1. Introduction
The first cases of pneumonia of unknown origin appeared in Wuhan (China) in December 2019. The etiological agent of this disease, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was identified in January 2020 [1]. Coronavirus disease 2019 (COVID-19) spread rapidly around all world, and in March 2020 the World Health Organization (WHO) declared COVID-19 as a pandemic [2].
The clinical presentation of this disease is variable, from an asymptomatic to a severe and fatal form [3]. The majority of patients are asymptomatic or present mild to moderate symptoms. However, approximately 14% of COVID-19 patients have severe presentations and 5% are critically ill with multiple organ failure and/or death [4,5].
Admission to the intensive care unit (ICU) is crucial for the survival of patients that develop serious forms of disease, especially those who develop respiratory failure (RF) requiring ventilatory support and/or other organ dysfunctions [6]. However, not all critically ill patients are admitted to the ICU. The criteria of admission depend on a patient’s characteristics, disease severity, its reversibility and ICU capacity. Therefore, the number of patients admitted to the ICU differs between hospitals, regions and countries [7,8].
Patients with underlying comorbidities appear to be more vulnerable to COVID-19 [9]. Several comorbidities, such as cardiovascular diseases, chronic kidney disease, liver disease, chronic respiratory diseases, neuromuscular diseases, solid or hematological malignancies and other primary or secondary immunodeficiencies, can influence the three stages of COVID-19 ((1) early viral illness; (2) inflammatory lung injury; (3) post-acute sequelae) by different mechanisms and consequently patients’ evolution and outcomes [10].
In oncological patients this vulnerability can be explained by an immune-compromised status inherent to oncological disease and antitumoral treatments. Additionally, nosocomial exposure associated with regular medical visits and oncological treatments in the hospital context can also contribute to the frailty of this group. Previously published studies have reported a superior mortality among COVID-19 cancer patients admitted to general hospitals as well as more severe clinical evolution, with higher rates of admission to the ICU and intubation [11,12,13,14,15,16,17,18,19,20,21].
The literature published on critically ill COVID-19 patients suggests that cancer patients have an increased risk of death [22]. However, the characteristics and outcomes of COVID-19 cancer patients admitted to the ICU remain largely unknown, with few studies published that focus on this group of patients. Therefore, this study aims to describe the clinical characteristics and outcomes of cancer patients with COVID-19 admitted to the ICU and compare them to non-cancer patients. This analysis is important from an epidemiological and clinical point of view. Furthermore, the comparison of data of critical COVID-19 cancer patients with a control group (patients without cancer) limits the confounding factors and helps to determine whether having an oncological disease is a risk factor for adverse outcomes in the intensive care setting.
2. Materials and Methods
2.1. Study Design and Patient Selection
A retrospective case–control study was performed on patients with laboratory-confirmed SARS-CoV-2 infection (by the detection of viral RNA in nasopharyngeal swab, using RT-PCR assay) admitted to the ICU of “Centro Hospitalar Universitário do Porto” (CHUPorto) from 2 March 2020 to 31 January 2021.
We included all patients admitted to the ICU in this period that were at least 18 years old and had an oncological disease (solid or hematological) diagnosed prior to hospital admission; patients with skin tumors as well as those with concomitant solid and hematological malignancies were excluded. This group (case group) was matched 1:1 on age, sex and underlying comorbidities with COVID-19 non-cancer patients (control group) admitted to the ICU of CHUPorto in the same period (Figure 1).
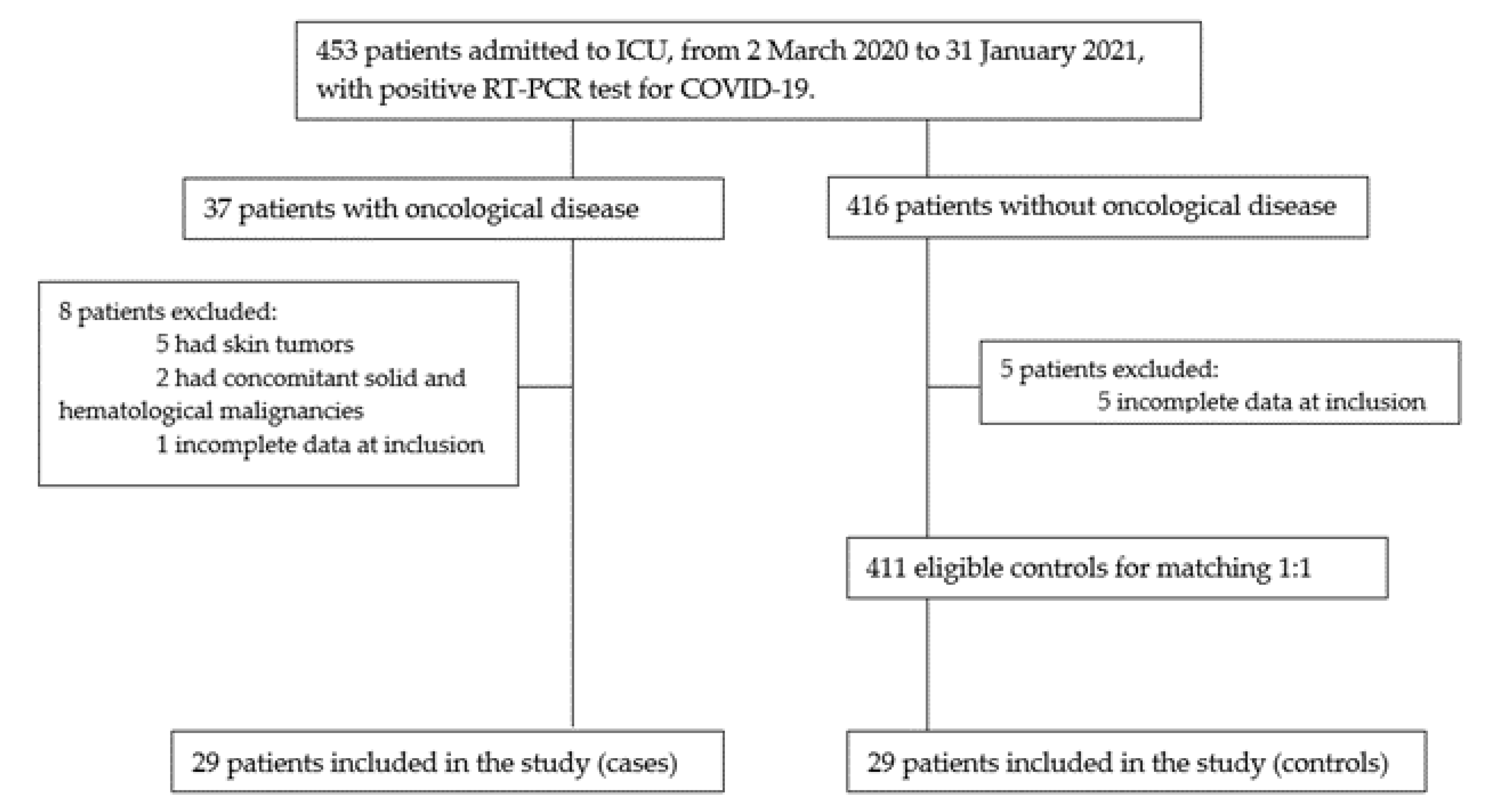
Figure 1. Flowchart of potentially eligible participants in the study.
2.2. Data Collection
Demographic, clinical, laboratorial and radiological findings were retrieved from the electronic health records. Demographic and clinical data included patient’s age, sex, comorbidities, oncological disease’s characteristics (type of cancer, primary site of malignancy, stage of tumor and status of oncological disease), prior oncological therapeutic regimens, source of SARS-CoV-2 infection, symptoms/signs of COVID-19 presentation, organ dysfunctions, COVID-19 pharmacological and non-pharmacological treatments performed in ICU, ventilatory support, complications and length of ICU stay. Laboratorial data collected included the presence of leukopenia, lymphopenia, anemia, thrombocytopenia, elevated C-reactive protein (CRP), elevated procalcitonin (PCT), elevated lactic dehydrogenase (LDH) and elevated D-dimers at ICU admission. Radiologic features on chest-computed tomography (CT) at the moment of ICU admission and laterality of abnormalities were also retrieved. Patients were followed up until they were discharged or died through their electronic health records.
An active oncological disease was defined as histologically confirmed diagnosis of cancer within 5 years prior to the COVID-19 diagnosis or receiving antitumoral treatment (chemotherapy, endocrine therapy, immunotherapy, target therapy, surgery or radiotherapy) within 5 years prior to SARS-CoV-2 infection diagnosis. Cancers were classified according to the 10th revision of the International Classification of Diseases (ICD-10). Septic shock was defined according to the 3rd International Consensus Definitions for Sepsis and Septic Shock.
2.3. Statistical Analysis
Statistical analysis was performed using IBM software—SPSS Statistics version 26.0. In a descriptive analysis, continuous variables were presented as mean and standard deviation or median and interquartile range, as appropriate. Categorical variables were presented as absolute number and percentage. The Shapiro–Wilk test was used to test the normality of distributions. The comparison of clinical, laboratorial and radiological findings between the cases and controls was performed by applying parametric (t-test) or nonparametric tests (Mann–Whitney test) for quantitative variables, as appropriated, and Chi-squared test for categorical variables. Logistic regression was used to estimate the effect of oncological disease on adverse outcomes (death, IMV need at ICU admission and IMV need during all-length of ICU stay) of COVID-19 patients admitted to the ICU. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for study participants with cancer compared to with those without cancer. A p-value < 0.05 was considered statistically significant. Initially, the authors performed a univariate analysis followed by a multivariate analysis with variables that exhibited a statistically significant difference on the univariate analysis. The multivariate analysis was adjusted for age, sex and other factors, such as anemia, thrombocytopenia, lymphopenia, elevated procalcitonin (PCT) and elevated D-dimers.
3. Results
3.1. Demographic and Clinical Characteristics
Twenty-nine COVID-19 cancer patients were hospitalized in the ICU between 2 March 2020 and 31 January 2021. These patients were enrolled in the present study and matched with 29 critical COVID-19 non-cancer patients (controls); 59% (n = 17) of cases were men and the median age was 77 years (63.5–80). Cardiovascular risk factors were the most frequent comorbidities among critical COVID-19 cancer patients. The control group presented a sex distribution, median age and prevalence of comorbidities (variables of matching) very similar to the cases .
Of the critical COVID-19 cancer patients, 79.3% (n = 23) had a solid tumor and 20.7% (n = 6) had a hematological cancer. Among solid neoplasms, 13% (n = 3) were at stage IV. According to the ICD-10 classification, malignant neoplasms of breast (13.8%, n = 4), male genital tract (13.8%, n = 4; all of them from prostate) and urinary tract (13.8%, n = 4; three from bladder and one from kidney) were the most common . Oncological active disease was present in 69% (n = 20) of participants. A variety of antitumoral treatments were performed prior to ICU admission: 69% (n = 20) received surgery, 27.6% (n = 8) radiotherapy, 27.6% (n = 8) chemotherapy, 20.7% (n = 6) hormone therapy and 3.4% (n = 1) target therapy. In addition, 24.1% (n = 7) and 20.7% (n = 6) of participants received any form of oncological treatment in the 30 days or 14 days preceding COVID-19 diagnosis, respectively.
3.2. Clinical Presentation and Laboratorial and Radiological Findings
Patients’ presenting symptoms and laboratorial and radiological findings at the moment of ICU admission are summarized in . Fever, dyspnea, cough and asthenia were the most common initial symptoms in both groups. There were no significant differences in terms of clinical presentation between the two groups. Lymphopenia and elevated LDH were the most common laboratorial findings in both groups. Anemia was significantly more frequent in cancer patients (n = 22, 75.9% vs. n = 13, 44.8%; p = 0.031). Ground-glass opacities were the most common radiological findings and were especially seen non-cancer patients (n = 10, 66.7% vs. n = 16, 100%; p = 0.018). There were no statistically meaningful differences between the rates of nosocomial source of SARS-CoV-2 infection (6.9% (n = 2) vs. 3.4% (n = 1), p = 0.553).
3.3. Treatment and Complications
Organ dysfunctions during ICU stay did not differ between the two groups, as represented in . All cases and controls had respiratory dysfunction, and cardiovascular dysfunction was the second most common in both groups.
At the moment of admission to ICU, 48.3% (n = 14) of cases vs. 6.9% (n = 2) of controls were on IMV, with a statistically significant difference (p = 0.002). However, there was no significant difference when considering the global need for IMV during all-length of ICU stay (75.9%, n = 22 vs. 55.2%, n = 16; p = 0.167). The median duration of IMV was 12 (4.75–28.75) vs. 11 (7–14) days, and patients not intubated at admission required IMV after a median time of 2 days in both groups.
COVID-19-related pharmacological and non-pharmacological treatments performed in the ICU are summarized in . A total of 75.9% (n = 22) of cases received corticosteroids during hospitalization in the ICU vs. 100% (n = 29) of controls (p = 0.005). Other drug therapies were used at a similar rate between both groups.
The median length of stay in the ICU was 8 (3–23.50) days for cancer patients and 9 (6–13.50) days for non-cancer patients (p = 0.944). The mortality rate was 58.6% vs. 37.9% for cases and controls, respectively (p = 0.276).
3.4. Effect of Oncological Disease on Outcomes
The effect of oncological disease on outcomes (death, IMV need at ICU admission and IMV need during all-length of ICU stay) was analyzed by univariate and multivariate models of logistic regression, as represented in .
The univariate analysis revealed that critical cancer patients with COVID-19 had a significantly increased risk for IMV need at ICU admission than non-cancer patients (OR = 12.600, 95% CI: 2.517–63.063, p = 0.002), but not for IMV need during all-length of ICU stay or death. The other investigated variables did not reach statistically significant differences between groups ( (Table A1)). In the adjusted multivariate model this significance was maintained (adjusted OR = 14.036, 95% CI: 1.337–153.111, p = 0.028).
4. Discussion
Cancer patients’ admission to the ICU depends on multiple factors, such as their previous performance status, comorbidities, severity of the condition that motivates ICU admission, as well as its reversibility, and the prognosis associated with the oncological disease. The limited human and material resources seen during the COVID-19 pandemic in addition to the poor prognosis conferred by some oncological diseases may have conditioned the rates of ICU admissions of cancer patients and thus the sample size of our study.
Age, sex and underlying comorbidities were the variables of matching. The median age observed in the cancer group was 77 years. The prevalence of comorbidities tends to increase with aging [22]. Several chronic diseases influence the pathological mechanisms of COVID-19 and consequently patient’s vulnerability to SARS-CoV-2 infection [10,23]. Therefore, not surprisingly, the prevalence of other chronic diseases was high amongst both groups.
The immunosuppression inherent to oncological diseases is variable. Hematological malignancies compromise the immune system, resulting in a higher susceptibility to infections [24,25,26]. In the case of solid tumor immunosuppression results, in the majority of cases, oncological treatments are administered. Studies previously published that aimed to characterize the oncological population with COVID-19 found that lung cancer was one of the most prevalent subtypes [11,12,18,25,26,27,28,29,30,31,32]. In our study, which only included patients admitted to the ICU, the most common tumors were breast cancer, male genital tract cancer and urinary tract cancer. We did not have cases of lung cancer. Patients with lung cancer have an inferior pulmonary reserve, a more severe form of COVID-19-related-lung injury, and thus a lower probability of reversing this condition [33]. These phenomena occur because the main site affected by SARS-CoV-2 is already compromised by lung cancer and/or oncological treatments [32], which, in turn, renders the benefit from invasive measures smaller and contributes to explaining the differences between the prevalence of cancer subtypes in the general population and the oncological patients admitted to the ICU.
Given an increased contact with hospital settings, we were expecting to find a higher prevalence of health-care-associated SARS-CoV-2 infections in the cancer group. However, there was no statistical difference regarding the source of infection between cancer patients and controls. This may be explained by measures adopted at the beginning of the pandemic, such as teleconsultation regimens (especially for patients under surveillance), the concentration of medical appointments/exams/treatments in order to avoid multiple hospital contacts, prolonged prescriptions and the implementation of viral RNA research by RT-PCR assay prior to hospital admissions or treatments.
Lymphopenia is considered a prominent laboratorial marker of severe COVID-19 and was the most common analytical alteration observed in both groups [34,35]. The second most frequent laboratorial abnormality was the LDH elevation. In severe SARS-CoV-2 infection, multiple organ dysfunction leads to cellular hypoxia and cell damage, which, conjugated with lung injury due to acute respiratory distress syndrome (ARDS), culminate with LDH release [36]. We highlight that anemia is not one of the most common findings in SARS-CoV-2 infection, but it occurred in 76% of cancer patients, which was significantly superior to the frequency observed in the control group [37]. This finding suggests that, in addition to the inflammatory component subsequent to a severe infection in a critically ill patient, oncological disease could also have an impact either by direct medullar invasion, medullar suppression following oncological treatments and/or by cancer-associated malnutrition.
According to Liang et al., COVID-19 cancer patients presented a higher risk of severe events (ICU admission and need for IMV and death) than non-cancer patients—39% vs. 8% [12]. However, the authors highlight that the comparison between cancer and non-cancer patients did not consider confounding factors, such as age, sex and comorbidities. In order to minimize the influence of these confounding factors we matched these variables between critical COVID-19 cancer patients and controls.
The mortality rates reported in previously conducted studies ranged from 10% to 84% in the COVID-19 population admitted to the ICU [38]. When considering the oncological population admitted to the ICU it ranged from 25% to 100%, with a pooled mortality of 60.2% in a meta-analysis which included 28 studies (1 276 patients) [39]. In the present analysis, 59% of critical COVID-19 cancer patients died, which is in concordance with the previously mentioned data. According to the available literature, COVID-19 cancer patients admitted to the ICU had a significantly higher mortality compared to non-cancer patients (59.8% vs. 42.3%) [39]. In the present study, the mortality was also superior amongst cancer patients, but did not reach statistical significance (59% vs. 38%, p = 0.276). Nadkarni et al. and Plais et al. reported that the presence of an oncologic disease significantly increased the risk of death (OR = 4.144, 95% CI: 1.24–13.83) [39,40]. However, the logistic regression model applied here revealed that the impact of cancer on mortality was not significant. The small sample size could help to explain the different results. The time from ICU admission to death was superior in controls (8 vs. 13 days), suggesting a more rapid evolution to death in the oncological patients’ group, although without statistical significance.
IMV need at the moment of ICU admission was significantly higher among cancer patients (48% vs. 7%, p = 0.002). The global need for IMV during all-length of ICU stay was superior in the cancer patients, but without statistical significance (76% vs. 55%, p = 0.167). The level of significance persisted in a multivariate logistic regression. These findings suggest that cancer patients evolve more rapidly to severe RF that requires IMV at ICU admission, but not more frequently than those without an oncologic disease.
We expected to find a superior rate of infectious complications among cancer patients, due to the additional immune-compromised status inherent to oncological disease and antitumoral treatments. Nevertheless, the rate of secondary infections did not differ significantly between the two groups (69% vs. 59%, p = 0.414). In addition to the immunosuppression conferred by a severe SARS-CoV-2 infection, the high rate of corticosteroid administration in the control group (76% vs. 100%, p = 0.005) probably contributed to the susceptibility to secondary infections.
COVID-19 and cancer are both prothrombotic diseases [41]. Therefore, we were expecting to find an increased rate of thromboembolic events in the case group. However, the occurrence of these events was identical (3% vs. 10%, p = 0.300). This finding might be associated with the prophylactic usage of an intermediate dose of low-molecular-weight heparin, popular during the pandemic.
The authors remind that the present study has limitations: we conducted a retrospective analysis, with a small sample size, with a 1:1 matching. In addition, to increase sample size, the authors had to include patients with both solid and hematological malignancies, thus providing heterogeneity to the sample, as the courses are different between those types of tumors. In consequence, further prospective, multicentric studies with larger samples and arms differentiating hematological and solid malignancies, if possible, are necessary to reinforce the results obtained here.
5. Conclusions
Our findings showed that cancer patients had an increased risk for IMV need at the moment of ICU admission, however, not for IMV need during all-length of ICU stay or death. Nevertheless, the mortality of COVID-19 cancer patients was not superior to that of non-cancer patients, stressing the importance of an aggressive early treatment of oncologic patients. The decision on ICU admission must be individualized, considering the performance status of the patient, the stage of neoplasm, the intention of oncological treatments and the severity and potential of reversibility of COVID-19. Further multicentric studies are needed to shed light on why critical COVID-19 patients with cancer evolve more rapidly to IMV.
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Singhal, T. A Review of Coronavirus Disease-2019 (COVID-19). Indian J. Pediatr. 2020, 87, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72,314 Cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Aiyegbusi, O.L.; Hughes, S.E.; Turner, G.; Rivera, S.C.; McMullan, C.; Chandan, J.S.; Haroon, S.; Price, G.; Davies, E.H.; Nirantharakumar, K.; et al. Symptoms, complications and management of long COVID: A review. J. R. Soc. Med. 2021, 114, 428–442. [Google Scholar] [CrossRef]
- Hajjar, L.A.; Costa, I.B.S.D.S.; Rizk, S.I.; Biselli, B.; Gomes, B.R.; Bittar, C.S.; Oliveira, G.Q.; Almeida, J.P.; Oliveira Bello, M.V.; Garzillo, C.; et al. Intensive care management of patients with COVID-19: A practical approach. Ann. Intensive Care. 2021, 11, 36. [Google Scholar] [CrossRef]
- Azoulay, E.; Waele, J.; Ferrer, R.; Staudinger, T.; Borkowska, M.; Povoa, P.; Iliopoulou, K.; Artigas, A.; Schaller, S.J.; Shankar-Hari, M.; et al. International variation in the management of severe COVID-19 patients. Crit. Care. 2020, 24, 486. [Google Scholar] [CrossRef]
- Heo, J.; Han, D.; Kim, H.J.; Kim, D.; Lee, Y.K.; Lim, D.; Hong, S.O.; Park, M.J.; Ha, B.; Seog, W. Prediction of patients requiring intensive care for COVID-19: Development and validation of an integer-based score using data from Centers for Disease Control and Prevention of South Korea. J. Intensive Care. 2021, 9, 16. [Google Scholar] [CrossRef]
- Yang, L.; Chai, P.; Yu, J.; Fan, X. Effects of cancer on patients with COVID-19: A systematic review and meta-analysis of 63,019 participants. Cancer Biol. Med. 2021, 18, 298–307. [Google Scholar] [CrossRef]
- Russell, C.D.; Lone, N.I.; Baillie, J.K. Comorbidities, multimorbidity and COVID-19. Nat. Med. 2023, 29, 334–343. [Google Scholar] [CrossRef]
- Dai, M.; Liu, D.; Liu, M.; Zhou, F.; Li, G.; Chen, Z.; Zhang, Z.; You, H.; Wu, M.; Zheng, Q.; et al. Patients with Cancer Appear More Vulnerable to SARS-CoV-2: A Multicenter Study during the COVID-19 Outbreak. Cancer Discov. 2020, 10, 783–791. [Google Scholar] [CrossRef]
- Liang, W.; Guan, W.; Chen, R.; Wang, W.; Li, J.; Xu, K.; Li, C.; Ai, Q.; Lu, W.; Liang, H.; et al. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020, 21, 335–337. [Google Scholar] [CrossRef]
- Tian, J.; Yuan, X.; Xiao, J.; Zhong, Q.; Yang, C.; Liu, B.; Cai, Y.; Lu, Z.; Wang, J.; Wang, Y.; et al. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: A multicentre, retrospective, cohort study. Lancet Oncol. 2020, 21, 893–903. [Google Scholar] [CrossRef]
- Yang, K.; Sheng, Y.; Huang, C.; Jin, Y.; Xiong, N.; Jiang, K.; Lu, H.; Liu, J.; Yang, J.; Dong, Y.; et al. Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: A multicentre, retrospective, cohort study. Lancet Oncol. 2020, 21, 904–913. [Google Scholar] [CrossRef] [PubMed]
- Kuderer, N.; Choueiri, T.; Shah, D.; Shyr, Y.; Rubinstein, S.M.; Rivera, D.R.; Shete, S.; Hsu, C.Y.; Desai, A.; Lima Lopes, G.; et al. Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet 2020, 395, 1907–1918. [Google Scholar] [CrossRef] [PubMed]
- Meng, Y.; Lu, W.; Guo, E.; Liu, J.; Yang, B.; Wu, P.; Lin, S.; Peng, T.; Fu, Y.; Li, F.; et al. Cancer history is an independent risk factor for mortality in hospitalized COVID-19 patients: A propensity score-matched analysis. J. Hematol. Oncol. 2020, 13, 75. [Google Scholar] [CrossRef] [PubMed]
- Garassino, M.C.; Whisenant, J.G.; Huang, L.C.; Trama, A.; Torri, V.; Agustoni, F.; Baena, J.; Banna, G.; Berardi, R.; Bettini, A.C.; et al. COVID-19 in patients with thoracic malignancies (TERAVOLT): First results of an international, registry-based, cohort study. Lancet Oncol. 2020, 21, 914–922. [Google Scholar] [CrossRef]
- Zhang, L.; Zhu, F.; Xie, L.; Wang, C.; Wang, J.; Chen, R.; Jia, P.; Guan, H.Q.; Peng, L.; Chen, Y.; et al. Clinical characteristics of COVID-19-infected cancer patients: A retrospective case study in three hospitals within Wuhan, China. Ann. Oncol. 2020, 31, 894–901. [Google Scholar] [CrossRef]
- Richards, M.; Anderson, M.; Carter, P.; Ebert, B.L.; Mossialos, E. The impact of the COVID-19 pandemic on cancer care. Nat. Cancer 2020, 1, 565–567. [Google Scholar] [CrossRef]
- Arayici, M.E.; Kipcak, N.; Kayacik, U.; Kelbat, C.; Keskin, D.; Kilicarslan, M.E.; Kilinc, A.V.; Kirgoz, S.; Kirilmaz, A.; Kizilkaya, M.A.; et al. Effects of SARS-CoV-2 infections in patients with cancer on mortality, ICU admission and incidence: A systematic review with meta-analysis involving 709,908 participants and 31,732 cancer patients. J. Cancer Res. Clin. Oncol. 2022, 13, 1–14. [Google Scholar] [CrossRef]
- Liu, C.; Zhao, Y.; Okwan-Duodu, D.; Basho, R.; Cui, X. COVID-19 in cancer patients: Risk, clinical features, and management. Cancer Biol. Med. 2020, 17, 519–527. [Google Scholar] [CrossRef]
- Lenti, M.V.; Klersy, C.; Brera, A.S.; Ballesio, A.; Croce, G.; Padovini, L.; Ciccocioppo, R.; Bertolino, G.; Di Sabatino, A.; Corazza, G.R. Aging underlies heterogeneity between comorbidity and multimorbidity frameworks. Intern. Emerg. Med. 2022, 17, 1033–1041. [Google Scholar] [CrossRef] [PubMed]
- Xia, Y.; Jin, R.; Zhao, J.; Li, W.; Shen, H. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020, 21, e180. [Google Scholar] [CrossRef] [PubMed]
- Malard, F.; Genthon, A.; Brissot, E.; van de Wyngaert, Z.; Marjanovic, Z.; Ikhlef, S.; Banet, A.; Lapusan, S.; Sestilli, S.; Corre, E.; et al. COVID-19 outcomes in patients with hematologic disease. Bone Marrow Transplant. 2020, 55, 2180–2184. [Google Scholar] [CrossRef]
- Höllein, A.; Bojko, P.; Schulz, S.; Neitz, J.; Stötzer, O.; Pihusch, R.; Abedinpour, F.; Schmidt, B.; Hentrich, M. Characteristics and outcomes of patients with cancer and COVID-19: Results from a cohort study. Acta Oncol. 2021, 60, 24–27. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.Y.W.; Cazier, J.B.; Starkey, T.; Briggs, S.E.W.; Arnold, R.; Bisht, V.; Booth, S.; Campton, N.A.; Cheng, V.W.T.; Collins, G.; et al. COVID-19 prevalence and mortality in patients with cancer and the effect of primary tumour subtype and patient demographics: A prospective cohort study. Lancet Oncol. 2020, 21, 1309–1316. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Wang, L.; Chen, Y.; Shen, X.; Wang, Q.; Yan, Y.; Yu, Y.; Wu, Q.; Zhong, Y.; Chua, M.L.K.; et al. A multicentre study of 2019 novel coronavirus disease outcomes of cancer patients in Wuhan, China. MedRxiv 2020, 41, 145. [Google Scholar]
- Stroppa, E.M.; Toscani, I.; Citterio, C.; Anselmi, E.; Zaffignani, E.; Codeluppi, M.; Cavanna, L. Coronavirus disease-2019 in cancer patients. A report of the first 25 cancer patients in a western country (Italy). Future Oncol. 2020, 16, 1425–1432. [Google Scholar] [CrossRef]
- Rogado, J.; Obispo, B.; Pangua, C.; Serrano-Montero, G.; Martín Marino, A.; Pérez-Pérez, M.; López-Alfonso, A.; Gullón, P.; Lara, M.Á. COVID-19 transmission, outcome and associated risk factors in cancer patients at the first month of the pandemic in a Spanish hospital in Madrid. Clin. Transl. Oncol. 2020, 22, 2364–2368. [Google Scholar] [CrossRef]
- Rogado, J.; Pangua, C.; Serrano-Montero, G.; Obispo, B.; Marino, A.M.; Pérez-Pérez, M.; López-Alfonso, A.; Gullón, P.; Lara, M.Á. COVID-19 and lung cancer: A greater fatality rate? Lung Cancer 2020, 146, 19–22. [Google Scholar] [CrossRef]
- Yarza, R.; Bover, M.; Paredes, D.; López-López, F.; Jara-Casas, D.; Castelo-Loureiro, A.; Baena, J.; Mazarico, J.M.; Folgueira, M.D.; Meléndez-Carmona, M.Á.; et al. SARS-CoV-2 infection in cancer patients undergoing active treatment: Analysis of clinical features and predictive factors for severe respiratory failure and death. Eur. J. Cancer 2020, 135, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Lemos, A.E.G.; Silva, G.R.; Gimba, E.R.P.; Matos, A.D.R. Susceptibility of lung cancer patients to COVID-19: A review of the pandemic data from multiple nationalities. Thorac. Cancer. 2021, 12, 2637–2647. [Google Scholar] [CrossRef] [PubMed]
- Passaro, A.; Bestvina, C.; Velez Velez, M.; Garassino, M.C.; Garon, E.; Peters, S. Severity of COVID-19 in patients with lung cancer: Evidence and challenges. J. Immunother. Cancer. 2021, 9, e002266. [Google Scholar] [CrossRef]
- Zhao, Q.; Meng, M.; Kumar, R.; Wu, Y.; Huang, J.; Deng, Y.; Weng, Z.; Yang, L. Lymphopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A systemic review and meta-analysis. Int. J. Infect. Dis. 2020, 96, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Jafarzadeh, A.; Jafarzadeh, S.; Nozari, P.; Mokhtari, P.; Nemati, M. Lymphopenia an important immunological abnormality in patients with COVID-19: Possible mechanisms. Scand. J. Immunol. 2021, 93, e12967. [Google Scholar] [CrossRef]
- Szarpak, L.; Ruetzler, K.; Safiejko, K.; Hampel, M.; Pruc, M.; Kanczuga-Koda, L.; Filipiak, K.J.; Jaguszewski, M.J. Lactate dehydrogenase level as a COVID-19 severity marker. Am. J. Emerg. Med. 2021, 45, 638–639. [Google Scholar] [CrossRef]
- Zuin, M.; Rigatelli, G.; Quadretti, L.; Fogato, L.; Zuliani, G.; Roncon, L. Prognostic Role of Anemia in COVID-19 Patients: A Meta-Analysis. Infect. Dis. Rep. 2021, 13, 930–937. [Google Scholar] [CrossRef]
- Armstrong, R.A.; Kane, A.D.; Cook, T.M. Outcomes from intensive care in patients with COVID-19: A systematic review and meta-analysis of observational studies. Anaesthesia 2020, 75, 1340–1349. [Google Scholar] [CrossRef]
- Nadkarni, A.R.; Vijayakumaran, S.C.; Gupta, S.; Divatia, J.V. Mortality in Cancer Patients With COVID-19 Who Are Admitted to an ICU or Who Have Severe COVID-19: A Systematic Review and Meta-Analysis. JCO Glob. Oncol. 2021, 7, 1286–1305. [Google Scholar] [CrossRef]
- Plais, H.; Labruyère, M.; Creutin, T.; Nay, P.; Plantefeve, G.; Tapponnier, R.; Jonas, M.; Ngapmen, N.T.; Le Guennec, L.; De Roquetaillade, C.; et al. Outcomes of Patients with Active Cancer and COVID-19 in the Intensive-Care Unit: A Multicenter Ambispective Study. Front. Oncol. 2022, 12, 858276. [Google Scholar] [CrossRef]
- Zavras, P.D.; Mehta, V.; Goel, S.; Pradhan, K.; Billett, H.H. Increased Incidence of Thrombosis in a Cohort of Cancer Patients with COVID-19. Acta Haematol. 2022, 145, 152–159. [Google Scholar] [CrossRef] [PubMed]

