1. Introduction
Hip fracture is a medical condition associated with mortality and poor functional outcomes. According to the International Osteoporosis Foundation, 1.6 million hip fractures were recorded worldwide in 2000, and this number is expected to increase to 4.5–6.3 million by 2050 because of the ageing of the population [1,2]. The mortality risk from a hip fracture persists beyond 5 years, and the 1-year mortality rate is estimated to be 20–24% [3,4]. Among patients who experience hip fractures, 40% cannot walk independently, 60% require assistance, and 33% are completely dependent or living in a nursing home 1 year after they experience the hip fracture [3,5,6].
COVID-19 is an infectious disease transmitted through air droplets and small airborne particles. The first known COVID-19 infection occurred on 31 December 2019 in China [7]. The COVID-19 pandemic was a burden on healthcare systems worldwide. Orthopedic clinics performed fewer elective and nonelective surgeries during the COVID-19 pandemic. However, orthopedic surgeries for trauma cases were still performed. The number of older adult patients presenting to hospitals with hip fractures was the same during the COVID-19 pandemic as it was before the pandemic, even in regions that experienced severe outbreaks of the virus [8]. Moldovan et al. conducted a multicenter study in Romania in 2023 and found that the COVID-19 pandemic has had a severe impact on the volume of elective arthroplasty cases in Romania’s 120 hospitals, with a dramatic decrease in the volume of primary interventions for hip and knee patients of up to 69.14% and a corresponding decline in the quality of patient care [9]. The COVID-19 pandemic has influenced patterns of care and health outcomes among patients with hip fractures [10].
In Taiwan, the COVID-19 pandemic reached a critical stage in March 2022. To prevent the spread of the virus, the government implemented strict hospital care and visitation policies. These policies influenced the quality of care, including daily living care and bedside rehabilitation, received by patients with hip fractures. An inferior quality of care has been associated with increased mortality, adverse outcomes, and poor functional improvement.
We hypothesized that the COVID-19 pandemic has led to the launch of policies that could affect hip fracture postoperative care. This includes nursing care and family care, where a decrease in the number of early bedside rehabilitation programs may further increase mortality and poor functional outcomes. Our study aimed to compare mortality and functional outcomes between patients with and without COVID-19 after surgery for hip fractures in our medical center during the COVID-19 pandemic apex in Taiwan.
2. Materials and Methods
2.1. Study Design and Population
We conducted this prospective cohort study in a single medical center in eastern Taiwan, enrolling patients aged 60 and above who were diagnosed with hip fractures between 9 March 2022 and 9 September 2022. The patients with pertrochanteric fractures received open reduction and internal fixation with a cephalomedullary nail, while the patients with displaced femoral neck fractures received hemiarthroplasty. Patients with high-energy trauma, periprosthetic or peri-implant fractures, as well as those who did not undergo surgery or underwent revision surgery for a prior hip fracture, were excluded from the study. The patients’ data were included, collected, and classified, as shown in Figure 1.
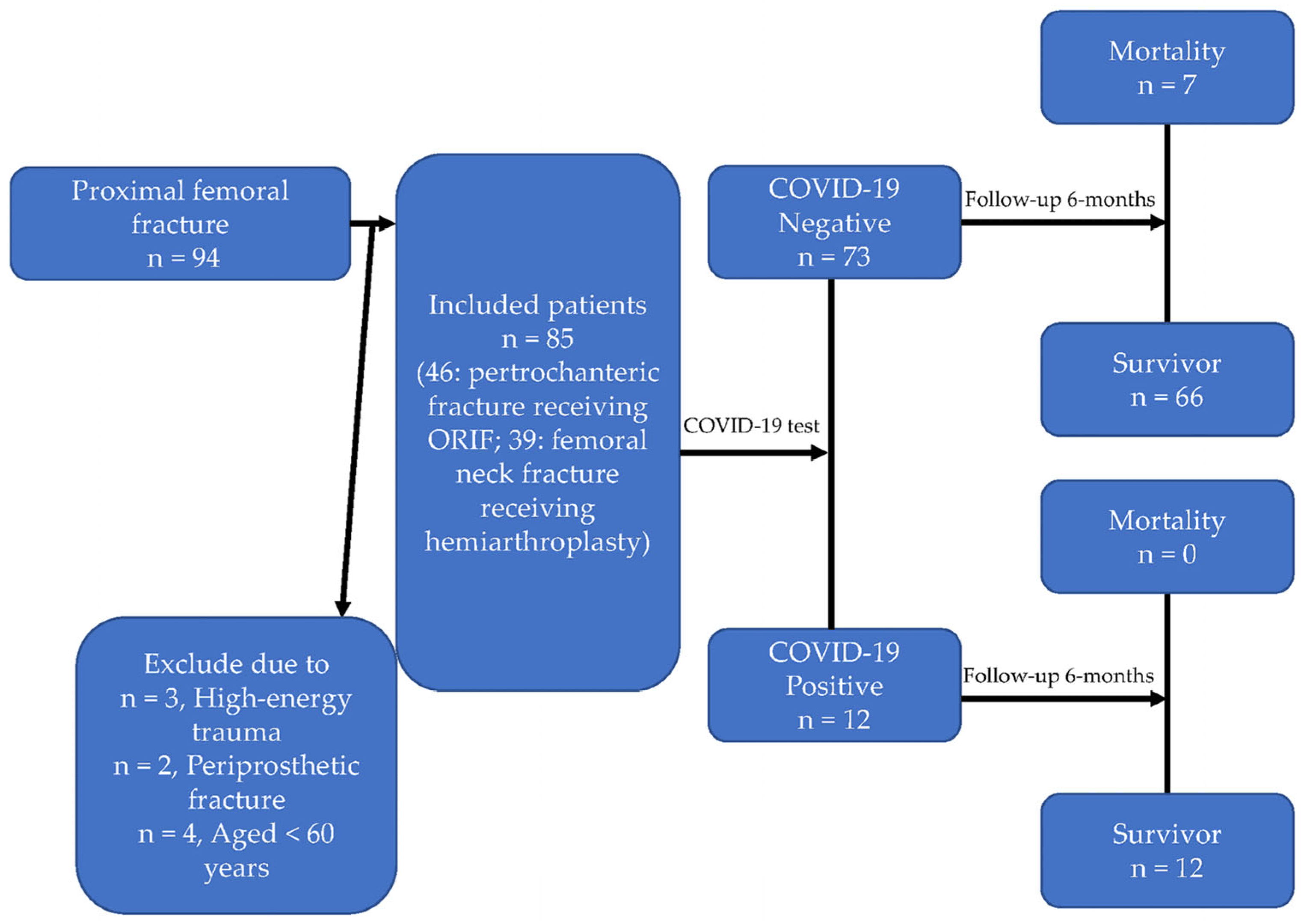
Figure 1. Flowchart of this study.
2.2. Data Collection
Demographic and clinical data were meticulously extracted from electronic medical records. Preoperative functional scores were assessed upon patient admission through validated tools. Follow-up postoperative functional scores were obtained during scheduled outpatient consultations or structured telephone interviews conducted by trained medical staff. The parameters were as listed as below: (1) preoperative data: age, gender, body mass index, fracture type, American Society of Anesthesiologists grade, blood chemistry, Charlson comorbidity index, Barthel index score (activities of daily living), Eastern Cooperative Oncology Group (ECOG) score, and COVID-19 status, as confirmed using polymerase chain reaction tests; (2) operative data: surgical approach, anesthesia type, use of a nerve block, preoperative NPO time, time from admission to operation, the duration of the operation, anesthesia time, estimated blood loss, and immediate postoperative hemoglobin levels; (3) postoperative data: the length of hospital stay, complication incidence (e.g., pneumonia, sepsis, acute urinary retention, ileus, electrolyte imbalance, urinary tract infection, anemia, moderate to severe hip pain), mortality, and postoperative functional scores (ECOG, Barthel index, and modified Harris hip score).
2.3. Statistical Analysis
All statistical analyses were performed using SPSS version 23.0 (IBM, Armonk, NY, USA). The descriptive statistics included continuous variables presented as means ± standard deviations and categorical variables shown as numbers and percentages. The univariate analysis included Student’s t-test, employed for comparing continuous variables between groups, and chi-square tests, used for categorical variables. The multivariable analysis included a multiple linear regression analysis conducted to assess the impact of the covariates and postoperative comorbidities on changes in the ECOG, Barthel index, and Harris hip scores, with adjustments made for potential confounders. The variable selection was based on a stepwise backward elimination process. The outcome analysis included logistic regression models used to identify factors independently associated with mortality, adjusted for confounding variables. Odds ratios and 95% confidence intervals were reported for all the logistic regression analyses. Statistical significance was defined as a p-value of <0.05, and all tests were two-tailed.
3. Results
This study comprised 85 patients, 12 of whom (14.12%) were COVID-19-positive. There were 29 (34.1%) males and 56 (65.9%) females with a mean age of 79.42 years and mean body mass index of 22.58 ± 3.72 kg/m2 . In total, 39 (45.9%) of them had femoral pertrochanteric fractures and 46 (54.1%) had femoral neck fractures . No statistically significant differences in age, body mass index, gender, ASA grade, fracture type, Charlson comorbidity index score, comorbidity status, preoperative blood chemistry data, or preoperative Barthel index score were observed between the COVID-19-positive and -negative groups .
The COVID-19-negative group had a shorter anesthesia time than the positive group (137.73 ± 32.30 vs. 158.25 ± 40.24 min, p = 0.046; . No statistically significant differences in the surgical method, anesthesia method, use of perioperative nerve block, preoperative NPO time, time to operation, operation time, blood loss, or hemoglobin level were observed between the COVID-19-positive and -negative groups . The postoperative Barthel index scores were significantly lower in the COVID-19-positive group (74.58 ± 17.64) than in the negative group (88.03 ± 16.82) (p = 0.014; . No significant differences in the length of hospital stay, incidence of complications, ECOG status, Harris hip score, or mortality rate were observed between the groups .
Subgroup analyses were performed to investigate the relationships between postoperative complications and functional outcomes after 6 months in terms of the ECOG, Barthel index, and Harris hip score. A higher incidence of complications was associated with general anesthesia (β: 0.50, 95% confidence interval (CI): 0.06–0.94, p = 0.026) and a longer length of hospital stay (β: 0.04, 95% CI: 0.01–0.06, p = 0.004) . Poor ECOG status was associated with a lower preoperative Barthel index score (β: −0.03, 95% CI: −0.04 to −0.02, p < 0.001) . A lower postoperative Barthel index score was correlated with COVID-19 infection (β: −15.59, 95% CI: −24.29 to −6.89, p = 0.001), a higher Charlson comorbidity index score (β: −3.30, 95% CI: −5.18 to −1.42, p = 0.001), and a lower preoperative Barthel index score (β: 0.65, 95% CI: 0.43–0.87, p < 0.001) . A lower postoperative Harris hip score was correlated with COVID-19 infection (β: −8.20, 95% CI: −16.75 to −0.35, p = 0.048), a higher Charlson comorbidity index score (β: −1.78, 95% CI: −3.62 to −0.07, p = 0.049), and a lower preoperative Barthel index (β: 0.36, 95% CI: 0.15–0.58, p = 0.001) . We investigated the factors which were associated with postoperative mortality. After adjustment for various factors, age (adjusted odd ratio (aOR): 1.25, 95% CI: 1.001–1.55, p = 0.049), gender (aOR: 342.45, 95% CI: 3.56–32910.44, p = 0.012), ASA grade (aOR: 28.96, 95% CI: 1.42–590.37, p = 0.029), and Charlson comorbidity index score (aOR: 0.22, 95% CI: 0.06–0.85, p = 0.028) were closely associated with postoperative mortality .
4. Discussion
In our study, we noticed that time to operation did not significantly differ between the positive and negative groups (1.58 ± 0.51 vs. 1.38 ± 0.39 days, respectively). No significant differences were observed in the length of hospital stay or postoperative complications between the groups. Kim discovered that during the COVID-19 pandemic, hip fracture surgeries were postponed for 24 to 36 h, and the rate of postoperative complications did not increase [11]. Wang observed no change in the 30-day mortality rate, time to surgery, or length of hospital stay in a level-1 trauma center in the United States before, during, and after the COVID-19 pandemic [8]. However, a systematic review of 11 cohort studies and a total of 336 patients discovered that the in-hospital mortality rate of hip fracture patients was 29.8% (95% CI: 26.6−35.6%), the 30-day postoperative mortality rate was 35% (95% CI: 29.9−40.5%), and the average hospital stay was 11.29 days [12]. Another systematic review and meta-analysis discovered that patients with hip fractures who had concomitant COVID-19 infection had a 34% short-term mortality rate [13]. Mastan et al. found that COVID-19 status was associated with a 4-fold increase in mortality among patients with hip fractures [14]. In a study conducted by Raheman, patients with hip fractures who had COVID-19 had a 4-fold risk of mortality (risk ratio: 4.59, p < 0.0001), and the 30-day mortality rate was 38% (hazard ratio: 4.73, p < 0.0001). Raheman et al. discovered that male sex, diabetes, dementia, and extracapsular fractures were risk factors for mortality in patients with COVID-19 [15]. However, in our study, the mortality rate did not significantly differ between patients who had COVID-19 and those who did not have COVID-19. None of the seven patients who died had COVID-19.
The postoperative Barthel index score was significantly lower in the COVID-19-positive group (74.58 ± 17.64) than in the COVID-19-negative group. The postoperative Barthel index score and Harris hip score were associated with COVID-19 status . Two factors may have contributed to this result. First, COVID-19 may have made the patients more vulnerable to health problems or caused their existing health problems to worsen. Second, the delayed initiation of rehabilitation may have had a significant impact on the surgical results because of the isolation policy for COVID-19 infection. Early mobilization is essential for the optimal postoperative management of patients with hip fractures, including activities such as getting in and out of bed, performing sit-to-stand exercises, rising from chairs with assistance, and walking with the aid of a walker [16,17,18,19]. Patients with hip fractures experience an average loss of muscle strength in their affected limbs of more than 50% in the first postoperative week [20,21,22,23].
The COVID-19 pandemic clearly impacted surgical treatment for patients with a hip pathology. Moldovan et al. quantified the effects of COVID-19 on elective arthroplasty interventions in Romania. He found that the COVID-19 pandemic had a severe impact on the volume of elective arthroplasty cases in Romania’s 120 hospitals [9], and this impact had significant financial ramifications for the hospitals. The author proposed the development of new clinical procedures and personalized home recovery programs for future outbreaks. Telemedicine through virtual consultations may also be integrated into emergency orthopedics in the future to maintain the care quality of patients during infectious disease pandemics [24,25]. The COVID-19 pandemic has placed unprecedented strain on healthcare systems worldwide, affecting various medical specialties, including orthopedics [26]. The pandemic apex has led to specific challenges in managing hip fractures among older adults in Taiwan in terms of both surgical quality and postoperative care. In terms of the impact of hip fractures on surgical quality, it can be divided into four parts: (1) Resource Allocation and Triage: The pandemic has forced many hospitals to reprioritize surgeries, with centers often postponing elective surgeries to focus on emergency cases [27]. In Taiwan, this has impacted the availability of resources like surgical suites, specialized orthopedic teams, and even equipment, which could potentially affect the surgical outcomes for hip fractures. (2) Surgical Delays: With hospitals at or near capacity due to COVID-19 patients, surgical delays have become common. A study in the Journal of Bone and Joint Surgery indicated that even a delay of just over 48 h could lead to a significant increase in 30-day mortality rates for hip fractures [28]. Delays may be exacerbated if the patient is COVID-19-positive, given the need for special protocols and isolation measures. (3) Surgical Technique and Team Experience: Due to the need for staff redeployment to care for COVID-19 patients, less experienced teams may sometimes handle surgeries, possibly affecting the surgical outcomes. Additionally, some studies suggest that less invasive surgical techniques might be preferred during pandemic conditions to reduce the operation time and hospital stay, although this could affect long-term outcomes [29]. (4) Perioperative Care: Special precautions have to be taken if the patient is COVID-19-positive. These include changes in anesthesia protocols and more intensive monitoring, which could affect the overall surgical experience and potentially lead to complications [30]. In terms of the impact on postoperative care quality for hip fractures, it can be divided into six parts: (1) Hospital Stay: During the pandemic’s apex, the focus was on reducing the length of hospital stays to free up beds. Quick discharge protocols may not always align with the optimal recovery paths for hip fracture patients, especially older adults, who often have comorbid conditions requiring complex care [9]. (2) Physical Rehabilitation: Given the social distancing norms and limitations on in-person interactions, physical rehabilitation schedules may be disrupted. A meta-analysis study in Medicine indicates that reduced postoperative mobility can lead to complications such as joint stiffness and an increased fall risk [31]. (3) Psychological Impact: Isolation due to COVID-19 protocols, coupled with the natural apprehension arising from being in a hospital during a pandemic, can lead to mental health issues like depression or anxiety [32]. These psychological factors can adversely affect postoperative recovery. (4) Follow-Up and Long-Term Care: Telehealth has often replaced in-person consultations for follow-up care, but not all aspects of postoperative care can be adequately managed remotely [24]. Moreover, older adults may face challenges in accessing or using digital platforms. (5) Economic Impact: In Taiwan, as elsewhere, the economic repercussions of the pandemic have led to funding cuts and resource allocation changes that could affect the quality of postoperative care. (6) Complications: According to an article in the World Journal of Orthopedics, the incidence of postoperative complications like pneumonia, urinary tract infections, or deep vein thrombosis may rise due to the strains and changes in standard care protocols during a pandemic [33]. As Taiwan navigates the challenges of COVID-19, innovative strategies like tele-rehabilitation, personalized home-based recovery plans, and the integration of artificial intelligence into the monitoring of postoperative care are becoming more relevant. Research and healthcare policies must adapt to ensure that the surgical and postoperative care quality of hip fracture patients is not compromised, irrespective of pandemic conditions. The apex of the COVID-19 pandemic has had a multifaceted impact on the quality of surgical and postoperative care for hip fractures in Taiwan. With shifting resources and strained healthcare systems, the implications are vast and warrant urgent attention to mitigate adverse outcomes.
The COVID-19 pandemic has significantly disrupted healthcare systems, and its impact extends beyond immediate medical care to longer-term functional outcomes in various patient groups. Patients recovering from surgeries often require extensive postoperative care, including physical therapy [31]. The pandemic has led to limitations in access to physical rehabilitation services due to social distancing measures and the diversion of healthcare resources. A study in Clinical Rehabilitation has indicated that this reduction in physical therapy access can have negative implications for long-term functional recovery, especially in the first 6 months post-surgery, which is a critical period for regaining function [34]. For patients with chronic conditions like COPD, diabetes, or heart disease, routine care and regular exercise are vital for maintaining functional ability. A study in Experimental Gerontology found that the interruption of regular healthcare visits and reduced physical activity due to lockdown measures can result in deteriorated functional quality over a 6-month period [35]. For instance, decreased exercise can exacerbate issues with glycemic control in diabetics, and reduced pulmonary rehabilitation can affect respiratory function in COPD patients. Regarding COVID-19 survivors, a number of studies have examined the “long COVID” phenomenon, where symptoms persist for months after the initial infection has resolved [36]. These symptoms can range from fatigue and muscle weakness to difficulties with concentration and memory, all affecting functional quality. A study in The Lancet Global Health found that even mild cases of COVID-19 can have lingering functional impacts up to 6 months after recovery, affecting the ability to return to work and carry out daily activities [37]. Elderly patients are at high risk of functional decline due to both age and an increased susceptibility to COVID-19. Social isolation measures, although necessary, have contributed to reduced physical activity, and studies in The Journal of Frailty & Aging have highlighted how this inactivity can lead to rapid functional decline in elderly populations [38]. The pandemic also had a widespread psychological impact, exacerbating conditions like depression and anxiety, which can have a direct effect on physical health and functional ability [39]. Psychological stress can influence pain perception, sleep quality, and overall well-being, factors that are critical in functional recovery from any illness or surgical intervention [32]. The above conditions may explain why the apex of the COVID-19 pandemic had a profound impact on the 6-month functional quality of patients with hip fractures in our study. Reduced access to healthcare services, interruptions in routine care, and the lingering effects of COVID-19 itself pose challenges that need urgent attention. Telemedicine and home-based care models are emerging as potential alternatives, but there is a dire need for more research in order to understand how to effectively mitigate these functional impairments.
This study has several limitations. First, this was a single-center study with a small sample (n = 85). The unexpected phenomenon whereby all the patients who died were in the COVID-19-negative group is due to the small sample size. Second, this study compared patients with and without COVID-19 during the pandemic and did not evaluate patients before the pandemic. Third, we did not include other parameters such as bone density, sarcopenia, and nutrition status that may have also impacted the patients’ postoperative function scores. In the future, we could design a matching study to reduce the bias from other interfering causes. The strength of our study is that it is based on real-world data obtained during patient admission and during follow-up in the outpatient clinic department or using telephone interviews. Few studies have investigated functional outcomes in patients with hip fractures who have COVID-19. Our study provides information on the association between functional outcomes and COVID-19 in patients with hip fractures.
5. Conclusions
At our hospital, orthopedic surgeries were not unduly delayed during the COVID-19 pandemic. No significant differences in the length of hospital stay, postoperative complications, or mortality were observed between patients with and without COVID-19. The key finding of this study is that among patients with hip fractures, those with COVID-19 may have worse functional outcomes in terms of the Barthel index and Harris hip score than those without COVID-19.
References
- Cooper, C.; Campion, G.; Melton, L.J., 3rd. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 1992, 2, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Gullberg, B.; Johnell, O.; Kanis, J.A. World-wide projections for hip fracture. Osteoporos. Int. 1997, 7, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Leibson, C.L.; Tosteson, A.N.; Gabriel, S.E.; Ransom, J.E.; Melton, L.J. Mortality, disability, and nursing home use for persons with and without hip fracture: A population-based study. J. Am. Geriatr. Soc. 2002, 50, 1644–1650. [Google Scholar] [CrossRef] [PubMed]
- Magaziner, J.; Lydick, E.; Hawkes, W.; Fox, K.M.; Zimmerman, S.I.; Epstein, R.S.; Hebel, J.R. Excess mortality attributable to hip fracture in white women aged 70 years and older. Am. J. Public Health 1997, 87, 1630–1636. [Google Scholar] [CrossRef] [PubMed]
- Riggs, B.L.; Melton, L.J., 3rd. The worldwide problem of osteoporosis: Insights afforded by epidemiology. Bone 1995, 17 (Suppl. S5), 505S–511S. [Google Scholar] [CrossRef]
- Magaziner, J.; Simonsick, E.M.; Kashner, T.M.; Hebel, J.R.; Kenzora, J.E. Predictors of functional recovery one year following hospital discharge for hip fracture: A prospective study. J. Gerontol. 1990, 45, M101–M107. [Google Scholar] [CrossRef]
- Cheng, S.C.; Chang, Y.C.; Fan Chiang, Y.L.; Chien, Y.C.; Cheng, M.; Yang, C.H.; Huang, C.H.; Hsu, Y.N. First case of Coronavirus Disease 2019 (COVID-19) pneumonia in Taiwan. J. Formos. Med. Assoc. 2020, 119, 747–751. [Google Scholar] [CrossRef]
- Wang, K.C.; Xiao, R.; Cheung, Z.B.; Barbera, J.P.; Forsh, D.A. Early mortality after hip fracture surgery in COVID-19 patients: A systematic review and meta-analysis. J. Orthop. 2020, 22, 584–591. [Google Scholar] [CrossRef]
- Moldovan, F.; Gligor, A.; Moldovan, L.; Bataga, T. An Investigation for Future Practice of Elective Hip and Knee Arthroplasties during COVID-19 in Romania. Medicina 2023, 59, 314. [Google Scholar] [CrossRef]
- Zhong, H.; Poeran, J.; Liu, J.; Wilson, L.A.; Memtsoudis, S.G. Hip fracture characteristics and outcomes during COVID-19: A large retrospective national database review. Br. J. Anaesth. 2021, 127, 15–22. [Google Scholar] [CrossRef]
- Kim, K.K.; Lee, S.W.; Choi, J.K.; Won, Y.Y. Epidemiology and postoperative complications of hip fracture during COVID-19 pandemic. Osteoporos. Sarcopenia 2022, 8, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Tayyebi, H.; Hasanikhah, M.; Heidarikhoo, M.; Fakoor, S.; Aminian, A. Length of hospital stay and mortality of hip fracture surgery in patients with Coronavirus disease 2019 (COVID-19) infection: A systematic review and meta-analysis. Curr. Orthop. Pract. 2022, 33, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Isla, A.; Landy, D.; Teasdall, R.; Mittwede, P.; Albano, A.; Tornetta, P., 3rd; Bhandari, M.; Aneja, A. Postoperative mortality in the COVID-positive hip fracture patient, a systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 927–935. [Google Scholar] [CrossRef]
- Mastan, S.; Hodhody, G.; Sajid, M.; Malik, R.; Charalambous, C.P. COVID-19 Is Associated With a 4-Fold Increase in 30-day Mortality Risk in Hip Fracture Patients in the United Kingdom: A Systematic Review and Meta-Analysis. Geriatr. Orthop. Surg. Rehabil. 2022, 13, 21514593221099375. [Google Scholar] [CrossRef] [PubMed]
- Raheman, F.J.; Rojoa, D.M.; Nayan Parekh, J.; Berber, R.; Ashford, R. Meta-analysis and metaregression of risk factors associated with mortality in hip fracture patients during the COVID-19 pandemic. Sci. Rep. 2021, 11, 10157. [Google Scholar] [CrossRef]
- Parker, M.; Johansen, A. Hip fracture. BMJ 2006, 333, 27–30. [Google Scholar] [CrossRef]
- Mak, J.C.; Cameron, I.D.; March, L.M.; National Health and Medical Research Council. Evidence-based guidelines for the management of hip fractures in older persons: An update. Med. J. Aust. 2010, 192, 37–41. [Google Scholar] [CrossRef]
- Ftouh, S.; Morga, A.; Swift, C.; Guideline Development Group. Management of hip fracture in adults: Summary of NICE guidance. BMJ 2011, 342, d3304. [Google Scholar] [CrossRef]
- Swierstra, B.A.; Vervest, A.M.; Walenkamp, G.H.; Schreurs, B.W.; Spierings, P.T.; Heyligers, I.C.; van Susante, J.L.; Ettema, H.B.; Jansen, M.J.; Hennis, P.J.; et al. Dutch guideline on total hip prosthesis. Acta. Orthop. 2011, 82, 567–576. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Bandholm, T.; Bencke, J.; Ekdahl, C.; Kehlet, H. Knee-extension strength, postural control and function are related to fracture type and thigh edema in patients with hip fracture. Clin. Biomech. 2009, 24, 218–224. [Google Scholar] [CrossRef]
- Lamb, S.E.; Morse, R.E.; Evans, J.G. Mobility after proximal femoral fracture: The relevance of leg extensor power, postural sway and other factors. Age Ageing. 1995, 24, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, C.; Lord, S.R.; Herbert, R.D. A randomised trial of weight-bearing versus non-weight-bearing exercise for improving physical ability in inpatients after hip fracture. Aust. J. Physiother. 2003, 49, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Kronborg, L.; Bandholm, T.; Palm, H.; Kehlet, H.; Kristensen, M.T. Feasibility of progressive strength training implemented in the acute ward after hip fracture surgery. PLoS ONE 2014, 9, e93332. [Google Scholar] [CrossRef] [PubMed]
- Rizkalla, J.M.; Gladnick, B.P.; Bhimani, A.A.; Wood, D.S.; Kitziger, K.J.; Peters, P.C., Jr. Triaging Total Hip Arthroplasty during the COVID-19 Pandemic. Curr. Rev. Musculoskelet. Med. 2020, 13, 416–424. [Google Scholar] [CrossRef]
- Teo, S.H.; Abd Rahim, M.R.; Nizlan, N.M. The impact of COVID-19 pandemic on orthopaedic specialty in Malaysia: A cross-sectional survey. J. Orthop. Surg. 2020, 28, 2309499020938877. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, F.; Gligor, A.; Moldovan, L.; Bataga, T. The Impact of the COVID-19 Pandemic on the Orthopedic Residents: A Pan-Romanian Survey. Int. J. Environ. Res. Public Health. 2022, 19, 9176. [Google Scholar] [CrossRef] [PubMed]
- Shih, C.L.; Huang, P.J.; Huang, H.T.; Chen, C.H.; Lee, T.C.; Hsu, C.H. Impact of the COVID-19 pandemic and its related psychological effect on orthopedic surgeries conducted in different types of hospitals in Taiwan. J. Orthop. Surg. 2021, 29, 2309499021996072. [Google Scholar] [CrossRef]
- Siegmeth, A.W.; Gurusamy, K.; Parker, M.J. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J. Bone Jt. Surg. Br. 2005, 87, 1123–1126. [Google Scholar] [CrossRef]
- Qin, H.C.; He, Z.; Luo, Z.W.; Zhu, Y.L. Management of hip fracture in COVID-19 infected patients. World J. Orthop. 2022, 13, 544–554. [Google Scholar] [CrossRef]
- Shin, S.; Kim, S.H.; Park, K.K.; Kim, S.J.; Bae, J.C.; Choi, Y.S. Effects of Anesthesia Techniques on Outcomes after Hip Fracture Surgery in Elderly Patients: A Prospective, Randomized, Controlled Trial. J. Clin. Med. 2020, 9, 1605. [Google Scholar] [CrossRef]
- Liu, Y.; Yang, Y.; Liu, H.; Wu, W.; Wu, X.; Wang, T. A systematic review and meta-analysis of fall incidence and risk factors in elderly patients after total joint arthroplasty. Medicine 2020, 99, e23664. [Google Scholar] [CrossRef] [PubMed]
- Hwang, T.J.; Rabheru, K.; Peisah, C.; Reichman, W.; Ikeda, M. Loneliness and social isolation during the COVID-19 pandemic. Int. Psychogeriatr. 2020, 32, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Obamiro, E.; Trivedi, R.; Ahmed, N. Changes in trends of orthopedic services due to the COVID-19 pandemic: A review. World J. Orthop. 2022, 13, 955–968. [Google Scholar] [CrossRef] [PubMed]
- Berggren, M.; Karlsson, Å.; Lindelöf, N.; Englund, U.; Olofsson, B.; Nordström, P.; Gustafson, Y.; Stenvall, M. Effects of geriatric interdisciplinary home rehabilitation on complications and readmissions after hip fracture: A randomized controlled trial. Clin. Rehabil. 2019, 33, 64–73. [Google Scholar] [CrossRef]
- Markotegi, M.; Irazusta, J.; Sanz, B.; Rodriguez-Larrad, A. Effect of the COVID-19 pandemic on the physical and psychoaffective health of older adults in a physical exercise program. Exp. Gerontol. 2021, 155, 111580. [Google Scholar] [CrossRef]
- Sykes, D.L.; Holdsworth, L.; Jawad, N.; Gunasekera, P.; Morice, A.H.; Crooks, M.G. Post-COVID-19 Symptom Burden: What Is Long-COVID and How Should We Manage It? Lung 2021, 199, 113–119. [Google Scholar] [CrossRef]
- Dryden, M.; Mudara, C.; Vika, C.; Blumberg, L.; Mayet, N.; Cohen, C.; Tempia, S.; Parker, A.; Nel, J.; Perumal, R.; et al. Post-COVID-19 condition 3 months after hospitalisation with SARS-CoV-2 in South Africa: A prospective cohort study. Lancet Glob. Health 2022, 10, e1247–e1256. [Google Scholar] [CrossRef]
- Risbridger, S.; Walker, R.; Gray, W.K.; Kamaruzzaman, S.B.; Ai-Vyrn, C.; Hairi, N.N.; Khoo, P.L.; Pin, T.M. Social Participation’s Association with Falls and Frailty in Malaysia: A Cross-Sectional Study. J. Frailty Aging 2022, 11, 199–205. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Martínez-González, M.B.; Benitez-Agudelo, J.C.; Navarro-Jiménez, E.; Beltran-Velasco, A.I.; Ruisoto, P.; Diaz Arroyo, E.; Laborde-Cárdenas, C.C.; Tornero-Aguilera, J.F. The Impact of the COVID-19 Pandemic on Mental Disorders. A Critical Review. Int. J. Environ. Res. Public Health 2021, 18, 10041. [Google Scholar] [CrossRef]

