1. Introduction
Inflammatory bowel disease (IBD) is a chronic health condition marked by recurrent episodes of inflammation of the gastrointestinal tract. It includes two subtypes, better known as Crohn’s disease (CD) and ulcerative colitis (UC), distinguished mainly on the basis of the site of inflammation, which in UC is confined to the colon, but in CD may affect the entire gastrointestinal (GI) tract. Both conditions are highly unpredictable in nature, with stress (psychotrauma in particular) playing an important exacerbating role, accounting for a significant proportion of patients’ interindividual symptom variability. Specifically, stressful or traumatic experiences are known to activate the brain–gut axis, a complex communication system involving bidirectional interactions between the central nervous system, the autonomic nervous system, the hypothalamic–pituitary–adrenal (HPA) axis, and the digestive tract [1,2,3,4,5], allowing the brain to exert its regulatory influence over the gut, with the additional effect that a person’s GI health cannot be considered in isolation from his/her psychological and intersubjective functioning. Still, gastroenterologists and other health care providers pay surprisingly little attention to the influence of (inter)personal life experiences and/or emotional stress sensitivity on the functioning of IBD patients [6,7].
A first observation indicative of a meaningful relation between traumatizing stress and GI pathology is the high prevalence of psychotrauma and post-traumatic stress disorders (PTSDs) in GI (including IBD) patients. In the 1990s, it was already established that over 40% of GI patients attending a gastroenterological clinic had a history of physical or sexual abuse [8,9,10]. Moreover, those exposed to abuse exhibited significantly more inflammatory and functional bowel symptoms, somatic complaints, physical disability, lifetime surgeries, and a lower quality of life (QoL) than non-abused GI patients [9,11,12,13,14,15]. Likewise, several other traumatic experiences are now increasingly associated with IBD [12,16,17], calling for a further exploration of the relationship between stressful life experiences and GI vulnerability.
A second line of evidence supporting the stress/trauma-GI connection stems from research on the somatic (i.e., GI) correlates of psychotrauma, indicating that adverse life experiences often have profound and long-lasting disruptive effects on GI function. To illustrate, victims of physical or sexual abuse appeared to be more susceptible to a host of GI complaints [18], ranging from chronic abdominal pain, diarrhea, constipation to nausea, vomiting, bloating, and heartburn [19,20,21,22,23]. Likewise, a majority (71%) of battered women exposed to sexual, physical, or psychological partner violence were found to suffer from persistent indigestion, diarrhea, constipation, spastic colon, or pelvic pain [24,25,26,27]. Beyond intimate and domestic violence, GI symptoms and/or illnesses are also highly prevalent in people who experienced war or war-related captivity [28,29,30,31,32], making it all the more likely that negative, traumatic life experiences significantly amplify and/or increase the risk of (exacerbating) GI pathologies.
The apparent relationship between traumatic or stressful experiences and GI pathology might, however, not be a direct one. Whether a person becomes symptomatic in the aftermath of a traumatic experience seems best predicted by the degree of self-efficacy experienced at the time of the event, i.e., the degree to which the individual felt able to manage or control the situation at hand [33,34,35,36]. The greatest GI (inflammatory/functional) symptom aggravation is thus to be expected in the aftermath of traumatic or stressful events relative to which feelings of being ineffective, incompetent, helpless, and unable to function as an effective agent dominated. Indeed, experiences of a lack of mastery and control are often accompanied by detrimental (functional and structural) changes in the GI tract. To illustrate, uncontrollability during stress (e.g., during “helplessness” test paradigms) was found to predispose animals to gastric ulceration [37], intestinal inflammation, intestinal epithelial permeability [38,39,40,41], altered composition of the microbiota [42], hyper-reactivity of the GI tract [43], and (chemically induced) colitis [44]. Similarly, in patients suffering from IBD, episodes of bleeding and relapse were shown to occur almost exclusively following a subjective experience of being “absolutely crushed”, “helpless”, “hopeless”, “powerless”, “shocked”, and “endangered or enraged but powerless to do anything” [45]. Thus, to summarize, uncontrollable stressful experiences may severely increase IBD patients’ inflammatory and functional symptom profiles and decrease their quality of life, most likely as a function of diminished efficacy experiences.
A commonly acknowledged cognitive–emotional predisposition for frequently experiencing stress and uncontrollability due to a poor sense of personal effectiveness is neuroticism. Individuals with high trait neuroticism suffer from a weak sense of agency, heightened sense of incapacity, and a chronically felt inability to manage challenging events and withstand environmental demands, rendering them particularly vulnerable to feelings of helplessness, negatively tinted experiences, and related affective and somatic pathologies [46]. By confirmation, neuroticism is considered a major predictor for the development of PTSD in response to adversity [47] and associated with a wide range of mental and physical disorders. While IBD—too—appears to be more prevalent in individuals with a neurotic disposition [48], the exact influence of neuroticism on patients’ morbidity and trauma-related symptom aggravations remains to be established.
In conclusion, the high prevalence of trauma and emotional stress vulnerability (neuroticism) among IBD patients, the aggravating effect of adverse life events on the clinical expression of GI disease, and the heightened gut sensitivity in victims loaded with interpersonal trauma all point to trauma and felt uncontrollability as important vulnerability factors driving GI (inflammatory and functional) symptomatology. The current study further explored the notion of such experience-driven GI susceptibility in a sample of IBD patients. To this end, we first established the trauma and emotional stress sensitivity (neuroticism) profiles of IBD patients and related them to (interindividual differences in) inflammatory/functional symptom expressions and quality of life (QoL). Here, symptom/QoL scores were expected to fluctuate as a function of past trauma and neuroticism, with neuroticism either mediating or moderating the negative effects of trauma on GI health. I.e., while it is conceivable that trait neuroticism (reflecting feelings of incapacity and uncontrollability) moderates (influences/intensifies) the effect of trauma on (GI) health, it is equally plausible that it decisively determines (mediates) it (i.e., a strong/meaningful effect of psychological trauma on GI disease is only expected in those who experience such trauma as highly severe and uncontrollable). Secondly, the relative influence of trauma type on these relationships was explored, whereby inflammatory and functional bowel symptoms were hypothesized to increase in accord with trauma complexity (degree of threat to the self or other).
2. Materials and Methods
2.1. Study Sample
A total of n = 112 patients diagnosed with Crohn’s disease (CD, 75.9% female, 24.1% male) and n = 99 patients diagnosed with ulcerative colitis (UC; 78.8% female, 21.2% male) were recruited via a gastroenterological university clinic (MUMC+), advertisements on social media, local newspapers, and online platforms of patient organizations. Only patients whose self-reports indicated that they had received an official IBD diagnosis were included in the study. For further exploratory analyses, an additional 51 controls without significant GI complaints (66.7% female, 33.3% male) were enrolled using aforementioned recruitment channels complemented with the Maastricht University’s Research Participation System. The study was approved by the Ethics Review Committee Psychology and Neuroscience at Maastricht University (ERCPN-205_14_03_2019) and complied with the Helsinki Declaration. Informed consent was obtained from all participants.
2.2. Materials
2.3. Procedure
Patients were approached via the gastroenterological university clinic Maastricht (MUMC+), social media, local newspapers, and online platforms of patient organizations. They were invited to sign up via email, after which they were informed about the study and received a link to the online questionnaire package (Qualtrics®). After signing the informed consent, the previously described questionnaires were administered in the following order: the IBS-SSS, IBDQ, P-HBI, P-SCCAI, the Dutch Life Events Questionnaire, and the neuroticism scale. Median completion time was 21.5 min.
2.4. Data Analysis
All data were first examined for missing values (SPSS version 26 for Mac, IBM Corp., Armonk, NY, USA). For one patient, the IBS-SSS score was missing and for seven patients, the P-HBI scores were lacking. These patients were excluded from the respective analyses. First, t-tests were conducted to verify whether Crohn’s and colitis patients (CD | UC) significantly differ in symptom reporting (P-SCCAI, P-HBI, IBS-SSS, IBDQ scores). Since this was not the case, (ts < 1.59, ps > 0.11), patient groups were merged for further analyses. Next, bivariate correlations showed that age was not meaningfully related to physical/mental symptom severity (IBDQ, P-HBI, and P-SCCAI scores respectively) (rs < 0.10, ps > 0.18), allowing it to be omitted as a factor from further analyses. Additional bivariate correlations established a large co-variability between the two IBD activity index scores (P-SCCAI and P-HBI) (r(202)= 0.79, p < 0.001) allowing them to be pooled into a single composite Crohn’s–colitis activity score (P-SCCAI + P-HBI). One-way ANOVAs were performed to compare cumulative trauma, trauma subtype, and neuroticism scores across different disease activity groups (quiescent, mild, moderate, and severe IBD activity). Hierarchical multiple regression analyses were conducted to examine whether neuroticism altered the expected association between trauma exposure (either total trauma or a trauma profile as predictor) and IBD disease activity (i.e., pooled Crohn’s–colitis activity, functional GI symptoms, and disease-related QoL). Here, trauma exposure (Model 1), neuroticism (Model 2) were mean-centered and sequentially added as predictors of changes in disease activity. Significant regressions were further analyzed using Preacher and Hayes PROCESS moderation and mediation analyses (Model 1 and 4, bootstrapping with 5000 resamples). All statistics were evaluated at a (two-tailed) significance level of 5%.
3. Results
3.1. Sample Characteristics
At study entry, 42.1% of Crohn’s (CD) patients presented with active disease (as indicated by a P-HBI score > 5), and approximately three-quarters (74.1%) reported significant functional GI complaints (IBS-SSS score > 74). As for Colitis (UC) patients, roughly two-thirds (66.7%) suffered active disease (P-SCCAI score > 2), and almost three-quarters (72.4%) experienced functional GI symptoms.
3.2. Disease Activity Group Differences in Cumulative Traumatization and Neuroticism
One-way ANOVAs revealed a main effect of disease activity (quiescent, mild, moderate, severe) for total trauma exposure (F(3, 203) = 3.83, p = 0.01), past victimization (F(3, 203) = 3.45, p < 0.05), and neuroticism (F(3, 203) = 14.58, p < 0.001) (see . Pairwise comparisons using Tukey’s post hoc tests revealed that patients with severe IBD activity experienced significantly more cumulative trauma (p < 0.05), interpersonal victimization (p < 0.01), and structural feelings of uncontrollability and powerlessness (neuroticism) (p < 0.001) than those with quiescent IBD. Moreover, patients with mild (p < 0.01) and moderate (p < 0.001) disease activity scored significantly higher on the neuroticism scale than those with quiescent disease, while those with mild IBD scored significantly lower than those with severe IBD (p < 0.05). The remaining comparisons proved non-significant (ps > 0.20).
3.3. Correlations between Experiential Vulnerability Factors and Disease Activity
Significant correlations between predictors (total trauma, trauma profiles, and neuroticism scores) and dependent outcome variables (IBS-SSS, Composite CD-UC activity and IBDQ scores) are summarized in . Both neuroticism and victimization were most closely associated with all outcome measures. Total trauma (TT) and psychopathology of self (PoS) correlated with two of the three disease activity measures (IBD activity score and disease-related QoL, respectively).
3.4. Effect of Neuroticism on the Relationship between Trauma and IBD Activity
Hierarchical regression analyses revealed that total trauma (TT) as sole predictor (Model 1) explained a small but significant proportion (3%) of the variance in IBD activity scores (F(1, 202) = 6.252, p = 0.013, R2 = 0.03; . When adding neuroticism as an additional predictor (Model 2) the model more powerfully explained 21% of the variance in IBD activity scores (F(2, 201) = 26.512; p < 0.001), with TT no longer forming a significant predictor of IBD scores. Additional exploratory analyses with a small group of available controls (n = 51) indicated that addition of condition (dummy variable: IBD = 1, controls = 0) as a third predictor (β = 0.30; p < 0.001) yielded a significant increase in explanatory capacity, with trauma (β = 0.05; p = 0.35) and neuroticism (β = 0.39; p < 0.001) now explaining 31% of the variance in IBD activity, F(3, 248) = 36.98, p < 0.001, R2 = 0.31.
To further examine and interpret significant regressions, moderation and mediation analyses were performed using the PROCESS macro (Model 1 and 4; bootstrapping with 5000 resamples). Results showed that neuroticism did not moderate (b = 0.022, p = 0.14) but, rather, mediated the effect of TT on IBD activity (bootstrapped estimate = 0.27, 95% CI = 0.126, 0.454), with the indirect (neuroticism-mediated) path accounting for 70% of the total effect. Hence, greater trauma accumulation was meaningfully related to a structural experience of incapacity or low controllability and, accordingly, to a greater clinical disease expression. Upon correction for neuroticism, the direct effect of TT on patients’ clinical disease expression ceased to be significant (b = 0.011, p = 0.43), reaffirming the indirect influence of TT on patients’ clinical disease profiles.
To establish which trauma profile was most specific to the association between TT and IBD activity, the two-step regression model was repeated for each trauma profile separately. Out of all traumata, only victimization (Vic) (Model 1: β = 0.149; p < 0.05) and psychopathology of the self (PoS) (Model 1: β = 0.160; p < 0.05) were significantly related to IBD activity. Yet, while PROCESS mediation analyses showed that the effect of PoS on clinical disease expression was significantly mediated by neuroticism, (bootstrapped estimate = 2.01, 95% CI = 1.216, 3.003; Figure 1B), the effect of Vic was not (bootstrapped estimate = 0.46, 95% CI = −0.006, 0.987; Figure 1A), even though 43% of Vic’s total effect was accounted for by the indirect (neuroticism-mediated) path.
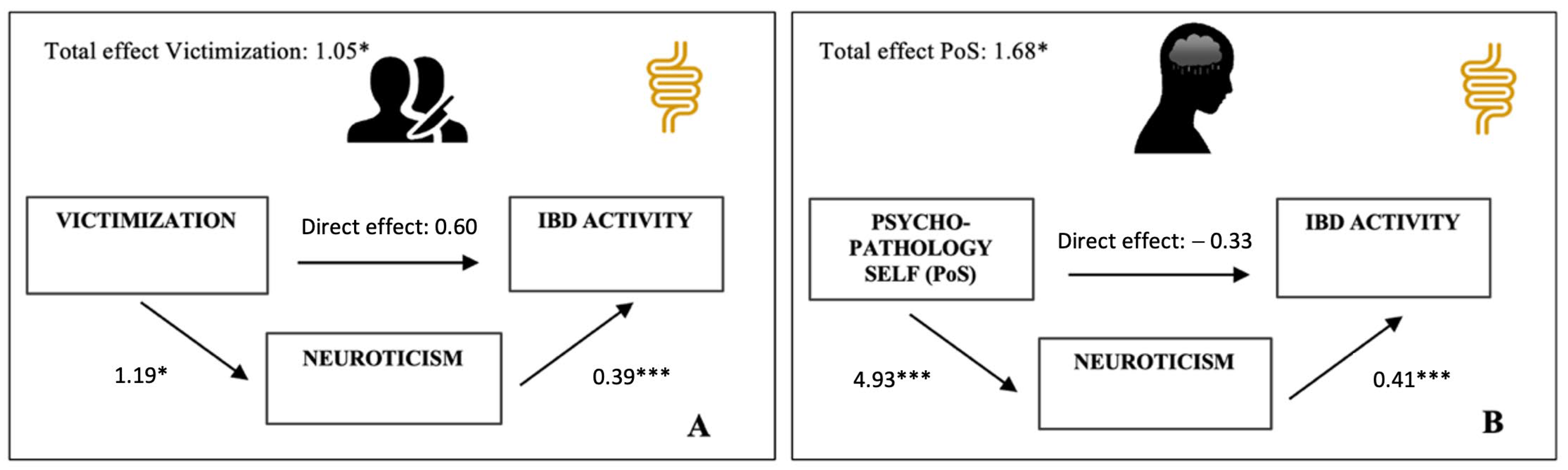
Figure 1. Multiple mediation models of the relationship between traumatic life events and IBD activity. (A) Model with victimization predicting IBD activity scores. (B) Model with psychopathology of self predicting IBD activity scores. All path estimates are unstandardized regression coefficients. Both trauma profiles are measured on a similar scale, making comparison of the effect estimates straightforward. * p < 0.05; *** p < 0.001.
3.5. Effect of Neuroticism on the Relationship between Trauma and Functional GI Symptom Scores
Hierarchical regression analyses indicated that total trauma (TT) as sole predictor (Model 1) could not significantly predict the variance in functional GI symptom scores (FGISS) (F(1, 208) = 2.633; p = 0.106; R2 = 0.013; . Yet, when letting the regression model take into account a possible additional influence of neuroticism (Model 2), it now more powerfully explained 16% of the variance in FGISS (Model 2: F(2, 207) = 19.243; p < 0.001, R2 = 0.157). Subsequent exploratory analyses with a small group of available controls (n = 51) indicated that inclusion of condition as third predictor (β = 0.39; p < 0.001) resulted in a further increase in explanatory capacity, with trauma (β = 0.01; p = 0.93) and neuroticism (β = 0.34; p < 0.001) now explaining 32% of the FGISS variance, F(3, 255) = 40.55, p < 0.001, R2 = 0.32.
Considering the influence of the individual trauma profiles, victimization (Vic) emerged as the only meaningful predictor of FGISS scores explaining a modest yet significant proportion of interindividual variability in FGISS (Model 1: F(1, 208) = 5.851; p = 0.016). Hence, where TT had no significant effect on FGISS , step 1), Vic did. Subsequent process moderation and mediation analyses confirmed that neuroticism did not moderate, (b = 0.732, p = 0.30) but significantly mediated, the association between Vic and FGISS variability (bootstrapped estimate = 6.51; 95% CI: 0.741, 13.553; Figure 2). Upon correction for neuroticism, the direct effect of Vic on patients’ functional bowel symptoms ceased to be significant (b = 11.54, p = 0.10), reaffirming the mere indirect influence of Vic on patients’ functional GI complaints.
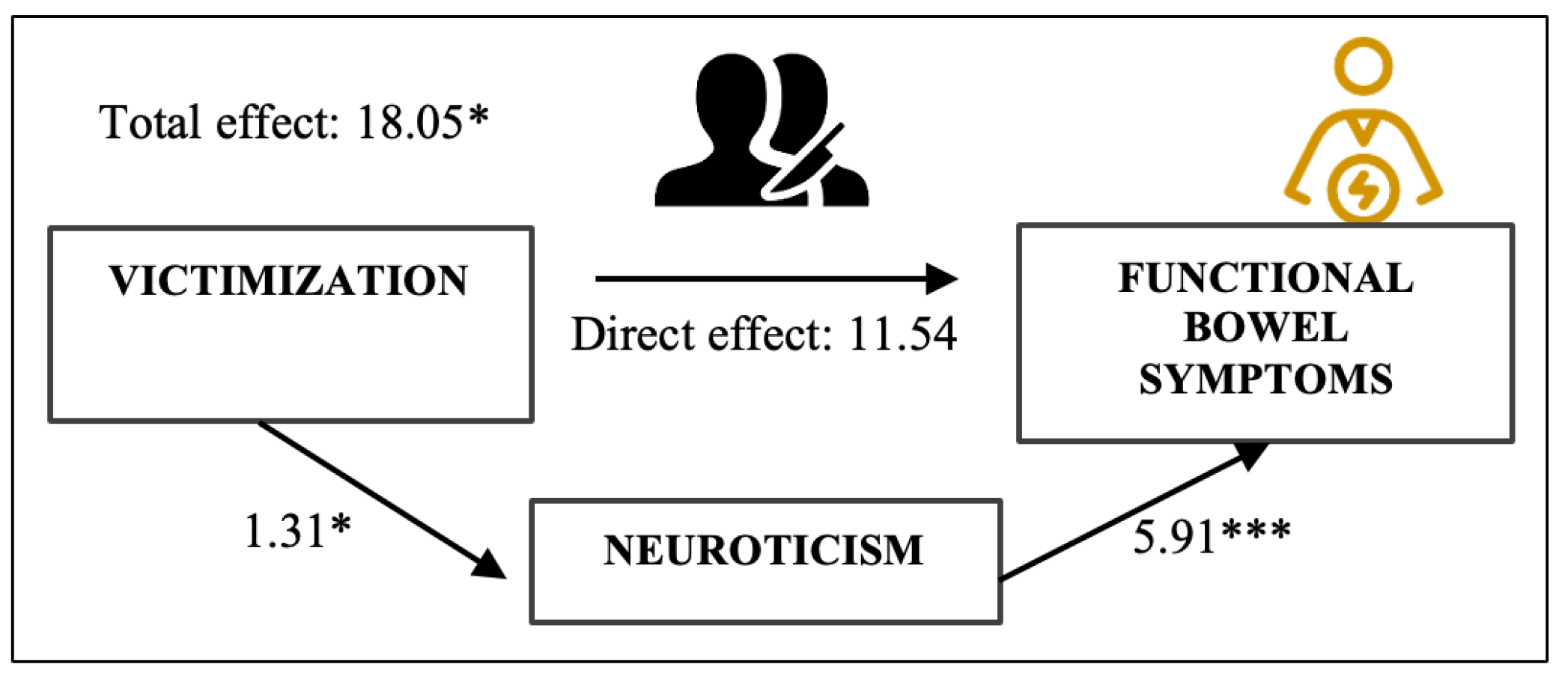
Figure 2. Mediation model of the relationship between victimization and functional bowel symptom severity. All path estimates are unstandardized regression coefficients. * p < 0.05. *** p < 0.001.
3.6. Effect of Neuroticism on the Relationship between Trauma and Disease-Related QoL Scores
A hierarchical regression analysis including trauma accumulation as sole predictor of interindividual differences in QoL (Model 1) revealed that total trauma (TT) explained a small yet significant proportion (3%) of the variance in QoL (F(1, 209) = 6.948, p = 0.009; . When adding neuroticism as second predictor (Model 2), the model now more powerfully explained 35% of the variance in QoL scores (F(2, 208) = 56.481; p < 0.001, R2 = 0.352). Subsequent exploratory analyses with a small control group revealed that addition of condition (β = −0.33; p < 0.001) as a third predictor resulted in another 12% gain in explanatory power, with TT (β = −0.02; p = 0.62) and neuroticism (β = −0.53; p < 0.001) now accounting for 47% of variance in QoL. PROCESS moderation and mediation modelling showed that neuroticism did not moderate, (b = 0.003, p = 0.96) but mediated the relationship between TT and EIC (bootstrapped estimate = −1.632, 95% CI = −2.506, −0.885). That is, trauma accumulation positively predicted neuroticism (b = 0.74, p < 0.001), which, in turn, negatively affected patients’ overall QoL (b = −2.20, p < 0.001). After adjustment for neuroticism, TT was no longer meaningfully associated with QoL (b = −0.088, p = 0.88), confirming the mere indirect association between TT and QoL.
Additional regression analyses for the trauma profiles separately identified victimization (β = −0.219; p = 0.001) as the trauma profile with the most detrimental effect on patients’ QoL (Model 1: F(1, 209) = 10.571; p = 0.001, R2 = 0.048), followed by psychopathology of the self (PoS) (Model 1: F(1, 209) = 7.445; p = 0.007, R2 = 0.034). Next, PROCESS mediation analyses revealed that the negative effects of both trauma profiles were mediated by neuroticism (Vic: bootstrapped estimate = −2.747, 95% CI = −5.524, −0.375; Figure 3A; PoS: bootstrapped estimate = −12.198, 95% CI = −17.216, −8.170; Figure 3B). However, while TT and PoS merely exerted an indirect (neuroticism-mediated) effect on QoL, Vic influenced QoL both directly (b = −4.06, p < 0.05) and indirectly (via neuroticism), hinting at the mere partial mediating role of neuroticism in the association between victimization and overall function.
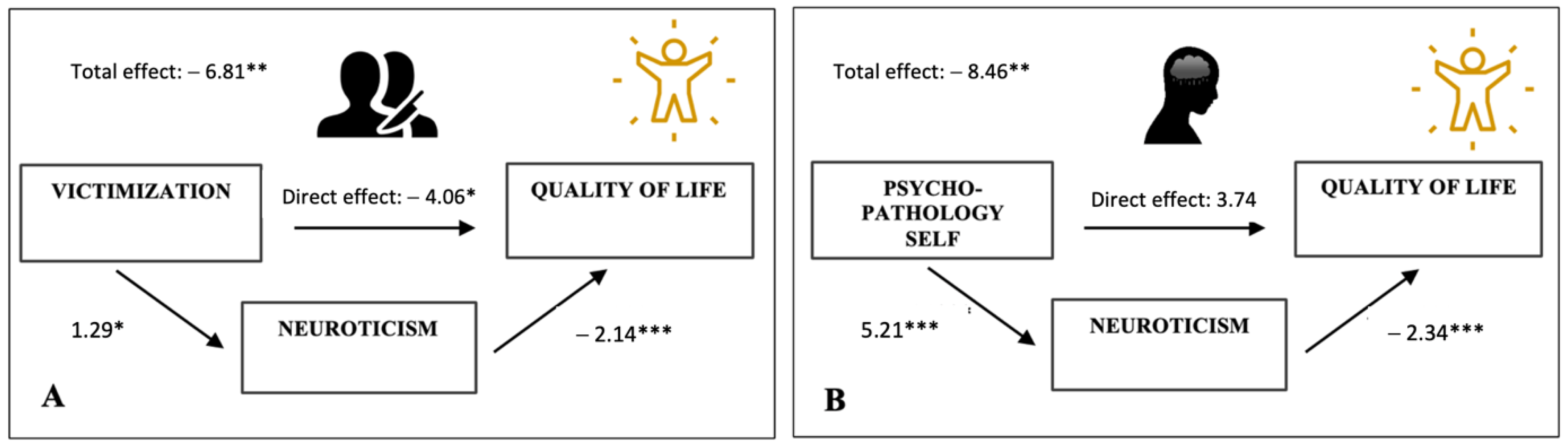
Figure 3. Multiple mediation models of the relationship between different trauma experiences and patients’ overall quality of life (QoL). (A) Model with the trauma factor victimization predicting QoL scores. (B) Model with trauma factor psychopathology of self predicting QoL scores. * p < 0.05; ** p < 0.01; *** p < 0.001.
4. Discussion
In the current study, the association between negative life events, emotional stress vulnerability, and symptom variability in patients with inflammatory bowel disease (IBD) was examined. Consistent with a biopsychosocial understanding of IBD [5], the findings provided partial support for the hypotheses that patients’ (inflammatory and functional) symptom presentations fluctuate in accord with their cumulative trauma experiences and emotional stress sensitivity.
First, we found that patients with severe IBD activity have endured significantly more interpersonal trauma and victimization than those with quiescent IBD. Moreover, we established that patients’ cumulative trauma scores were meaningfully associated with (i.e., predictive of) their IBD activity and quality of life scores. That is, the greater the patient’s exposure to interpersonal trauma, the greater their inflammatory symptom expression and the lower their overall quality of life. As anticipated, the effect of trauma on disease activity was mediated by neuroticism, with both factors conjointly accounting for 21% of the variance in inflammatory (GI) symptoms, 16% of the variance in functional GI symptoms, and 35% of the variance in quality of life. More so, upon correction for neuroticism, cumulative trauma lost its explanatory capacity, indicating that structural experiences of uncontrollability and incapacity were at the root of the trauma-induced disease exacerbations. This substantiates existing research suggesting that the symptomatic consequences of trauma are best predicted by the magnitude of felt helplessness, incapacity, or lack of agency. Moreover, it supports data linking structural experiences of uncontrollability and incapacity (neuroticism) to somatic and affective symptomatology [59,60,61] and subjective dysfunction in IBD patients [62]. Exploratory regressions with a small group of available controls (n = 51) suggest that the effect of trauma and neuroticism is more pronounced in IBD patients. That is, when adjusting for condition (IBD diagnosis), the explanatory power of trauma and neuroticism in relation to psychological and somatic dysfunction doubled, with the two factors now accounting for 31% of the variance in inflammatory (GI) symptoms, 32% of the variance in functional GI symptoms, and up to 47% of the cross-sample mental (QoL) symptom variance.
Out of all traumata analyzed, victimization (esp. domestic violence and intimate abuse) emerged as the best predictor of the interindividual symptom variability and the only trauma profile with a consistent influence on both mental (QoL) and physical fitness of IBD patients—be it with respect to functional bowel symptoms only by mediation of neuroticism. This is consistent with existing literature [63]. First, it confirms that complex trauma (i.e., pervasive domination of the other over the self) is most disruptive to a person’s self-regulatory capacity. Second, it affirms that individuals with a stronger sense of uncontrollability are more susceptible to the functional GI consequences of victimization. Third, it illustrates that repetitive trauma (as in domestic violence) tends to amplify and generalize the physiologic and affective symptoms of post-traumatic stress [63], with symptoms increasing progressively in relation to stressor intrusiveness. Finally, it illustrates that the traumas that pose the greatest risk in terms of attachment insecurity [64], have the strongest GI symptom-promoting effect—which is coherent with literature linking insecure attachment to heightened affective, neuroendocrine, and inflammatory reactivity [65,66,67,68,69] and studies reporting on the high prevalence of insecure attachment amongst IBD patients [70,71,72].
Interestingly, neuroticism only partially mediated the association between victimization and self-reported wellbeing. This may well be attributed to the fact that the detrimental effect of victimization is supposedly less dependent on—and yet itself dramatically disruptive to—patients’ structurally felt effectiveness and adaptive abilities. As for the remaining trauma profiles, only psychopathology of the self (PoS; patients’ current and past mental comorbidity) coincided with greater physical (inflammation-related) and mental (QoL) function impairment. Yet, upon further analysis, the symptom-aggravating effect of PoS proved merely of an indirect nature, i.e., informed by its inter-relatedness with neuroticism.
To summarize, other than victimization, trauma histories merely exhibited an indirect, neuroticism-mediated effect on patients’ symptom profiles. Hence, neuroticism (reflecting feelings of incompetence and uncontrollability) decisively determined—rather than merely influenced/reinforced—the effect of trauma experiences on (GI) health, implying that a significant effect of psychological trauma on GI illness is mainly to be expected among those who experience such trauma as very severe and uncontrollable. This stands in contrast to previous studies linking cumulative trauma to IBD [12]. Yet, it affirms that—as far as experience-driven (IBD) symptom complexity is concerned—the emphasis is not on trauma accumulation in general, but rather on the experiential state of helplessness, incapacity, and paralysis potentially evoked by it, the manifestation thereof and resistance to which varies as a function of emotional stress vulnerability (neuroticism) and trauma complexity. That is, while feelings of uncontrollability are at the core of neuroticism, they are also widespread in victims of complex trauma (victimization), permanently lowering their thresholds for stress [63].
Current findings must be evaluated considering several limitations. First, trauma histories were evaluated retrospectively and are therefore subject to recall bias. Moreover, trauma scopes were narrowed to a limited number of mainly interpersonal stress experiences with a well-established disruptive effect on the stress-adaptation systems involved in IBD. As such, the study does not contribute to a better understanding of the sensitizing effects of nonsocial experiences, nor of the synergetic effect of social and nonsocial stressors. Third, given the non-specificity of the GI symptomatic repertoire and absence of a sufficiently sensitive (bio)marker of inflammatory activity, the reading of IBD patients’ (inflammatory and functional) symptom profiles was hampered. To resolve these issues in future studies, subjective disease activity indices may be complemented with biochemical markers such as fecal calprotectin that allow for a better differentiation between ongoing IBD activity and concomitant IBS. Fourth, as COVID-19-related measures abruptly restricted patient recruitment in university clinics, we were forced to continue the recruitment procedure online and rely on self-reported IBD diagnoses only, devoid of information on diagnostic procedures followed and parameters used. However, previous research has shown that IBD patients are perfectly capable of providing accurate information (through online self-reports) on their medical history and type of disease [73]. Additionally, considering existing literature identifying inflammation as a risk factor for PTSD, it seems plausible that the causal pathways postulated here are, in fact, bidirectional in nature [74]. To further explore this possibility, inverse mediation models were run (with IBD measures as predictors, neuroticism as mediator, and total trauma as dependent variable), revealing that IBD activity, by augmenting individuals’ stress sensitivity, renders them more vulnerable to structural trauma experiences. Altogether, the findings thus point to a reciprocal relationship between trauma and IBD, with both factors prospectively increasing individuals’ stress sensitivity and therewith their vulnerability to chronic stress experiences and disease progression. Yet, given the cross-sectional nature of the present study, longitudinal studies are needed to better identify the temporal relationships between trauma and IBD activity. Lastly, the results may have been colored by the presence of psychiatric disorders (observed in six patients, one control) as well as the use of psychotropic agents (seven patients, two controls). However, when rerunning all analyses without the affected participants, the same mediating effects of neuroticism emerged while the moderation effects remained insignificant).
5. Conclusions
Despite the aforementioned limitations, the current study shows that neuroticism and victimization play a significant role in predicting IBD patients’ (mental/somatic) functioning, most likely by giving rise to an affective stance rotating around feelings of uncontrollability and a confusion about the self as agent. By implication, there where feelings of being ineffective, incompetent, not in control, and unable to function as a relatively autonomous agent prevail, a more aggressive (inflammatory/functional) disease course is to be expected. As such, the present study adds to the growing body of evidence linking experiential vulnerability to IBD expression. It naturally follows that interventions aimed at restoring a sense of agency, rebalancing an overly externally oriented locus of control, and inviting patients into (new) habit formation wherein feelings of mastery, efficacy, choice, and capacity for deliberate action have a natural place are most promising in dampening experientially driven symptom exacerbations in IBD patients.
References
- D’Andrea, W.; Sharma, R.; Zelechoski, A.; Spinazzola, J. Physical Health Problems after Single Trauma Exposure. J. Am. Psychiatr. Nurses Assoc. 2011, 17, 378–392. [Google Scholar] [CrossRef] [PubMed]
- McCrory, C.; Dooley, C.; Layte, R.; Kenny, R. The Lasting Legacy of Childhood Adversity for Disease Risk in Later Life. Health Psychol. 2015, 34, 687–696. [Google Scholar] [CrossRef] [PubMed]
- Campbell, R.; Sefl, T.; Ahrens, C.E. The Physical Health Consequences of Rape: Assessing Survivors’ Somatic Symptoms in a Racially Diverse Population. Women’s Stud. Q. 2003, 31, 90–104. [Google Scholar]
- De Sousa, J.F.M.; Paghdar, S.; Khan, T.M.; Patel, N.P.; Chandrasekaran, S.; Tsouklidis, N. Stress and Inflammatory Bowel Disease: Clear Mind, Happy Colon. Cureus 2022, 14, e25006. [Google Scholar] [CrossRef] [PubMed]
- Ballou, S.; Feingold, J.H. Stress, Resilience, and the Brain-Gut Axis: Why Is Psychogastroenterology Important for all Digestive Disorders? Gastroenterol. Clin. N. Am. 2022, 51, 697–709. [Google Scholar] [CrossRef] [PubMed]
- Craven, M.R.; Quinton, S.; Taft, T.H. Inflammatory Bowel Disease Patient Experiences with Psychotherapy in the Community. J. Clin. Psychol. Med. Settings 2019, 26, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Keefer, L.; Sayuk, G.; Bratten, J.; Rahimi, R.; Jones, M.P. Multicenter study of gastroenterologists’ ability to identify anxiety and depression in a new patient encounter and its impact on diagnosis. J. Clin. Gastroenterol. 2008, 42, 667–671. [Google Scholar] [CrossRef]
- Drossman, D. Sexual and Physical Abuse in Women with Functional or Organic Gastrointestinal Disorders. Ann. Intern. Med. 1990, 113, 828. [Google Scholar] [CrossRef]
- Leserman, J.; Drossman, D.; Li, Z.; Toomey, T.; Nachman, G.; Glogau, L. Sexual and Physical Abuse History in Gastroenterology Practice. Psychosom. Med. 1996, 58, 4–15. [Google Scholar] [CrossRef]
- Walker, E.A.; Katon, W.J.; Roy-Byrne, P.P.; Jemelka, R.P.; Russo, J. Histories of Sexual Victimization in Patients with Irritable Bowel Syndrome or Inflammatory Bowel Disease. Am. J. Psychiatry 1993, 150, 1502–1506. [Google Scholar] [CrossRef]
- Baccini, F.; Pallotta, N.; Calabrese, E.; Pezzotti, P.; Corazziari, E. Prevalence of Sexual and Physical Abuse and Its Relationship with Symptom Manifestations in Patients with Chronic Organic and Functional Gastrointestinal Disorders. Dig. Liver Dis. 2003, 35, 256–261. [Google Scholar] [CrossRef]
- Bednarikova, H.; Kascakova, N.; Furstova, J.; Zelinkova, Z.; Falt, P.; Hasto, J.; Tavel, P. Life Stressors in Patients with Inflammatory Bowel Disease: Comparison with a Population-Based Healthy Control Group in the Czech Republic. Int. J. Environ. Res. Public Health 2021, 18, 3237. [Google Scholar] [CrossRef] [PubMed]
- Drossman, D.; Li, Z.; Leserman, J.; Toomey, T.; Hu, Y. Health Status by Gastrointestinal Diagnosis and Abuse History. Gastroenterology 1996, 110, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Caplan, R.A.; Maunder, R.G.; Stempak, J.M.; Silverberg, M.S.; Hart, T.L. Attachment, childhood abuse, and IBD-related quality of life and disease activity outcomes. Inflamm. Bowel Dis. 2014, 20, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Kanuri, N.; Cassell, B.; Bruce, S.E.; White, K.S.; Gott, B.M.; Gyawali, C.P.; Sayuk, G.S. The impact of abuse and mood on bowel symptoms and health-related quality of life in irritable bowel syndrome (IBS). Neurogastroenterol. Motil. 2016, 28, 1508–1517. [Google Scholar] [CrossRef] [PubMed]
- Thomann, A.; Lis, S.; Reindl, W. P796 Adverse Childhood Events and Psychiatric Comorbidity in a Single-Centre IBD-Cohort. J. Crohn’s Colitis 2018, 12, S514. [Google Scholar] [CrossRef]
- Glynn, H.; Möller, S.; Wilding, H.; Apputhurai, P.; Moore, G.; Knowles, S. Prevalence and Impact of Post-Traumatic Stress Disorder in Gastrointestinal Conditions: A Systematic Review. Dig. Dis. Sci. 2021, 66, 4109–4119. [Google Scholar] [CrossRef] [PubMed]
- Leserman, J.; Drossman, D. Relationship of Abuse History to Functional Gastrointestinal Disorders and Symptoms: Some possible mediating mechanisms. Trauma Violence Abus. 2007, 8, 331–343. [Google Scholar] [CrossRef] [PubMed]
- Felitti, V. Long-Term Medical Consequences of Incest, Rape, and Molestation. South. Med. J. 1991, 84, 328–331. [Google Scholar] [CrossRef]
- Golding, J. Sexual Assault History and Physical Health in Randomly Selected Los Angeles Women. Health Psychol. 1994, 13, 130–138. [Google Scholar] [CrossRef]
- Hulme, P. Symptomatology and Health Care Utilization of Women Primary Care Patients Who Experienced Childhood Sexual Abuse. Child Abus. Negl. 2000, 24, 1471–1484. [Google Scholar] [CrossRef] [PubMed]
- Lechner, M.E.; Vogel, M.E.; Garcia-Shelton, L.M.; Leichter, J.L.; Steibel, K.R. Self-reported medical problems of adult female survivors of childhood sexual abuse. J. Fam. Pract. 1993, 36, 633–638. [Google Scholar] [PubMed]
- Melchior, C.; Wilpart, K.; Midenfjord, I.; Trindade, I.A.; Törnblom, H.; Tack, J.F.; Simrén, M.; Van Oudenhove, L. Relationship between Abuse History and Gastrointestinal and Extraintestinal Symptom Severity in Irritable Bowel Syndrome. Psychosom. Med. 2022, 84, 1021–1033. [Google Scholar] [PubMed]
- Talley, N.; Fett, S.; Zinsmeister, A.; Melton, L. Gastrointestinal Tract Symptoms and Self-Reported Abuse: A Population-Based Study. Gastroenterology 1994, 107, 1040–1049. [Google Scholar] [CrossRef] [PubMed]
- Perona, M.; Benasayag, R.; Perelló, A.; Santos, J.; Zárate, N.; Zárate, P.; Mearin, F. Prevalence of Functional Gastrointestinal Disorders in Women Who Report Domestic Violence to the Police. Clin. Gastroenterol. Hepatol. 2005, 3, 436–441. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.; Jones, A.; Dienemann, J.; Kub, J.; Schollenberger, J.; O’Campo, P.; Gielen, A.; Wynne, C. Intimate Partner Violence and Physical Health Consequences. Arch. Intern. Med. 2002, 162, 1157–1163. [Google Scholar] [CrossRef] [PubMed]
- Coker, A.; Smith, P.; Bethea, L.; King, M.; McKeown, R. Physical Health Consequences of Physical and Psychological Intimate Partner Violence. Arch. Fam. Med. 2000, 9, 451–457. [Google Scholar] [CrossRef]
- Wang, W.; Guo, X.; Yang, Y. Gastrointestinal Problems in Modern Wars: Clinical Features and Possible Mechanisms. Mil. Med. Res. 2015, 2, 15. [Google Scholar] [CrossRef]
- Pizarro, J.; Silver, R.; Prause, J. Physical and Mental Health Costs of Traumatic War Experiences among Civil War Veterans. Arch. Gen. Psychiatry 2006, 63, 193–200. [Google Scholar] [CrossRef]
- McLeay, S.; Harvey, W.; Romaniuk, M.; Crawford, D.; Colquhoun, D.; Young, R.; Dwyer, M.; Gibson, J.; O’Sullivan, R.; Cooksley, G.; et al. Physical Comorbidities of Post-Traumatic Stress Disorder in Australian Vietnam War Veterans. Med. J. Aust. 2017, 206, 251–257. [Google Scholar] [CrossRef]
- Goulston, K.; Dent, O.; Chapuis, P.; Chapman, G.; Smith, C.; Tait, A.; Tennant, C. Gastrointestinal Morbidity among World War II Prisoners of War: 40 Years on. Med. J. Aust. 1985, 143, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Dimsdale, J. Survivors, Victims, and Perpetrators; Hemisphere Pub. Corp.: Washington, DC, USA, 1980; pp. 142–143. [Google Scholar]
- Krystal, H. Integration and Self Healing: Affect, Trauma, Alexithymia; Analytic Press: Hilsdale, NJ, USA, 2015. [Google Scholar]
- Le, L.; Morina, N.; Schnyder, U.; Schick, M.; Bryant, R.; Nickerson, A. The Effects of Perceived Torture Controllability on Symptom Severity of Posttraumatic Stress, Depression and Anger in Refugees and Asylum Seekers: A Path Analysis. Psychiatry Res. 2018, 264, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Roemer, L.; Orsillo, S.; Borkovec, T.; Litz, B. Emotional Response at the Time of a Potentially Traumatizing Event and PTSD Symptomatology. J. Behav. Ther. Exp. Psychiatry 1998, 29, 123–130. [Google Scholar] [CrossRef]
- Salcioglu, E.; Urhan, S.; Pirinccioglu, T.; Aydin, S. Anticipatory Fear and Helplessness Predict PTSD and Depression in Domestic Violence Survivors. Psychol. Trauma Theory Res. Pract. Policy 2017, 9, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Overmier, J.; Murison, R. Anxiety and Helplessness in the Face of Stress Predisposes, Precipitates, and Sustains Gastric Ulceration. Behav. Brain Res. 2000, 110, 161–174. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.; Li, Y.; Tang, W.; Sun, Q.; Chen, L.; Wang, X.; Liu, Q.; Yu, S.; Yu, S.; Liu, C.; et al. Chronic Unpredictable Mild Stress In Rats Induces Colonic Inflammation. Front. Physiol. 2019, 10, 1228. [Google Scholar] [CrossRef]
- Lennon, E.; Maharshak, N.; Elloumi, H.; Borst, L.; Plevy, S.; Moeser, A. Early Life Stress Triggers Persistent Colonic Barrier Dysfunction and Exacerbates Colitis in Adult IL-10−/− Mice. Inflamm. Bowel Dis. 2013, 19, 712–719. [Google Scholar] [CrossRef]
- Söderholm, J.; Yang, P.; Ceponis, P.; Vohra, A.; Riddell, R.; Sherman, P.; Perdue, M. Chronic Stress Induces Mast Cell–Dependent Bacterial Adherence and Initiates Mucosal Inflammation in Rat Intestine. Gastroenterology 2002, 123, 1099–1108. [Google Scholar] [CrossRef]
- Zheng, P.; Feng, B.; Oluwole, C.; Struiksma, S.; Chen, X.; Li, P.; Tang, S.; Yang, P. Psychological Stress Induces Eosinophils to Produce Corticotrophin Releasing Hormone in the Intestine. Gut 2009, 58, 1473–1479. [Google Scholar] [CrossRef]
- Murakami, T.; Kamada, K.; Mizushima, K.; Higashimura, Y.; Katada, K.; Uchiyama, K.; Handa, O.; Takagi, T.; Naito, Y.; Itoh, Y. Changes in Intestinal Motility and Gut Microbiota Composition in a Rat Stress Model. Digestion 2017, 95, 55–60. [Google Scholar] [CrossRef]
- Stam, R.; Croiset, G.; Akkermans, L.; Wiegant, V. Sensitization of The Colonic Response to Novel Stress after Previous Stressful Experience. Am. J. Physiol. Regul. Integr. Comp. Physiol. 1996, 271, R1270–R1273. [Google Scholar] [CrossRef]
- Milde, A.; Sundberg, H.; RØseth, A.; Murison, R. Proactive Sensitizing Effects of Acute Stress on Acoustic Startle Responses and Experimentally Induced Colitis in Rats: Relationship to Corticosterone. Stress 2003, 6, 49–57. [Google Scholar] [CrossRef]
- Engel, G. Studies of Ulcerative Colitis. III. The nature of psychologic processes. Am. J. Med. 1955, 19, 231–256. [Google Scholar] [CrossRef] [PubMed]
- Satchell, L.; Kaaronen, R.; Latzman, R. An Ecological Approach to Personality: Psychological Traits as Drivers and Consequences of Active Perception. Soc. Personal. Psychol. Compass 2021, 15, e12595. [Google Scholar] [CrossRef]
- Breslau, N.; Schultz, L. Neuroticism and Post-Traumatic Stress Disorder: A Prospective Investigation. Psychol. Med. 2012, 43, 1697–1702. [Google Scholar] [CrossRef] [PubMed]
- Petruo, V.; Krauss, E.; Kleist, A.; Hardt, J.; Hake, K.; Peirano, J.; Krause, T.; Ehehalt, R.; von Arnauld de la Perriére, P.; Büning, J.; et al. Perceived distress, personality characteristics, coping strategies and psychosocial impairments in a national German multicenter cohort of patients with Crohn’s disease and ulcerative colitis. Z. Gastroenterol. 2019, 57, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Kraaij, V.; Garnefski, N.; de Wilde, E.; Dijkstra, A.; Gebhardt, W.; Maes, S.; ter Doest, L. Negative Life Events and Depressive Symptoms in Late Adolescence: Bonding and Cognitive Coping as Vulnerability Factors? J. Youth Adolesc. 2003, 32, 185–193. [Google Scholar] [CrossRef]
- Luteijn, F.; Starren, J.; Dijk, H. Handleiding Bij De NPV; Swets & Zeitlinger: Lisse, The Netherlands, 1985. [Google Scholar]
- Bennebroek Evertsz’, F.; Nieuwkerk, P.; Stokkers, P.; Ponsioen, C.; Bockting, C.; Sanderman, R.; Sprangers, M. The Patient Simple Clinical Colitis Activity Index (P-SCCAI) Can Detect Ulcerative Colitis (UC) Disease Activity in Remission: A Comparison of The P-SCCAI with Clinician-Based SCCAI and Biological Markers. J. Crohn’s Colitis 2013, 7, 890–900. [Google Scholar] [CrossRef] [PubMed]
- Marín-Jiménez, I.; Nos, P.; Domènech, E.; Riestra, S.; Gisbert, J.; Calvet, X.; Cortés, X.; Iglesias, E.; Huguet, J.; Taxonera, C.; et al. Diagnostic Performance of the Simple Clinical Colitis Activity Index Self-Administered Online at Home by Patients with Ulcerative Colitis: CRONICA-UC Study. Am. J. Gastroenterol. 2016, 111, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Walsh, A.; Ghosh, A.; Brain, A.; Buchel, O.; Burger, D.; Thomas, S.; White, L.; Collins, G.; Keshav, S.; Travis, S. Comparing Disease Activity Indices in Ulcerative Colitis. J. Crohn’s Colitis 2014, 8, 318–325. [Google Scholar] [CrossRef]
- Bennebroek Evertsz’, F.; Hoeks, C.; Nieuwkerk, P.; Stokkers, P.; Ponsioen, C.; Bockting, C.; Sanderman, R.; Sprangers, M. Development of the Patient Harvey Bradshaw Index and a Comparison with a Clinician-Based Harvey Bradshaw Index Assessment of Crohn’s Disease Activity. J. Clin. Gastroenterol. 2013, 47, 850–856. [Google Scholar] [CrossRef] [PubMed]
- Best, W. Predicting the Crohn’s Disease Activity Index from the Harvey-Bradshaw Index. Inflamm. Bowel Dis. 2006, 12, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Vermeire, S.; Schreiber, S.; Sandborn, W.; Dubois, C.; Rutgeerts, P. Correlation between the Crohn’s Disease Activity and Harvey–Bradshaw Indices in Assessing Crohn’s Disease Severity. Clin. Gastroenterol. Hepatol. 2010, 8, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Francis, C.Y.; Morris, J.; Whorwell, P.J. The irritable bowel severity scoring system: A simple method of monitoring irritable bowel syndrome and its progress. Aliment. Pharmacol. Ther. 1997, 11, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.; Mitchell, A.; Irvine, E.; Singer, J.; Williams, N.; Goodacre, R.; Tompkins, C. A New Measure of Health Status for Clinical Trials in Inflammatory Bowel Disease. Gastroenterology 1989, 96, 804–810. [Google Scholar] [CrossRef] [PubMed]
- Barlow, D.; Sauer-Zavala, S.; Carl, J.; Bullis, J.; Ellard, K. The Nature, Diagnosis, and Treatment of Neuroticism. Clin. Psychol. Sci. 2013, 2, 344–365. [Google Scholar] [CrossRef]
- Denovan, A.; Dagnall, N.; Lofthouse, G. Neuroticism and Somatic Complaints: Concomitant Effects of Rumination and Worry. Behav. Cogn. Psychother. 2018, 47, 431–445. [Google Scholar] [CrossRef]
- Shipley, B.; Weiss, A.; Der, G.; Taylor, M.; Deary, I. Neuroticism, Extraversion, and Mortality in the UK Health and Lifestyle Survey: A 21-Year Prospective Cohort Study. Psychosom. Med. 2007, 69, 923–931. [Google Scholar] [CrossRef]
- Moreno-Jiménez, B.; López Blanco, B.; Rodríguez-Muñoz, A.; Garrosa Hernández, E. The Influence of Personality Factors on Health-Related Quality of Life of Patients with Inflammatory Bowel Disease. J. Psychosom. Res. 2007, 62, 39–46. [Google Scholar] [CrossRef]
- Herman, J. Complex PTSD: A Syndrome In Survivors of Prolonged And Repeated Trauma. J. Trauma. Stress 1992, 5, 377–391. [Google Scholar] [CrossRef]
- Erozkan, A. The link between types of attachment and childhood trauma. Univers. J. Educ. Res. 2016, 4, 1071–1079. [Google Scholar] [CrossRef]
- Diamond, L.M.; Hicks, A.M.; Otter-Henderson, K. Physiological evidence for repressive coping among avoidantly attached adults. J. Soc. Pers. Relatsh. 2006, 23, 205–229. [Google Scholar] [CrossRef]
- Ehrlich, K.B. Attachment and psychoneuroimmunology. Curr Opin Psychol. 2019, 25, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Gouin, J.P.; Glaser, R.; Loving, T.J.; Malarkey, W.B.; Stowell, J.; Houts, C.; Kiecolt-Glaser, J.K. Attachment avoidance predicts inflammatory responses to marital conflict. Brain Behav. Immun. 2009, 23, 898–904. [Google Scholar] [CrossRef] [PubMed]
- Maunder, R.G.; Hunter, J.J. Attachment and psychosomatic medicine: Developmental contributions to stress and disease. Psychosom. Med. 2001, 63, 556–567. [Google Scholar] [CrossRef] [PubMed]
- Pietromonaco, P.R.; DeBuse, C.J.; Powers, S.I. Does Attachment Get Under the Skin? Adult Romantic Attachment and Cortisol Responses to Stress. Curr. Dir. Psychol. Sci. 2013, 22, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Agostini, A.; Rizzello, F.; Ravegnani, G.; Gionchetti, P.; Tambasco, R.; Straforini, G.; Ercolani, M.; Campieri, M. Adult attachment and early parental experiences in patients with Crohn’s disease. Psychosomatics. 2010, 51, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Agostini, A.; Moretti, M.; Calabrese, C.; Rizzello, F.; Gionchetti, P.; Ercolani, M.; Campieri, M. Attachment and quality of life in patients with inflammatory bowel disease. Int. J. Color. Dis. 2014, 29, 1291–1296. [Google Scholar] [CrossRef] [PubMed]
- Agostini, A.; Spuri Fornarini, G.; Ercolani, M.; Campieri, M. Attachment and perceived stress in patients with ulcerative colitis, a case-control study. J. Psychiatr. Ment. Health Nurs. 2016, 23, 561–567. [Google Scholar] [CrossRef]
- Kelstrup, A.M.; Juillerat, P.; Korzenik, J. The accuracy of self-reported medical history: A preliminary analysis of the promise of internet-based research in Inflammatory Bowel Diseases. J. Crohns Colitis 2014, 8, 349–356. [Google Scholar] [CrossRef]
- Hori, H.; Kim, Y. Inflammation and post-traumatic stress disorder. Psychiatry Clin. Neurosci. 2019, 73, 143–153. [Google Scholar] [CrossRef]

