Syst. Rev. 2013, 2022, CD009448. [Google Scholar] [CrossRef]
- Lockwood, C.; Dos Santos, K.B.; Pap, R. Practical Guidance for Knowledge Synthesis: Scoping Review Methods. Asian Nurs. Res. 2019, 13, 287–294. [Google Scholar] [CrossRef]
- Munn, Z.; Stern, C.; Aromataris, E.; Lockwood, C.; Jordan, Z. What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med. Res. Methodol. 2018, 18, 5. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Social. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Implement. 2021, 19, 3–10. [Google Scholar] [CrossRef]
- Daudt, H.M.; van Mossel, C.; Scott, S.J. Enhancing the scoping study methodology: A large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med. Res. Methodol. 2013, 13, 48. [Google Scholar] [CrossRef]
- Fowler, B.; Jamrozik, K.; Norman, P.; Allen, Y.; Wilkinson, E. Improving maximum walking distance in early peripheral arterial disease: Randomised controlled trial. Aust. J. Physiother. 2002, 48, 269–275. [Google Scholar] [CrossRef]
- Bonet, J.; Coll, R.; Rocha, E.; Romero, R. Supervised versus recommended physical exercise in hypertensive women. Is its recommendation enough? Blood Press. 2003, 12, 139–144. [Google Scholar] [CrossRef]
- Eriksson, K.M.; Westborg, C.; Eliasson, M.C.E. A randomized trial of lifestyle intervention in primary healthcare for the modification of cardiovascular risk factors. Scand. J. Public. Health 2006, 34, 453–461. [Google Scholar] [CrossRef]
- Wisse, W.; Boer Rookhuizen, M.; de Kruif, M.D.; van Rossum, J.; Jordans, I.; ten Cate, H.; van Loon, L.J.C.; Meesters, E.W. Prescription of physical activity is not sufficient to change sedentary behavior and improve glycemic control in type 2 diabetes patients. Diabetes Res. Clin. Pract. 2010, 88, e10–e13. [Google Scholar] [CrossRef]
- Molenaar, E.A.; van Ameijden, E.J.C.; Vergouwe, Y.; Grobbee, D.E.; Numans, M.E. Effect of nutritional counselling and nutritional plus exercise counselling in overweight adults: A randomized trial in multidisciplinary primary care practice. Fam. Pract. 2010, 27, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.-T.; Hwang, C.-L.; Chen, C.-N.; Chuang, L.-M. Home-based exercise improves exercise behavior and metabolic risk factors in middle-aged adults at diabetic risk. Physiotherapy 2011, 97, eS523. [Google Scholar] [CrossRef]
- Reid, R.D.; Morrin, L.I.; Higginson, L.A.J.; Wielgosz, A.; Blanchard, C.; Beaton, L.J.; Nelson, C.; McDonnell, L.; Oldridge, N.; Wells, G.A.; et al. Motivational counselling for physical activity in patients with coronary artery disease not participating in cardiac rehabilitation. Eur. J. Prev. Cardiol. 2012, 19, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Oerkild, B.; Frederiksen, M.; Hansen, J.F.; Prescott, E. Home-based cardiac rehabilitation is an attractive alternative to no cardiac rehabilitation for elderly patients with coronary heart disease: Results from a randomised clinical trial. BMJ Open 2012, 2, e001820. [Google Scholar] [CrossRef] [PubMed]
- Takatori, K.; Matsumoto, D.; Okada, Y.; Nakamura, J.; Shomoto, K. Effect of intensive rehabilitation on physical function and arterial function in community-dwelling chronic stroke survivors. Top. Stroke Rehabil. 2012, 19, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Wu, X.; Tsang, R.C.; Yun, R.; Lu, Y.; Dean, E.; Jones, A.Y. A Randomised Controlled Trial to Evaluate the Administration of the Health Improvement Card as a Health Promotion Tool: A Physiotherapist-Led Community-Based Initiative. Int. J. Environ. Res. Public Health 2020, 17, 8065. [Google Scholar] [CrossRef]
- Gerage, A.M.; Benedetti, T.R.B.; Cavalcante, B.R.; Farah, B.Q.; Ritti-Dias, R.M. Efficacy of a behavior change program on cardiovascular parameters in patients with hypertension: A randomized controlled trial. Einstein 2020, 18, eAO5227. [Google Scholar] [CrossRef]
- Bearne, L.M.; Volkmer, B.; Peacock, J.; Sekhon, M.; Fisher, G.; Galea Holmes, M.N.; Douiri, A.; Amirova, A.; Farran, D.; Quirke-McFarlane, S.; et al. Effect of a Home-Based, Walking Exercise Behavior Change Intervention vs Usual Care on Walking in Adults with Peripheral Artery Disease: The MOSAIC Randomized Clinical Trial. JAMA 2022, 327, 1344–1355. [Google Scholar] [CrossRef]
- Preston, E.; Dean, C.M.; Ada, L.; Stanton, R.; Brauer, S.; Kuys, S.; Waddington, G. Promoting physical activity after stroke via self-management: A feasibility study. Top. Stroke Rehabil. 2017, 24, 353–360. [Google Scholar] [CrossRef]
- Gunnes, M.; Langhammer, B.; Aamot, I.-L.; Lydersen, S.; Ihle-Hansen, H.; Indredavik, B.; Reneflot, K.H.; Schroeter, W.; Askim, T.; LAST Collaboration group. Adherence to a Long-Term Physical Activity and Exercise Program After Stroke Applied in a Randomized Controlled Trial. Phys. Ther. 2019, 99, 74–85. [Google Scholar] [CrossRef]
- Higgs, C.; Skinner, M.; Hale, L. Outcomes of a community-based lifestyle programme for adults with diabetes or pre-diabetes. J. Prim. Health Care 2016, 8, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Pariser, G.; Ann Demeuro, M.; Gillette, P.; Stephen, W. Outcomes of an Education and Exercise Program for Adults with Type 2 Diabetes, and Comorbidities that Limit their Mobility: A Preliminary Project Report. Cardiopulm. Phys. Ther. J. 2010, 21, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Quinn, A.; Doody, C.; O’Shea, D. The effect of a physical activity education programme on physical activity, fitness, quality of life and attitudes to exercise in obese females. J. Sci. Med. Sport 2008, 11, 469–472. [Google Scholar] [CrossRef] [PubMed]
- Batsis, J.A.; Petersen, C.L.; Clark, M.M.; Cook, S.B.; Lopez-Jimenez, F.; Al-Nimr, R.I.; Pidgeon, D.; Kotz, D.; Mackenzie, T.A.; Bartels, S.J. A Weight Loss Intervention Augmented by a Wearable Device in Rural Older Adults with Obesity: A Feasibility Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2021, 76, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Deka, P.; Blesa, J.; Pathak, D.; Sempere-Rubio, N.; Iglesias, P.; Micó, L.; Soriano, J.M.; Klompstra, L.; Marques-Sule, E. Combined Dietary Education and High-Intensity Interval Resistance Training Improve Health Outcomes in Patients with Coronary Artery Disease. Int. J. Environ. Res. Public Health 2022, 19, 1402. [Google Scholar] [CrossRef]
- Gunnes, M.; Indredavik, B.; Langhammer, B.; Lydersen, S.; Ihle-Hansen, H.; Dahl, A.E.; Askim, T. Associations Between Adherence to the Physical A ctivity and Exercise Program Applied in the LAST Study and Functional Recovery After Stroke. Arch. Phys. Med. Rehabil. 2019, 100, 2251–2259. [Google Scholar] [CrossRef]
- Dean, E. Physical therapy in the 21st century (Part I): Toward practice informed by epidemiology and the crisis of lifestyle conditions. Physiother. Theory Pract. 2009, 25, 330–353. [Google Scholar] [CrossRef]
- Dean, E.; Skinner, M.; Myezwa, H.; Mkumbuzi, V.; Mostert, K.; Parra, D.C.; Shirley, D.; Söderlund, A.; de Andrade, A.D.; Abaraogu, U.O.; et al. Health Competency Standards in Physical Therapist Practice. Phys. Ther. 2019, 99, 1242–1254. [Google Scholar] [CrossRef]
- Dean, E.; Creig, A.; Murphy, S.; Roots, R.; Nembhard, N.; Rankin, A.; Bainbridge, L.; Anthony, J.; Hoens, A.M.; Garland, S.J. Raising the Priority of Lifestyle-Related Noncommunicable Diseases in Physical Therapy Curricula. Phys. Ther. 2016, 96, 940–948. [Google Scholar] [CrossRef]
- Anand, S.; Bradshaw, C.; Prabhakaran, D. Prevention and management of CVD in LMICs: Why do ethnicity, culture, and context matter? BMC Med. 2020, 18, 7. [Google Scholar] [CrossRef]
- Minja, N.W.; Nakagaayi, D.; Aliku, T.; Zhang, W.; Ssinabulya, I.; Nabaale, J.; Amutuhaire, W.; De Loizaga, S.R.; Ndagire, E.; Rwebembera, J.; et al. Cardiovascular diseases in Africa in the twenty-first century: Gaps and priorities going forward. Front. Cardiovasc. Med. 2022, 9, 1008335. [Google Scholar] [CrossRef] [PubMed]
- Dzudie, A.; Rayner, B.; Ojji, D.; Schutte, A.E.; Twagirumukiza, M.; Damasceno, A.; Ba, S.A.; Kane, A.; Kramoh, E.; Kacou, J.B.A.; et al. Roadmap to achieve 25% hypertension control in Africa by 2025. CVJA 2017, 28, 261–272. [Google Scholar] [CrossRef]
- Ngeh, E.N. Research among undergraduate biomedical students in Cameroon: Contextual barriers, room for improvement. Pan Afr. Med. J. 2019, 33, 149. [Google Scholar] [CrossRef] [PubMed]
- Ngeh Ngeh, E.; Chigbo, N.N.; Whitehouse, Z.; Anekwu, E.M.; Mukaruzima, L.M.; Mtsetfwa, L.; Kitur, R.; Agoriwo, M.W.; Ondogah, P.; Douryang, M.; et al. A report on the development of COVID-19 guidelines for rehabilitation professionals in African settings. Pan Afr. Med. J. 2021, 38, 129. [Google Scholar] [CrossRef] [PubMed]
- Bennell, K.L.; Lawford, B.J.; Keating, C.; Brown, C.; Kasza, J.; Mackenzie, D.; Metcalf, B.; Kimp, A.J.; Egerton, T.; Spiers, L.; et al. Comparing Video-Based, Telehealth-Delivered Exercise and Weight Loss Programs with Online Education on Outcomes of Knee Osteoarthritis: A Randomized Trial. Ann. Intern. Med. 2022, 175, 198–209. [Google Scholar] [CrossRef] [PubMed]

