1. Introduction
The re-emergence of bacteriophages (phages) for the treatment of chronic or difficult-to-treat infections and diseases has been extensively observed in recent years. Phages are viruses that specifically target and kill host bacteria. They serve as a possible alternative to antibiotics in the treatment of bacterial infections, especially in this era where there is a lack of new and effective antibiotics to combat the rise of multidrug-resistant (MDR) bacteria. The term “MDR” refers to organisms that are resistant to at least one antibiotic agent from three or more antibiotic classes [1]. Extensively drug-resistant (XDR) and pan-drug-resistant (PDR) bacteria are also used to categorize bacterial resistance, of which XDR bacteria are non-susceptible to at least one agent in all but two or fewer antibiotic categories, and PDR bacteria are resistant to an agent from all antibiotic classes [2].
The development of phage therapy as an alternative to traditional antibiotics has gained substantial interest over the years. However, its ultimate success in clinical use relies on evidence that proves phage therapy is safe and non-toxic for humans. A major safety concern is the disruption of the body’s microbiome, which is a key regulator of human health. Another concern is the impact of phage on the immune system, which may ultimately lead to chronic inflammation and other immune reactions. As phages are prepared by co-culturing with bacteria, it is crucial to consider the potential risk of endotoxin contamination that could trigger the inflammatory cytokine response, resulting in serious health issues such as toxic shock [3]. Additionally, the use of temperate phages may produce bacterial lysogens that are resistant to the same phage type, potentially increasing their virulence [4].
Recent studies have shown that phages are generally safe and do not produce any adverse effects when used in animals or humans [5,6,7,8]. Nevertheless, a few studies have reported transient adverse events or side effects during phage therapy, which include inflammation, flushing, hypotension, and fever [9,10,11]. The absence of a standard protocol to evaluate the safe usage and preparation of phages results in a lack of consistent, complete, and reliable data to conclude the safety aspect of phage therapy. Hence, a rigorous and detailed exploration of phage safety is required to guide treatment decisions.
In this review, we discuss the advancement, importance, and current applications of phages. Phage applications in clinical settings, the food and agricultural sector (e.g., prevention), and environmental control (e.g., biosensors) are reviewed. It also focuses on the safety concerns and challenges of translating phages from the bench to clinical bedside applications. The topics that are included are the disruption of the microbiome, immunological responses, induction of phage resistance in bacteria, lysogeny, and contaminants (e.g., endotoxins) associated with phage preparation. The environmental safety issue related to phage release is also briefly discussed.
2. The Era of Phages
2.1. An Alternative to Antibiotic
Ever since the discovery of the “wonder drug” penicillin, antibiotics have been the first line of defense against bacterial infections. Indeed, virtually everyone alive today has grown up in the antibiotic era. However, the overuse of antibiotics has inadvertently led to the emergence of MDR bacteria. For example, infections caused by Acinetobacter baumannii such as pneumonia, meningitis, and sepsis have traditionally been treated with beta-lactams [12,13]. However, MDR A. baumannii strains, including those resistant to beta-lactams, are increasingly reported; hence, last-line antibiotics such as polymyxins are prescribed for their treatment [14,15]. Thus, A. baumannii is listed by the World Health Organization (WHO) as a priority pathogen for which new antibiotics are urgently needed, along with other bacteria such as Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, and Pseudomonas aeruginosa, collectively referred to as the ‘ESKAPE’ pathogens [16]. As MDR bacteria become more prevalent among human populations, they pose a serious threat to clinical and public health, thus becoming a major global health issue. With only a handful of new antibiotics on the horizon [4], there is a growing need to explore alternative antimicrobial strategies, of which phage therapy has become increasingly apparent.
Phages are the most abundant and diverse biological entities that are present on Earth [17]. Phages are highly specific, and they are loosely categorized into monovalent or polyvalent phages depending on their host range. Monovalent phages are defined as phages that have a narrow host range spectrum specific to a single bacterial genus, whereas polyvalent phages are phages that have a broad host range specific to more than two genera [18]. For example, FAHEc1 is a monovalent phage that only targets Escherichia coli and can be used to reduce contamination in beef, whereas S5 and vB_EcoM_swi3 are polyvalent and target both Salmonella and E. coli [19,20,21]. Phages exhibit different life cycles, including the lytic cycle, chronic cycle, lysogenic cycle, and pseudolysogenic cycle [22]. Worth noting, lytic phages are often favored for phage therapy due to their ability to effectively lyse bacteria [15].
2.2. Current Phage Applications
Ever since the discovery of phages, researchers have taken advantage of their abundance and infection specificity to combat pathogenic bacteria, mainly for treating bacterial infections, preventing food contamination, and for environmental control. With the emergence of MDR bacteria, research examining phages as an alternative to antibiotics has once again begun in earnest, with the current application of phages against these “superbugs” briefly discussed below.
3. Safety Concerns and Challenges
Despite successful cases of treatment with phage therapy, the safety and potential side effects pose a significant challenge to its broader application, especially for clinical use. The concerns associated with the human body include the impact of phage on the microbiome, lysis-induced endotoxin release, immune activation, and increased bacterial resistance. Phage usage may also have environmental implications.
3.1. Human Body
3.2. Temperate Phages
Lytic phages are unanimously preferred over temperate phages for therapy purposes. The administration of temperate phages may not be favored due to their intrinsic nature, which favors the lysogenic cycle, in which their genomes are integrated into the bacterial genome and do not lead to immediate bacterial killing. Importantly, bacterial lysogens often exhibit resistance to subsequent infections by phages [4]. Superinfection exclusion and superinfection immunity are the mechanisms that prevent superinfecting phages from either entering the bacterial cell or blocking their infection cycle within the bacterial cell [66].
Temperate phages have the ability to obtain ARGs and virulence genes from the infected host and subsequently transfer them to other bacterial hosts. This process can inevitably lead to the widespread distribution of these factors among bacteria, contributing to the development of difficult-to-treat MDR bacteria. Hence, it is advisable to refrain from using temperate phages in phage treatment until more comprehensive research is available to guide their application. In fact, researchers have been exploring phage engineering techniques to modify temperate phages, making them safe and effective for use in phage therapy.
3.3. Induction of Phage-Resistant Bacteria
As phages are increasingly employed for the treatment of bacterial infections, it has unavoidably led to the emergence of phage-resistant bacteria. It has been reported that bacteria can develop phage resistance through various mechanisms, which include receptor alterations, abortive infection systems, bacteriophage exclusion (BREX), and quorum sensing defense [105]. An example of receptor alteration is observed in Bordetella spp. that prevents infection from phage BPP-1 by suppressing the expression of the phage receptor pertactin autotransporter (Prn) [106]. The abortive infection (Abi) system is a strategy that induces host cell death, thus limiting phage propagation. An example of Abi involves the toxin-antitoxin systems, of which Erwinia carotovora subspecies atrosepticawa was found to consist of a toxI gene that encodes for an antitoxin that neutralizes ToxN [107,108]. The BREX defense system is another mechanism that has been increasingly reported. Bacillus cereus consists of six-gene cassettes called BREX defense systems that are subject to substantial horizontal gene transfer and offer total phage resistance to a variety of phages, including lytic and temperate phages [105]. A summary of the mechanism of phage resistance in relation to the life cycle of phages is presented in Figure 1.
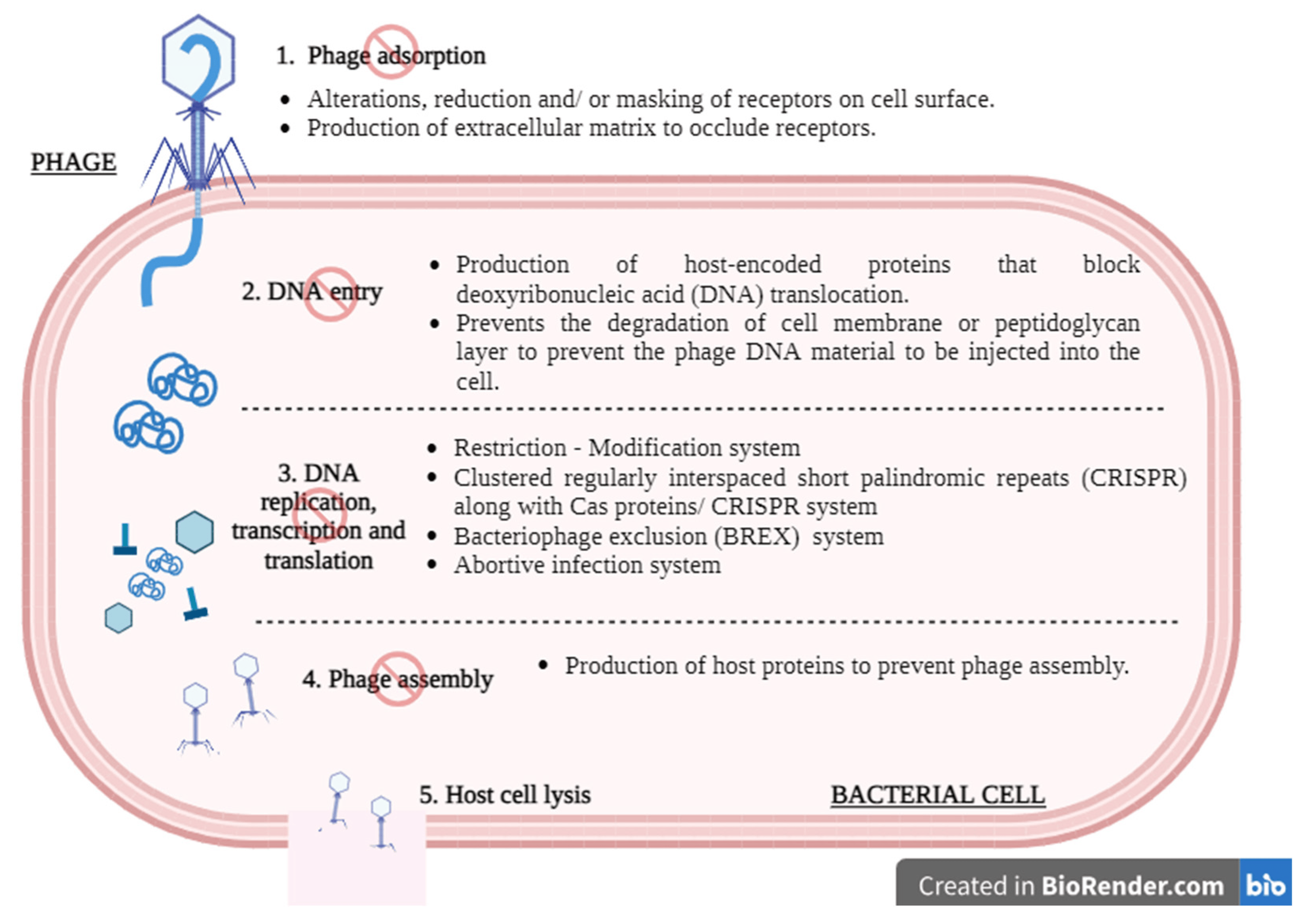
Figure 1. A schematic illustration of the mechanism of phage resistance in relation to the general lytic phage cycle. (1) Phages can attach to the surface of host bacteria using receptor-binding proteins (RBPs). Bacterial cells have various ways to disrupt this attachment process, such as by alternating, reducing, and/or masking their receptors on the surface of the cell. (2) During translocation, phage DNA is directly injected into the host cell’s cytoplasm. Certain bacterial strains can hinder this injection by employing proteins encoded by the host that interfere with the transfer of phage nucleic acid. (3) Once inside the host cytoplasm, phage DNA undergoes preparation for replication. Whether the phage DNA is modified or unmodified, it can be degraded by host-encoded proteins following its translocation into the host cytoplasm. Normally, replication, transcription, and translation of the phage DNA will proceed as usual. However, bacterial cells may be able to resist this action through the initiation of the Restriction–Modification system, the CRISPR system, the BREX system, or the abortive infection system. (4) Assembly and packaging are crucial steps in the production of new phage particles. Certain bacterial strains express proteins that interfere with the assembly or packaging process of the newly synthesized virions. These proteins disrupt the proper formation of the phage capsid or the packaging of phage DNA into the capsid. (5) If the lytic phages manage to pass through all the bacterial defenses, it will eventually lead to host cell lysis. Created with Biorender.com.
3.4. Environmental Impact
The application of phage therapy may directly or indirectly affect ecosystem biodiversity as phages are released into the environment; however, there is limited research on the environmental impact.
Research has been conducted to compare the disposal of therapeutic phages and broad-spectrum chemical antibiotics in the environment. There has been an increasing focus on antibiotic surveillance and investigations into strategies for appropriate antibiotic disposal [109]. The presence of antibiotic traces in the environment, such as surface and ocean waters, has resulted in increasing public concern due to the potential for promoting the emergence of MDR bacteria. Contrary to antibiotics, discarded therapeutic phages are said to only have a minimal effect on a small group of bacteria as they are often originally isolated from the environment. Furthermore, phages can be rapidly inactivated if they are not adapted to harsh environmental factors, such as extreme temperature, humidity, and UV light [66]. Worth mentioning is that phages are able to withstand a wide range of temperatures (generally 40–70 °C) [110], therefore making them more thermally stable in comparison to antibiotics.
Although phages are naturally present in the environment, the release of high phage concentrations as a result of phage therapy could potentially cause an imbalance in the ecosystem by disrupting the natural microbial balance [111]. Hence, proper waste management represents an essential area that should be put in place to protect the environment and safeguard public health.
4. Studies on Phage Safety
Several animal studies [6,8,83], case reports [5,7,10], and clinical trials [13] have been conducted to monitor the safety of phages in the treatment of MDR bacteria.
4.1. Animal Studies
Murine and sheep are often used as animal models for studying phage safety. The use of the sheep model provides an advantage over the more commonly used murine model as it is one of the most significant representations of human organ systems, providing a more accurate assessment of phage safety in humans.
Phage therapy has been demonstrated to be safe and effective in treating pathogenic E. coli, P. aeruginosa, S. aureus, and A. baumannii in sheep and mouse models [6,83]. Utilizing a murine model, phage 536_P1 successfully eradicated E. coli infection without inducing an innate inflammatory response [83]. In another study conducted by Yin et al. (2017), phage Abp1 was effective in eliminating MDR A. baumannii in mice without eliciting any cytotoxic effects [8]. Employing a sheep rhinosinusitis model, the administration of a phage cocktail locally at the sinus for treating P. aeruginosa infection resulted in no significant adverse effects, such as loss of appetite, fever, or other signs of systemic illness [6]. Similarly, the treatment of S. aureus-associated rhinosinusitis in sheep with the phage cocktail NOV012 was not associated with tissue damage or inflammatory infiltration [112]. Details for these animal studies are summarized in .
4.2. Clinical Cases
Multiple case studies have included phage safety monitoring. Liu et al. (2021) have conducted one of the first systematic literature reviews on phage therapy clinical cases where phage safety monitoring alongside treatment is included [113]. These case studies mostly involve patients with conditions such as cystic fibrosis, prosthetic knee infections (PKI), urinary tract infections (UTI), surgery/transplant-related wound infections, and abscesses.
As endotoxins are a major source of phage contamination that may lead to adverse effects during therapy, several case reports have reported the endotoxin level of the phage products used for clinical treatment. While most of the studies reported endotoxin levels within the FDA limits [10,114,115], dilutions were required by some phage products to achieve safe endotoxin levels [11,30,116]. The process of diluting phages to adhere to clinical endotoxin limits results in a reduced phage concentration, potentially compromising the effectiveness of therapy [94]. Due to the lack of standardization, some studies do not include this safety aspect in their research, and consequently, endotoxin levels are not reported [5,117].
In one study, inflammatory changes were assessed following IV and/or intraarticular (IA) administration of SaGR51Φ1, along with antibiotic administration. This study reported no significant inflammatory effect except for a transient, reversible transaminitis [10]. Most cases have reported little to no significant adverse reactions or that the effects were not phage-related . Of note, transient fever represents the most associated adverse effect reported; however, fever is a common physiological response to infection.
Overall, it is crucial that standardized therapeutic guidelines are made available to promote consistency and uniformity in monitoring the safety profile of phage therapy, enabling a more reliable conclusion to be drawn.
4.3. Clinical Trials
Clinical studies that evaluate the safety aspects of phage therapy are scarce. In a clinical trial to test the efficacy and safety of phage therapy for treating urinary tract infections caused by MDR uropathogens (Enterococcus spp., E. coli, Proteus mirabilis, P. aeruginosa, Staphylococcus spp., and Streptococcus spp.), patients were subjected to either receiving Pyo phage (intravesically), placebo, or antibiotics [134]. The lowest occurrence of adverse effects was demonstrated by the phage group (21%; 6/28) in comparison to the placebo (41%; 13/32) and antibiotic (30%; 11/37) groups. Another phage therapy clinical trial was conducted on patients with MRSA infections. The safety aspects that were considered in this study include pain and systemic adverse reactions [135]. When patients were treated with phage AB-SA01, no adverse events were reported, although there was a notable decrease in inflammation markers and an increase in cytokine interactions. In a clinical trial involving the treatment of chronic ear infections caused by antibiotic-resistant P. aeruginosa, Biophage-PA significantly reduced the bacterial load, and no phage-related adverse effects were observed [136]. The details of these clinical trials are shown in . The presented clinical studies were chosen based on the criteria that they are recent studies involving phage therapy, specifically related to MDR bacterial infections, and that they evaluate the safety aspect of phage therapy.
5. Challenges and Future Improvements
Difficulties arise when attempting to compare the data across published clinical cases and clinical trials, as different studies employ their own set of treatment and monitoring protocols [113]. In order to improve current practices, the establishment of a gold standard or standard operating procedure is of paramount importance to guide phage preparation, storage, and transport, as well as the monitoring criteria for determining the efficacy and safety of phage therapy. The purified phage lysate should also adhere to the Good Manufacturing Practice (GMP) guidelines to ensure safety [129].
When phage products are used for therapeutic purposes, information such as the phage genome, titer, purity, and endotoxin level should be made available. Insufficient and incomplete data regarding phage safety monitoring represents another limitation to fully understanding the safety profile of phage therapy. The safety endpoints that can be included are evaluation of the patient’s physical symptoms, chemical lab assessment (e.g., kidney and liver function tests, electrolytes, and inflammation markers), hematology lab assessment (e.g., complete blood count), and immunological response evaluation (e.g., antibodies) [113]. The availability of this comprehensive data would permit a more thorough safety assessment of phage therapy, thus facilitating policymakers’ efforts to establish a comprehensive regulatory framework for phage treatment [137].
Phages are often used in combination with antibiotics to achieve better antibacterial activity [5,87,117], achieved by phage-antibiotic synergy (PAS) [138]. For instance, Uchiyama et al. (2018) evaluated phage-antibiotic combinations against P. aeruginosa and observed that combining piperacillin and ceftazidime with P. aeruginosa phage KPP22 showed the strongest PAS [139]. Understanding the mechanisms underlying PAS is the key to designing phage-antibiotic therapy. Utilizing metabolomics, it was revealed that the combination of polymyxin B and phage pK8 caused a prolonged inhibition of the citrate cycle, pentose phosphate pathway, and amino acid and nucleotide metabolism of K. pneumoniae [140]. It should also be noted that antagonistic phage-antibiotic combinations are often overlooked. A recent study by Zuo et al. (2021) showed that replication of coliphage T3 was impeded by aminoglycoside antibiotics (e.g., neomycin and kanamycin), which inhibit protein synthesis [141]. Overall, careful consideration and more research are needed to inform appropriate concentrations, application timing, and optimal selection of phages and antibiotics based on patients’ diagnoses and medical histories.
In order to further advance the field of phage therapy, it is essential to establish comprehensive phage libraries consisting of a diverse array of phages that are known to be safe and effective against bacterial infections. By having such accessible repositories of phages, the potential for finding suitable phages can be significantly enhanced.
6. Conclusions
Since their discovery, phages have been extensively utilized in the agricultural and environmental sectors to ensure food safety and effective pathogen control. Phages have also re-emerged as an alternative to antibiotics due to the emergence of MDR bacteria. As phage therapy research against MDR bacteria advances quickly, ensuring its safety in clinical applications becomes an absolute priority.
The recent success of in vivo studies, case reports, and clinical trials has demonstrated that phages exhibit a relatively safe profile and are typically tolerable when administered to animals and humans. These encouraging findings solidify the foundation for the broader application of phage therapy as a safe and well-tolerated treatment modality. Given existing knowledge gaps and limited data on the potential health implications of phage therapy, it will be imperative to address and overcome the safety concerns discussed in this paper. It is also vital to establish and implement standardized safety assessments. By adhering to consistent and rigorous safety evaluation protocols, researchers can effectively address any uncertainties and validate the reliability of phage therapy, reinforcing its position as a trustworthy medical approach.
Nonetheless, ongoing research in the phage field enables researchers to enhance their comprehension of the safety aspects surrounding phage therapy for combating MDR bacteria. While there remains a considerable journey before phage therapy becomes an established standard of clinical care, it is crucial to continue expanding the knowledge base and facilitating the translatability of phages from bench-side to clinical bedside applications.
References
- Sweeney, M.T.; Lubbers, B.V.; Schwarz, S.; Watts, J.L. Applying definitions for multidrug resistance, extensive drug resistance and pandrug resistance to clinically significant livestock and companion animal bacterial pathogens. J. Antimicrob. Chemother. 2018, 73, 1460–1463. [Google Scholar] [CrossRef] [PubMed]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- De Tejada, G.M.; Heinbockel, L.; Ferrer-Espada, R.; Heine, H.; Alexander, C.; Bárcena-Varela, S.; Goldmann, T.; Correa, W.; Wiesmüller, K.; Gisch, N.; et al. Lipoproteins/peptides are sepsis-inducing toxins from bacteria that can be neutralized by synthetic anti-endotoxin peptides. Sci. Rep. 2015, 5, 14292. [Google Scholar] [CrossRef] [PubMed]
- Ling, H.; Lou, X.; Luo, Q.; He, Z.; Sun, M.; Sun, J. Recent advances in bacteriophage-based therapeutics: Insight into the post-antibiotic era. Acta Pharm. Sin. B 2022, 12, 4348–4364. [Google Scholar] [CrossRef] [PubMed]
- Ferry, T.; Kolenda, C.; Batailler, C.; Gustave, C.A.; Lustig, S.; Malatray, M.; Fevre, C.; Josse, J.; Petitjean, C.; Chidiac, C.; et al. Phage Therapy as Adjuvant to Conservative Surgery and Antibiotics to Salvage Patients with Relapsing S. aureus Prosthetic Knee Infection. Front. Med. 2020, 7, 570572. [Google Scholar] [CrossRef]
- Fong, S.A.; Drilling, A.J.; Ooi, M.L.; Paramasivan, S.; Finnie, J.W.; Morales, S.; Psaltis, A.J.; Vreugde, S.; Wormald, P. Safety and efficacy of a bacteriophage cocktail in an in vivo model of Pseudomonas aeruginosa sinusitis. Transl. Res. J. Lab. Clin. Med. 2019, 206, 41–56. [Google Scholar] [CrossRef] [PubMed]
- Lebeaux, D.; Merabishvili, M.; Caudron, E.; Lannoy, D.; Van Simaey, L.; Duyvejonck, H.; Guillemain, R.; Thumerelle, C.; Podglajen, I.; Compain, F.; et al. A Case of Phage Therapy against Pandrug-Resistant Achromobacter xylosoxidans in a 12-Year-Old Lung-Transplanted Cystic Fibrosis Patient. Viruses 2021, 13, 60. [Google Scholar] [CrossRef]
- Yin, S.; Huang, G.; Zhang, Y.; Jiang, B.; Yang, Z.; Dong, Z.; You, B.; Yuan, Z.; Hu, F.; Zhao, Y.; et al. Phage Abp1 Rescues Human Cells and Mice from Infection by Pan-Drug Resistant Acinetobacter Baumannii. Cell. Physiol. Biochem. 2017, 44, 2337–2345. [Google Scholar] [CrossRef]
- Dedrick, R.M.; Guerrero-Bustamante, C.A.; Garlena, R.A.; Russell, D.A.; Ford, K.; Harris, K.; Gilmour, K.C.; Soothill, J.; Jacobs-Sera, D.; Schooley, R.T.; et al. Engineered bacteriophages for treatment of a patient with a disseminated drug resistant Mycobacterium abscessus. Nat. Med. 2019, 25, 730–733. [Google Scholar] [CrossRef]
- Doub, J.B.; Ng, V.Y.; Johnson, A.J.; Slomka, M.; Fackler, J.; Horne, B.; Brownstein, M.J.; Henry, M.; Malagon, F.; Biswas, B. Salvage Bacteriophage Therapy for a Chronic MRSA Prosthetic Joint Infection. Antibiotics 2020, 9, 241. [Google Scholar] [CrossRef]
- LaVergne, S.; Hamilton, T.; Biswas, B.; Kumaraswamy, M.; Schooley, R.T.; Wooten, D. Phage Therapy for a Multidrug-Resistant Acinetobacter baumannii Craniectomy Site Infection. Open Forum Infect. Dis. 2018, 5, ofy064. [Google Scholar] [CrossRef] [PubMed]
- Lindford, A.; Kiuru, V.; Anttila, V.J.; Vuola, J. Successful eradication of multidrug resistant acinetobacter in the Helsinki burn centre. J. Burn. Care Res. 2015, 36, 595–601. [Google Scholar] [CrossRef]
- Karumathil, D.P.; Nair, M.S.; Gaffney, J.; Kollanoor-Johny, A.; Venkitanarayanan, K. Trans-Cinnamaldehyde and eugenol increase Acinetobacter baumannii sensitivity to beta-lactam antibiotics. Front. Microbiol. 2018, 9, 1011. [Google Scholar] [CrossRef] [PubMed]
- Tsuji, B.T.; Pogue, J.M.; Zavascki, A.P.; Paul, M.; Daikos, G.L.; Forrest, A.; Giacobbe, D.R.; Viscoli, C.; Giamarellou, H.; Karaiskos, I.; et al. International Consensus Guidelines for the Optimal Use of the Polymyxins: Endorsed by the American College of Clinical Pharmacy (ACCP), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), and Society of Infectious Diseases Pharmacists (SIDP). Pharmacother. J. Hum. Pharmacol. Drug Ther. 2019, 39, 10–39. [Google Scholar] [CrossRef]
- Yang, Z.; Shi, Y.; Zhang, C.; Luo, X.; Chen, Y.; Peng, Y.; Gong, Y. Lytic Bacteriophage Screening Strategies for Multidrug-Resistant Bloodstream Infections in a Burn Intensive Care Unit. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019, 25, 8352–8362. [Google Scholar] [CrossRef]
- WHO Publishes List of Bacteria for Which New Antibiotics Are Urgently Needed; World Health Organization: Geneva, Switzerland, 2017. Available online: https://www.who.int/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed (accessed on 8 January 2023).
- Hendrix, R.W.; Smith, M.C.M.; Burns, R.N.; Ford, M.E.; Hatfull, G.F. Evolutionary relationships among diverse bacteriophages and prophages: All the world’s a phage. Proc. Natl. Acad. Sci. USA 1999, 96, 2192–2197. [Google Scholar] [CrossRef]
- Kim, S.H.; Adeyemi, D.E.; Park, M.K. Characterization of a new and efficient polyvalent phage infecting E. coli o157:H7, Salmonella spp., and Shigella sonnei. Microorganisms 2021, 9, 2105. [Google Scholar] [CrossRef]
- Hudson, J.A.; Billington, C.; Wilson, T.; On, S.L.W. Effect of phage and host concentration on the inactivation of Escherichia coli O157:H7 on cooked and raw beef. Food Sci. Technol. Int. = Cienc. Y Tecnol. De Los Aliment. Int. 2015, 21, 104–109. [Google Scholar] [CrossRef]
- Duc, H.M.; Son, H.M.; Yi, H.P.S.; Sato, J.; Ngan, P.H.; Masuda, Y.; Honjoh, K.; Miyamoto, T. Isolation, characterization and application of a polyvalent phage capable of controlling Salmonella and Escherichia coli O157:H7 in different food matrices. Food Res. Int. 2020, 131, 108977. [Google Scholar] [CrossRef]
- Sui, B.; Han, L.; Ren, H.; Liu, W.; Zhang, C. A Novel Polyvalent Bacteriophage vB_EcoM_swi3 Infects Pathogenic Escherichia coli and Salmonella enteritidis. Front. Microbiol. 2021, 12, 649673. [Google Scholar] [CrossRef]
- Sieiro, C.; Areal-Hermida, L.; Pichardo-Gallardo, Á.; Almuiña-González, R.; De Miguel, T.; Sánchez, S.; Sánchez-Pérez, Á.; Villa, T.G. A Hundred Years of Bacteriophages: Can Phages Replace Antibiotics in Agriculture and Aquaculture? Antibiotics 2020, 9, 493. [Google Scholar] [CrossRef] [PubMed]
- d’Herelle, F. An Address on Bacteriophagy and Recovery from Infectious Diseases. Can. Med. Assoc. J. 1931, 24, 619–628. [Google Scholar]
- d’Herelle, F. Annual Graduate Fortnight. Medical and Surgical Aspects of Acute Bacterial Infections, October 20 to 31, 1930: Bacteriophage as a Treatment in Acute Medical and Surgical Infections. Bull. N. Y. Acad. Med. 1931, 7, 329–348. [Google Scholar] [PubMed]
- Pirnay, J.P.; De Vos, D.; Verbeken, G.; Merabishvili, M.; Chanishvili, N.; Vaneechoutte, M.; Zizi, M.; Laire, G.; Lavigne, R.; Huys, I.; et al. The phage therapy paradigm: Prêt-à-porter or sur-mesure? Pharm. Res. 2011, 28, 934–937. [Google Scholar] [CrossRef] [PubMed]
- Arumugam, S.N.; Rudraradhya, A.C.; Sadagopan, S.; Sukumaran, S.; Sambasivam, G.; Ramesh, N. Analysis of susceptibility patterns of pseudomonas aeruginosa and Isolation, Characterization of lytic bacteriophages targeting multi drug resistant Pseudomonas aeruginosa. Biomed. Pharmacol. J. 2018, 11, 1105–1117. [Google Scholar] [CrossRef]
- Nepal, R.; Houtak, G.; Karki, S.; Dhungana, G.; Vreugde, S.; Malla, R. Genomic characterization of three bacteriophages targeting multidrug resistant clinical isolates of Escherichia, Klebsiella and Salmonella. Arch. Microbiol. 2022, 204, 334. [Google Scholar] [CrossRef]
- Tao, C.; Yi, Z.; Zhang, Y.; Wang, Y.; Zhu, H.; Afayibo, D.J.A.; Li, T.; Tian, M.; Qi, J.; Ding, C.; et al. Characterization of a Broad-Host-Range Lytic Phage SHWT1 Against Multidrug-Resistant Salmonella and Evaluation of Its Therapeutic Efficacy in vitro and in vivo. Front. Vet. Sci. 2021, 8, 683853. [Google Scholar] [CrossRef]
- Deng, L.Y.; Yang, Z.C.; Gong, Y.L.; Huang, G.T.; Yin, S.P.; Jiang, B.; Peng, Y.Z. Therapeutic effect of phages on extensively drug-resistant Acinetobacter baumannii-induced sepsis in mice. Chin. J. Burn. 2016, 32, 523–528. [Google Scholar] [CrossRef]
- Schooley, R.T.; Biswas, B.; Gill, J.J.; Hernandez-Morales, A.; Lancaster, J.; Lessor, L.; Barr, J.J.; Reed, S.L.; Rohwer, F.; Benler, S.; et al. Development and Use of Personalized Bacteriophage-Based Therapeutic Cocktails to Treat a Patient with a Disseminated Resistant Acinetobacter baumannii Infection. Antimicrob. Agents Chemother. 2017, 61, e00954-17. [Google Scholar] [CrossRef]
- Aslam, S.; Courtwright, A.M.; Koval, C.; Lehman, S.M.; Morales, S.; Furr, C.L.L.; Rosas, F.; Brownstein, M.J.; Fackler, J.R.; Sisson, B.M.; et al. Early clinical experience of bacteriophage therapy in 3 lung transplant recipients. Am. J. Transplantation 2019, 19, 2631–2639. [Google Scholar] [CrossRef]
- Rubalskii, E.; Ruemke, S.; Salmoukas, C.; Boyle, E.C.; Warnecke, G.; Tudorache, I.; Shrestha, M.; Schmitto, J.D.; Martens, A.; Rojas, S.V.; et al. Bacteriophage Therapy for Critical Infections Related to Cardiothoracic Surgery. Antibiotics 2020, 9, 232. [Google Scholar] [CrossRef]
- Wu, N.; Dai, J.; Guo, M.; Li, J.; Zhou, X.; Li, F.; Gao, Y.; Qu, H.; Lu, H.; Jin, J.; et al. Pre-optimized phage therapy on secondary Acinetobacter baumannii infection in four critical COVID-19 patients. Emerg. Microbes Infect. 2021, 10, 612–618. [Google Scholar] [CrossRef] [PubMed]
- Nick, J.A.; Dedrick, R.M.; Gray, A.L.; Vladar, E.K.; Smith, B.E.; Freeman, K.G.; Malcolm, K.C.; Epperson, L.E.; Hasan, N.A.; Hendrix, J.; et al. Host and pathogen response to bacteriophage engineered against Mycobacterium abscessus lung infection. Cell 2022, 185, 1860–1874.e12. [Google Scholar] [CrossRef] [PubMed]
- Martin, M.J.; Thottathil, S.E.; Newman, T.B. Antibiotics overuse in animal agriculture: A call to action for health care providers. Am. J. Public Health 2015, 105, 2409–2410. [Google Scholar] [CrossRef] [PubMed]
- Muloi, D.; Ward, M.J.; Pedersen, A.B.; Fèvre, E.M.; Woolhouse, M.E.J.; Van Bunnik, B.A.D. Are Food Animals Responsible for Transfer of Antimicrobial-Resistant Escherichia coli or Their Resistance Determinants to Human Populations? A Systematic Review. Foodborne Pathog. Dis. 2018, 15, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, H.; Zolfo, M.; Williams, A.; Ashubwe-Jalemba, J.; Tweya, H.; Adeapena, W.; Labi, A.; Adomako, L.A.B.; Addico, G.N.D.; Banu, R.A.; et al. Antibiotic-Resistant Bacteria in Drinking Water from the Greater Accra Region, Ghana: A Cross-Sectional Study, December 2021–March 2022. Int. J. Environ. Res. Public Health 2022, 19, 12300. [Google Scholar] [CrossRef] [PubMed]
- Bamigboye, C.O.; Amao, J.A.; Ayodele, T.A.; Adebayo, A.S.; Ogunleke, J.D.; Abass, T.B.; Oyedare, T.A.; Adetutu, T.J.; Adeeyo, A.O.; Oyedemi, A.A. An appraisal of the drinking water quality of groundwater sources in Ogbomoso, Oyo state, Nigeria. Groundw. Sustain. Dev. 2020, 11, 100453. [Google Scholar] [CrossRef]
- Odonkor, S.T.; Simpson, S.V.; Morales Medina, W.R.; Fahrenfeld, N.L. Antibiotic-Resistant Bacteria and Resistance Genes in Isolates from Ghanaian Drinking Water Sources. J. Environ. Public Health 2022, 2022, 2850165. [Google Scholar] [CrossRef]
- Adesoji, A.T.; Onuh, J.P.; Musa, A.O.; Akinrosoye, P.F. Bacteriological qualities and antibiogram studies of bacteria from “suya” and smoked fish (Clarias gariepinus) in Dutsin-Ma, Katsina State, Nigeria. Pan Afr. Med. J. 2019, 33, 219. [Google Scholar] [CrossRef]
- Lauteri, C.; Festino, A.R.; Conter, M.; Vergara, A. Prevalence and antimicrobial resistance profile in Salmonella spp. isolates from swine food chain. Ital. J. Food Saf. 2022, 11, 9980. [Google Scholar] [CrossRef]
- Rau, R.B.; Ribeiro, A.R.; Dos Santos, A.; Barth, A.L. Antimicrobial resistance of Salmonella from poultry meat in Brazil: Results of a nationwide survey. Epidemiol. Infect. 2021, 149, 26–39. [Google Scholar] [CrossRef]
- Andreoletti, O.; Lau Baggesen, D.; Bolton, D.; Butaye, P.; Cook, P.; Davies, R.; Escámez, P.S.F.; Griffin, J.; Hald, T.; Havelaar, A.; et al. Scientific Opinion on the risk posed by pathogens in food of non-animal origin. Part 1 (outbreak data analysis and risk ranking of food/pathogen combinations). EFSA J. 2013, 11, 3025. [Google Scholar] [CrossRef]
- Rahman, M.; Alam, M.U.; Luies, S.K.; Kamal, A.; Ferdous, S.; Lin, A.; Sharior, F.; Khan, R.; Rahman, Z.; Parvez, S.M.; et al. Contamination of fresh produce with antibiotic-resistant bacteria and associated risks to human health: A scoping review. Int. J. Environ. Res. Public Health 2022, 19, 360. [Google Scholar] [CrossRef] [PubMed]
- Verma, P.; Saharan, V.V.; Nimesh, S.; Singh, A.P. Phenotypic and virulence traits of Escherichia coli and Salmonella strains isolated from vegetables and fruits from India. J. Appl. Microbiol. 2018, 125, 270–281. [Google Scholar] [CrossRef]
- Olowe, O.A.; Adefioye, O.J.; Ajayeoba, T.A.; Schiebel, J.; Weinreich, J.; Ali, A.; Burdukiewicz, M.; Rödiger, S.; Schierack, P. Phylogenetic grouping and biofilm formation of multidrug resistant Escherichia coli isolates from humans, animals and food products in South-West Nigeria. Sci. Afr. 2019, 6, e00158. [Google Scholar] [CrossRef]
- Naghizadeh, M.; Karimi Torshizi, M.A.; Rahimi, S.; Engberg, R.M.; Sørensen Dalgaard, T. Effect of serum anti-phage activity on colibacillosis control by repeated phage therapy in broilers. Vet. Microbiol. 2019, 234, 61–71. [Google Scholar] [CrossRef]
- Guo, M.; Gao, Y.; Xue, Y.; Liu, Y.; Zeng, X.; Cheng, Y.; Ma, J.; Wang, H.; Sun, J.; Wang, Z.; et al. Bacteriophage Cocktails Protect Dairy Cows Against Mastitis Caused By Drug Resistant Escherichia coli Infection. Front. Cell. Infect. Microbiol. 2021, 11, 690377. [Google Scholar] [CrossRef]
- Tolen, T.N.; Xie, Y.; Hairgrove, T.B.; Gill, J.J.; Matthew Taylor, T. Evaluation of commercial prototype bacteriophage intervention designed for reducing O157 and non-O157 Shiga-toxigenic Escherichia coli (STEC) on beef cattle hide. Foods 2018, 7, 114. [Google Scholar] [CrossRef]
- Verstappen, K.M.; Tulinski, P.; Duim, B.; Fluit, A.C.; Carney, J.; Van Nes, A.; Wagenaar, J.A. The Effectiveness of Bacteriophages against Methicillin-Resistant Staphylococcus aureus ST398 Nasal Colonization in Pigs. PLoS ONE 2016, 11, e0160242. [Google Scholar] [CrossRef]
- Thanki, A.M.; Brown, N.; Millard, A.D.; Clokie, M.R.J. Genomic characterization of jumbo Salmonella phages that effectively target United Kingdom pig-associated Salmonella serotypes. Front. Microbiol. 2019, 10, 1491. [Google Scholar] [CrossRef]
- Chen, L.; Fan, J.; Yan, T.; Liu, Q.; Yuan, S.; Zhang, H.; Yang, J.; Deng, D.; Huang, S.; Ma, Y. Isolation and Characterization of Specific Phages to Prepare a Cocktail Preventing Vibrio sp. Va-F3 Infections in Shrimp (Litopenaeus vannamei). Front. Microbiol. 2019, 10, 2337. [Google Scholar] [CrossRef] [PubMed]
- Le, T.S.; Southgate, P.C.; O’connor, W.; Vu, S.V.; İpek Kurtböke, D. Application of Bacteriophages to Control Vibrio alginolyticus Contamination in Oyster (Saccostrea glomerata) Larvae. Antibiotics 2020, 9, 415. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Wei, Z.; Yang, K.; Wang, J.; Jousset, A.; Xu, Y.; Shen, Q.; Friman, V.P. Phage combination therapies for bacterial wilt disease in tomato. Nat. Biotechnol. 2019, 37, 1513–1520. [Google Scholar] [CrossRef] [PubMed]
- Carstens, A.B.; Djurhuus, A.M.; Kot, W.; Hansen, L.H. A novel six-phage cocktail reduces Pectobacterium atrosepticum soft rot infection in potato tubers under simulated storage conditions. FEMS Microbiol. Lett. 2019, 366, fnz101. [Google Scholar] [CrossRef] [PubMed]
- Zaczek-Moczydłowska, M.A.; Young, G.K.; Trudgett, J.; Plahe, C.; Fleming, C.C.; Campbell, K.; O’Hanlon, R. Phage cocktail containing Podoviridae and Myoviridae bacteriophages inhibits the growth of Pectobacterium spp. under in vitro and in vivo conditions. PLoS ONE 2020, 15, e0230842. [Google Scholar] [CrossRef] [PubMed]
- Papaianni, M.; Paris, D.; Woo, S.L.; Fulgione, A.; Rigano, M.M.; Parrilli, E.; Tutino, M.L.; Marra, R.; Manganiello, G.; Casillo, A.; et al. Plant Dynamic Metabolic Response to Bacteriophage Treatment After Xanthomonas campestris pv. campestris Infection. Front. Microbiol. 2020, 11, 732. [Google Scholar] [CrossRef]
- Vikram, A.; Tokman, J.I.; Woolston, J.; Sulakvelidze, A. Phage Biocontrol Improves Food Safety by Significantly Reducing the Level and Prevalence of Escherichia coli O157:H7 in Various Foods. J. Food Prot. 2020, 83, 668–676. [Google Scholar] [CrossRef]
- Xu, J.; Zhang, R.; Yu, X.; Zhang, X.; Liu, G.; Liu, X. Molecular Characteristics of Novel Phage vB_ShiP-A7 Infecting Multidrug-Resistant Shigella flexneri and Escherichia coli, and Its Bactericidal Effect in vitro and in vivo. Front. Microbiol. 2021, 12, 698962. [Google Scholar] [CrossRef]
- Rangasamy, K.; Murugan, A.; Devarajan, N.; Parray, J.A. Emergence of multi drug resistance among soil bacteria exposing to insecticides. Microb. Pathog. 2017, 105, 153–165. [Google Scholar] [CrossRef]
- Mahdiyah, D.; Farida, H.; Riwanto, I.; Mustofa, M.; Wahjono, H.; Laksana Nugroho, T.; Reki, W. Screening of Indonesian peat soil bacteria producing antimicrobial compounds. Saudi J. Biol. Sci. 2020, 27, 2604–2611. [Google Scholar] [CrossRef]
- Mafiz, A.I.; He, Y.; Zhang, W.; Zhang, Y. Soil Bacteria in Urban Community Gardens Have the Potential to Disseminate Antimicrobial Resistance Through Horizontal Gene Transfer. Front. Microbiol. 2021, 12, 771707. [Google Scholar] [CrossRef]
- Yahya, M.; Hmaied, F.; Jebri, S.; Jofre, J.; Hamdi, M. Bacteriophages as indicators of human and animal faecal contamination in raw and treated wastewaters from Tunisia. J. Appl. Microbiol. 2015, 118, 1217–1225. [Google Scholar] [CrossRef]
- Calero-Cáceres, W.; Balcázar, J.L. Antibiotic resistance genes in bacteriophages from diverse marine habitats. Sci. Total Environ. 2019, 654, 452–455. [Google Scholar] [CrossRef] [PubMed]
- Lekunberri, I.; Subirats, J.; Borrego, C.M.; Balcázar, J.L. Exploring the contribution of bacteriophages to antibiotic resistance. Environ. Pollut. 2017, 220, 981–984. [Google Scholar] [CrossRef] [PubMed]
- Loc-Carrillo, C.; Abedon, S.T. Pros and cons of phage therapy. Bacteriophage 2011, 1, 111–114. [Google Scholar] [CrossRef] [PubMed]
- McCallin, S.; Alam Sarker, S.; Barretto, C.; Sultana, S.; Berger, B.; Huq, S.; Krause, L.; Bibiloni, R.; Schmitt, B.; Reuteler, G.; et al. Safety analysis of a Russian phage cocktail: From MetaGenomic analysis to oral application in healthy human subjects. Virology 2013, 443, 187–196. [Google Scholar] [CrossRef]
- Febvre, H.P.; Rao, S.; Gindin, M.; Goodwin, N.D.M.; Finer, E.; Vivanco, J.S.; Manter, D.K.; Wallace, T.C.; Weir, T.L. PHAGE study: Effects of supplemental bacteriophage intake on inflammation and gut microbiota in healthy adults. Nutrients 2019, 11, 666. [Google Scholar] [CrossRef]
- Galtier, M.; De Sordi, L.; Maura, D.; Arachchi, H.; Volant, S.; Dillies, M.A.; Debarbieux, L. Bacteriophages to reduce gut carriage of antibiotic resistant uropathogens with low impact on microbiota composition. Environ. Microbiol. 2016, 18, 2237–2245. [Google Scholar] [CrossRef]
- Grubb, D.S.; Wrigley, S.D.; Freedman, K.E.; Wei, Y.; Vazquez, A.R.; Trotter, R.E.; Wallace, T.C.; Johnson, S.A.; Weir, T.L. PHAGE-2 Study: Supplemental Bacteriophages Extend Bifidobacterium animalis subsp. lactis BL04 Benefits on Gut Health and Microbiota in Healthy Adults. Nutrients 2020, 12, 2474. [Google Scholar] [CrossRef]
- Gunathilaka, G.U.; Tahlan, V.; Mafiz, A.I.; Polur, M.; Zhang, Y. Phages in urban wastewater have the potential to disseminate antibiotic resistance. Int. J. Antimicrob. Agents 2017, 50, 678–683. [Google Scholar] [CrossRef]
- Liu, J.; Liu, P.; Feng, F.; Zhang, J.; Li, F.; Wang, M.; Sun, Y. Evaluation of Potential ARG Packaging by Two Environmental T7-Like Phage during Phage-Host Interaction. Viruses 2020, 12, 1060. [Google Scholar] [CrossRef]
- Zhang, Y.; Guo, Y.; Qiu, T.; Gao, M.; Wang, X. Bacteriophages: Underestimated vehicles of antibiotic resistance genes in the soil. Front. Microbiol. 2022, 13, 936267. [Google Scholar] [CrossRef]
- Frazão, N.; Sousa, A.; Lässig, M.; Gordo, I. Horizontal gene transfer overrides mutation in Escherichia coli colonizing the mammalian gut. Proc. Natl. Acad. Sci. USA 2019, 116, 17906–17915. [Google Scholar] [CrossRef]
- Fernández-Orth, D.; Miró, E.; Brown-Jaque, M.; Rodríguez-Rubio, L.; Espinal, P.; Rodriguez-Navarro, J.; González-López, J.J.; Muniesa, M.; Navarro, F. Faecal phageome of healthy individuals: Presence of antibiotic resistance genes and variations caused by ciprofloxacin treatment. J. Antimicrob. Chemother. 2019, 74, 854–864. [Google Scholar] [CrossRef]
- Enault, F.; Briet, A.; Bouteille, L.; Roux, S.; Sullivan, M.B.; Petit, M.A. Phages rarely encode antibiotic resistance genes: A cautionary tale for virome analyses. ISME J. 2016, 11, 237–247. [Google Scholar] [CrossRef]
- Chan, B.K.; Abedon, S.T.; Loc-Carrillo, C. Phage cocktails and the future of phage therapy. Future Microbiol. 2013, 8, 769–783. [Google Scholar] [CrossRef]
- Ujmajuridze, A.; Chanishvili, N.; Goderdzishvili, M.; Leitner, L.; Mehnert, U.; Chkhotua, A.; Kessler, T.M.; Sybesma, W. Adapted bacteriophages for treating urinary tract infections. Front. Microbiol. 2018, 9, 1832. [Google Scholar] [CrossRef]
- Infusion Related Reactions Guidance 2013; Canterbury District Health Board (CRCHS): Canterbury, New Zealand, 2013; Available online: https://edu.cdhb.health.nz/Hospitals-Services/health-professionals/Cytotoxic-Biotherapy/Documents/Infusion%20Related%20Reactions%20Guidance%202013.pdf (accessed on 12 April 2023).
- Moghadam, M.T.; Amirmozafari, N.; Shariati, A.; Hallajzadeh, M.; Mirkalantari, S.; Khoshbayan, A.; Jazi, F.M. How phages overcome the challenges of drug resistant bacteria in clinical infections. Infect. Drug Resist. 2020, 13, 45–61. [Google Scholar] [CrossRef]
- Van Belleghem, J.D.; Clement, F.; Merabishvili, M.; Lavigne, R.; Vaneechoutte, M. Pro- and anti-inflammatory responses of peripheral blood mononuclear cells induced by Staphylococcus aureus and Pseudomonas aeruginosa phages. Sci. Rep. 2017, 7, 8004. [Google Scholar] [CrossRef]
- Zhang, L.; Hou, X.; Sun, L.; He, T.; Wei, R.; Pang, M.; Wang, R. Corrigendum: Staphylococcus aureus Bacteriophage Suppresses LPS-Induced Inflammation in MAC-T Bovine Mammary Epithelial Cells. Front. Microbiol. 2018, 9, 331–333. [Google Scholar] [CrossRef]
- Dufour, N.; Delattre, R.; Chevallereau, A.; Ricard, J.D.; Debarbieux, L. Phage Therapy of Pneumonia Is Not Associated with an Overstimulation of the Inflammatory Response Compared to Antibiotic Treatment in Mice. Antimicrob. Agents Chemother. 2019, 63, e00379-19. [Google Scholar] [CrossRef]
- Majewska, J.; Kaźmierczak, Z.; Lahutta, K.; Lecion, D.; Szymczak, A.; Miernikiewicz, P.; Drapała, J.; Harhala, M.; Marek-Bukowiec, K.; Jędruchniewicz, N.; et al. Induction of Phage-Specific Antibodies by Two Therapeutic Staphylococcal bacteriophages Administered per os. Front. Immunol. 2019, 10, 2607. [Google Scholar] [CrossRef]
- Jun, J.W.; Shin, T.H.; Kim, J.H.; Shin, S.P.; Han, J.E.; Heo, G.J.; De Zoysa, M.; Shin, G.W.; Chai, J.Y.; Park, S.C. Bacteriophage Therapy of a Vibrio parahaemolyticus Infection Caused by a Multiple-Antibiotic–Resistant O3:K6 Pandemic Clinical Strain. J. Infect. Dis. 2014, 210, 72–78. [Google Scholar] [CrossRef]
- Sunagar, R.; Patil, S.A.; Chandrakanth, R.K. Bacteriophage therapy for Staphylococcus aureus bacteremia in streptozotocin-induced diabetic mice. Res. Microbiol. 2010, 161, 854–860. [Google Scholar] [CrossRef]
- Gainey, A.B.; Burch, A.K.; Brownstein, M.J.; Brown, D.E.; Fackler, J.; Horne, B.; Biswas, B.; Bivens, B.N.; Malagon, F.; Daniels, R. Combining bacteriophages with cefiderocol and meropenem/vaborbactam to treat a pan-drug resistant Achromobacter species infection in a pediatric cystic fibrosis patient. Pediatr. Pulmonol. 2020, 55, 2990–2994. [Google Scholar] [CrossRef]
- Moghadam, M.T.; Khoshbayan, A.; Chegini, Z.; Farahani, I.; Shariati, A. Bacteriophages, a New Therapeutic Solution for Inhibiting Multidrug-Resistant Bacteria Causing Wound Infection: Lesson from Animal Models and Clinical Trials. Drug Des. Dev. Ther. 2020, 14, 1867–1883. [Google Scholar] [CrossRef]
- Park, K.; Cha, K.E.; Myung, H. Observation of inflammatory responses in mice orally fed with bacteriophage T7. J. Appl. Microbiol. 2014, 117, 627–633. [Google Scholar] [CrossRef]
- Setting Endotoxin Acceptance Criteria for Biologics Intravenous (IV) and Subcutaneous (SC) Mono- and Combination Therapies| American Pharmaceutical Review—The Review of American Pharmaceutical Business & Technology. American Pharmaceutical Review. 2018. Available online: https://www.americanpharmaceuticalreview.com/Featured-Articles/353671-Setting-Endotoxin-Acceptance-Criteria-for-Biologics-Intravenous-IV-and-Subcutaneous-SC-Mono-and-Combination-Therapies/ (accessed on 27 April 2023).
- Cooper, C.J.; Mirzaei, M.K.; Nilsson, A.S. Adapting drug approval pathways for bacteriophage-based therapeutics. Front. Microbiol. 2016, 7, 1209. [Google Scholar] [CrossRef]
- Bao, H.; Zhang, H.; Zhou, Y.; Zhu, S.; Pang, M.; Shahin, K.; Shahin, K.; Olaniran, A.; Schmidt, S.; Wang, R. Transient carriage and low-level colonization of orally administrated lytic and temperate phages in the gut of mice. Food Prod. Process. Nutr. 2020, 2, 14. [Google Scholar] [CrossRef]
- Cano, E.J.; Caflisch, K.M.; Bollyky, P.L.; Van Belleghem, J.D.; Patel, R.; Fackler, J.; Brownstein, M.J.; Horne, B.; Biswas, B.; Henry, M.; et al. Phage Therapy for Limb-threatening Prosthetic Knee Klebsiella pneumoniae Infection: Case Report and In Vitro Characterization of Anti-biofilm Activity. Clin. Infect. Dis. 2021, 73, e144–e151. [Google Scholar] [CrossRef]
- Jault, P.; Leclerc, T.; Jennes, S.; Pirnay, J.P.; Que, Y.A.; Resch, G.; Rousseau, A.F.; Ravat, F.; Carsin, H.; Le Floch, R.; et al. Efficacy and tolerability of a cocktail of bacteriophages to treat burn wounds infected by Pseudomonas aeruginosa (PhagoBurn): A randomised, controlled, double-blind phase 1/2 trial. Lancet Infect. Dis. 2019, 19, 35–45. [Google Scholar] [CrossRef]
- Wang, Y.; Han, S. Bacterial DNA involvement in carcinogenesis. Front. Cell. Infect. Microbiol. 2022, 12, 996778. [Google Scholar] [CrossRef]
- Gilbey, T.; Ho, J.; Cooley, L.A.; Petrovic Fabijan, A.; Iredell, J.R. Adjunctive bacteriophage therapy for prosthetic valve endocarditis due to Staphylococcus aureus. Med. J. Aust. 2019, 211, 142–143.e1. [Google Scholar] [CrossRef] [PubMed]
- Janik, E.; Ceremuga, M.; Bijak, J.S.; Bijak, M. Biological Toxins as the Potential Tools for Bioterrorism. Int. J. Mol. Sci. 2019, 20, 1181. [Google Scholar] [CrossRef] [PubMed]
- Kissner, T.L.; Cisney, E.D.; Ulrich, R.G.; Fernandez, S.; Saikh, K.U. Staphylococcal enterotoxin A induction of pro-inflammatory cytokines and lethality in mice is primarily dependent on MyD88. Immunology 2010, 130, 516–526. [Google Scholar] [CrossRef]
- Otto, M. Staphylococcus aureus toxins. Curr. Opin. Microbiol. 2014, 17, 32–37. [Google Scholar] [CrossRef]
- Ho, S.S.; Michalek, S.M.; Nahm, M.H. Lipoteichoic Acid Is Important in Innate Immune Responses to Gram-Positive Bacteria. Infect. Immun. 2008, 76, 206–213. [Google Scholar] [CrossRef]
- Berube, B.J.; Wardenburg, J.B. Staphylococcus aureus α-Toxin: Nearly a Century of Intrigue. Toxins 2013, 5, 1140–1166. [Google Scholar] [CrossRef]
- Szentirmai, É.; Massie, A.R.; Kapás, L. Lipoteichoic acid, a cell wall component of Gram-positive bacteria, induces sleep and fever and suppresses feeding. Brain Behav. Immun. 2021, 92, 184–192. [Google Scholar] [CrossRef]
- Guerin, K.; Choi, V.; Aranda, J.; Demirs, J.; Li, H.; Yang, J.; Nguyen, N.; Bottega, S.; Jaffee, B.; Dryja, T.; et al. Residual Cesium Chloride in AAV Vectors Purified by CsCl Gradient Centrifugation Does Not Cause Obvious Inflammation or Retinal Degeneration in C57Bl6/J Mice Following Subretinal Injection. Mol. Ther. 2015, 23, S240. [Google Scholar] [CrossRef]
- Hietala, V.; Horsma-Heikkinen, J.; Carron, A.; Skurnik, M.; Kiljunen, S. The Removal of Endo- and Enterotoxins from Bacteriophage Preparations. Front. Microbiol. 2019, 10, 1674. [Google Scholar] [CrossRef]
- Chaudhary, K. BacteRiophage EXclusion (BREX): A novel anti-phage mechanism in the arsenal of bacterial defense system. J. Cell. Physiol. 2018, 233, 771–773. [Google Scholar] [CrossRef]
- Liu, M.; Deora, R.; Doulatov, S.R.; Gingery, M.; Eiserling, F.A.; Preston, A.; Maskell, D.J.; Simons, R.W.; Cotter, P.A.; Parkhill, J.; et al. Reverse transcriptase-mediated tropism switching in Bordetella bacteriophage. Science 2002, 295, 2091–2094. [Google Scholar] [CrossRef] [PubMed]
- Fineran, P.C.; Blower, T.R.; Foulds, I.J.; Humphreys, D.P.; Lilley, K.S.; Salmond, G.P.C. The phage abortive infection system, ToxIN, functions as a protein-RNA toxin-antitoxin pair. Proc. Natl. Acad. Sci. USA 2009, 106, 894–899. [Google Scholar] [CrossRef] [PubMed]
- Blower, T.R.; Fineran, P.C.; Johnson, M.J.; Toth, I.K.; Humphreys, D.P.; Salmond, G.P.C. Mutagenesis and functional characterization of the RNA and protein components of the toxIN abortive infection and toxin-antitoxin locus of Erwinia. J. Bacteriol. 2009, 191, 6029–6039. [Google Scholar] [CrossRef] [PubMed]
- Larsson, D.G.J. Antibiotics in the environment. Upsala J. Med. Sci. 2014, 119, 108–112. [Google Scholar] [CrossRef]
- Litt, P.K.; Jaroni, D. Isolation and Physiomorphological Characterization of Escherichia coli O157:H7-Infecting Bacteriophages Recovered from Beef Cattle Operations. Int. J. Microbiol. 2017, 2017, 7013236. [Google Scholar] [CrossRef]
- Meaden, S.; Koskella, B. Exploring the risks of phage application in the environment. Front. Microbiol. 2013, 4, 358. [Google Scholar] [CrossRef]
- Drilling, A.J.; Ooi, M.L.; Miljkovic, D.; James, C.; Speck, P.; Vreugde, S.; Clark, J.; Wormald, P.J. Long-Term Safety of Topical Bacteriophage Application to the Frontal Sinus Region. Front. Cell. Infect. Microbiol. 2017, 7, 49. [Google Scholar] [CrossRef]
- Liu, D.; Van Belleghem, J.D.; de Vries, C.R.; Burgener, E.; Chen, Q.; Manasherob, R.; Aronson, J.R.; Amanatullah, D.F.; Tamma, P.D.; Suh, G.A. The safety and toxicity of phage therapy: A review of animal and clinical studies. Viruses 2021, 13, 1268. [Google Scholar] [CrossRef]
- Onsea, J.; Soentjens, P.; Djebara, S.; Merabishvili, M.; Depypere, M.; Spriet, I.; De Munter, P.; Debaveye, Y.; Njis, S.; Vanderschot, P.; et al. Bacteriophage Application for Difficult-To-Treat Musculoskeletal Infections: Development of a Standardized Multidisciplinary Treatment Protocol. Viruses 2019, 11, 891. [Google Scholar] [CrossRef] [PubMed]
- Khatami, A.; Lin, R.C.Y.; Petrovic-Fabijan, A.; Alkalay-Oren, S.; Almuzam, S.; Britton, P.N.; Brownstein, M.J.; Dao, Q.; Fackler, J.; Hazan, R.; et al. Bacterial lysis, autophagy and innate immune responses during adjunctive phage therapy in a child. EMBO Mol. Med. 2021, 13, e13936. [Google Scholar] [CrossRef] [PubMed]
- Aslam, S.; Lampley, E.; Wooten, D.; Karris, M.; Benson, C.; Strathdee, S.; Schooley, R.T. Lessons Learned From the First 10 Consecutive Cases of Intravenous Bacteriophage Therapy to Treat Multidrug-Resistant Bacterial Infections at a Single Center in the United States. Open Forum Infect. Dis. 2020, 7, ofaa389. [Google Scholar] [CrossRef] [PubMed]
- Bao, J.; Wu, N.; Zeng, Y.; Chen, L.; Li, L.; Yang, L.; Zhang, Y.; Guo, M.; Li, L.; Li, J.; et al. Non-active antibiotic and bacteriophage synergism to successfully treat recurrent urinary tract infection caused by extensively drug-resistant Klebsiella pneumoniae. Emerg. Microbes Infect. 2020, 9, 771–774. [Google Scholar] [CrossRef] [PubMed]
- Eskenazi, A.; Lood, C.; Wubbolts, J.; Hites, M.; Balarjishvili, N.; Leshkasheli, L.; Askilashvili, L.; Kvachadze, L.; van Noort, V.; Wagemans, J.; et al. Combination of pre-adapted bacteriophage therapy and antibiotics for treatment of fracture-related infection due to pandrug-resistant Klebsiella pneumoniae. Nat. Commun. 2022, 13, 302. [Google Scholar] [CrossRef] [PubMed]
- Johri, A.V.; Johri, P.; Hoyle, N.; Pipia, L.; Nadareishvili, L.; Nizharadze, D. Case Report: Chronic Bacterial Prostatitis Treated With Phage Therapy After Multiple Failed Antibiotic Treatments. Front. Pharmacol. 2021, 12, 692614. [Google Scholar] [CrossRef]
- Ramirez-Sanchez, C.; Gonzales, F.; Buckley, M.; Biswas, B.; Henry, M.; Deschenes, M.V.; Horne, B.; Fackler, J.; Brownstein, M.J.; Schooley, R.T.; et al. Successful Treatment of Staphylococcus aureus Prosthetic Joint Infection with Bacteriophage Therapy. Viruses 2021, 13, 1182. [Google Scholar] [CrossRef]
- Rostkowska, O.M.; Międzybrodzki, R.; Miszewska-Szyszkowska, D.; Górski, A.; Durlik, M. Treatment of recurrent urinary tract infections in a 60-year-old kidney transplant recipient. The use of phage therapy. Transpl. Infect. Dis. 2021, 23, e13391. [Google Scholar] [CrossRef]
- Corbellino, M.; Kieffer, N.; Kutateladze, M.; Balarjishvili, N.; Leshkasheli, L.; Askilashvili, L.; Tsertsvadze, G.; Rimoldi, S.G.; Nizharadze, D.; Hoyle, N.; et al. Eradication of a Multidrug-Resistant, Carbapenemase-Producing Klebsiella pneumoniae Isolate Following Oral and Intra-rectal Therapy With a Custom Made, Lytic Bacteriophage Preparation. Clin. Infect. Dis. 2020, 70, 1998–2001. [Google Scholar] [CrossRef]
- Nir-Paz, R.; Gelman, D.; Khouri, A.; Sisson, B.M.; Fackler, J.; Alkalay-Oren, S.; Khalifa, L.; Rimon, A.; Yerushalmy, O.; Bader, R.; et al. Successful Treatment of Antibiotic-resistant, Poly-microbial Bone Infection With Bacteriophages and Antibiotics Combination. Clin. Infect. Dis. 2019, 69, 2015–2018. [Google Scholar] [CrossRef]
- Tkhilaishvili, T.; Winkler, T.; Müller, M.; Perka, C.; Trampuz, A. Bacteriophages as Adjuvant to Antibiotics for the Treatment of Periprosthetic Joint Infection Caused by Multidrug-Resistant Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2020, 64, e00924-19. [Google Scholar] [CrossRef]
- Maddocks, S.; Fabijan, A.P.; Ho, J.; Lin, R.C.Y.; Ben Zakour, N.L.; Dugan, C.; Kliman, I.; Branston, S.; Morales, S.; Iredell, J.R. Bacteriophage Therapy of Ventilator-associated Pneumonia and Empyema Caused by Pseudomonas aeruginosa. Am. J. Respir. Crit. Care Med. 2019, 200, 1179–1181. [Google Scholar] [CrossRef] [PubMed]
- Law, N.; Logan, C.; Yung, G.; Furr, C.L.L.; Lehman, S.M.; Morales, S.; Rosas, F.; Gaidamaka, A.; Bilinsky, I.; Grint, P.; et al. Successful adjunctive use of bacteriophage therapy for treatment of multidrug-resistant Pseudomonas aeruginosa infection in a cystic fibrosis patient. Infection 2019, 47, 665–668. [Google Scholar] [CrossRef]
- Kuipers, S.; Ruth, M.M.; Mientjes, M.; de Sévaux, R.G.L.; van Ingen, J. A Dutch Case Report of Successful Treatment of Chronic Relapsing Urinary Tract Infection with Bacteriophages in a Renal Transplant Patient. Antimicrob. Agents Chemother. 2020, 64, e01281-19. [Google Scholar] [CrossRef] [PubMed]
- Aslam, S.; Pretorius, V.; Lehman, S.M.; Morales, S.; Schooley, R.T. Novel bacteriophage therapy for treatment of left ventricular assist device infection. J. Heart Lung Transplantation 2019, 38, 475–476. [Google Scholar] [CrossRef] [PubMed]
- Ferry, T.; Boucher, F.; Fevre, C.; Perpoint, T.; Chateau, J.; Petitjean, C.; Josse, J.; Chidiac, C.; L’hostis, G.; Leboucher, G.; et al. Innovations for the treatment of a complex bone and joint infection due to XDR Pseudomonas aeruginosa including local application of a selected cocktail of bacteriophages. J. Antimicrob. Chemother. 2018, 73, 2901–2903. [Google Scholar] [CrossRef] [PubMed]
- Duplessis, C.; Biswas, B.; Hanisch, B.; Perkins, M.; Henry, M.; Quinones, J.; Wolfe, D.; Estrella, L.; Hamilton, T. Refractory Pseudomonas Bacteremia in a 2-Year-Old Sterilized by Bacteriophage Therapy. J. Pediatr. Infect. Dis. Soc. 2018, 7, 253–256. [Google Scholar] [CrossRef]
- Ferry, T.; Leboucher, G.; Fevre, C.; Herry, Y.; Conrad, A.; Josse, J.; Batailler, C.; Chidiac, C.; Medina, M.; Lustig, S.; et al. Salvage Debridement, Antibiotics and Implant Retention (“DAIR”) With Local Injection of a Selected Cocktail of Bacteriophages: Is It an Option for an Elderly Patient With Relapsing Staphylococcus aureus Prosthetic-Joint Infection? Open Forum Infect. Dis. 2018, 5, ofy269. [Google Scholar] [CrossRef]
- Zhvania, P.; Hoyle, N.S.; Nadareishvili, L.; Nizharadze, D.; Kutateladze, M. Phage therapy in a 16-year-old boy with netherton syndrome. Front. Med. 2017, 4, 94. [Google Scholar] [CrossRef]
- Jennes, S.; Merabishvili, M.; Soentjens, P.; Pang, K.W.; Rose, T.; Keersebilck, E.; Soete, O.; François, P.; Teodorescu, S.; Verween, G.; et al. Use of bacteriophages in the treatment of colistin-only-sensitive Pseudomonas aeruginosa septicaemia in a patient with acute kidney injury—A case report. Crit. Care 2017, 21, 129. [Google Scholar] [CrossRef]
- Leitner, L.; Ujmajuridze, A.; Chanishvili, N.; Goderdzishvili, M.; Chkonia, I.; Rigvava, S.; Chkhotua, A.; Changashvili, G.; McCallin, S.; Schneider, M.O.; et al. Intravesical bacteriophages for treating urinary tract infections in patients undergoing transurethral resection of the prostate: A randomised, placebo-controlled, double-blind clinical trial. Lancet. Infect. Dis. 2021, 21, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Fabijan, A.; Lin, R.C.Y.; Ho, J.; Maddocks, S.; Zakour, N.L.; Iredell, J.R.; Westmead Bacteriophage Therapy Team. Safety of bacteriophage therapy in severe Staphylococcus aureus infection. Nat. Microbiol. 2020, 5, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Wright, A.; Hawkins, C.H.; Änggård, E.E.; Harper, D.R. A controlled clinical trial of a therapeutic bacteriophage preparation in chronic otitis due to antibiotic-resistant Pseudomonas aeruginosa; a preliminary report of efficacy. Clin. Otolaryngol. 2009, 34, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.-S.; Kumar Biswas, S.; Tan, W.S.; Saha, A.K.; Leo, B.-F. Efficacy and potential of phage therapy against multidrug resistant Shigella spp. PeerJ 2019, 7, e6225. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Jo, Y.; Hwang, Y.J.; Hong, H.W.; Hong, S.S.; Park, K.; Myung, H. Phage-Antibiotic Synergy via Delayed Lysis. Appl. Environ. Microbiol. 2018, 84, e02085-18. [Google Scholar] [CrossRef]
- Uchiyama, J.; Shigehisa, R.; Nasukawa, T.; Mizukami, K.; Takemura-Uchiyama, I.; Ujihara, T.; Murakami, H.; Imanishi, I.; Nishifuji, K.; Sakaguchi, M.; et al. Piperacillin and ceftazidime produce the strongest synergistic phage–antibiotic effect in Pseudomonas aeruginosa. Arch. Virol. 2018, 163, 1941–1948. [Google Scholar] [CrossRef]
- Han, M.L.; Nang, S.C.; Lin, Y.W.; Zhu, Y.; Yu, H.H.; Wickremasinghe, H.; Barlow, C.K.; Creek, D.J.; Crawford, S.; Rao, G.; et al. Comparative metabolomics revealed key pathways associated with the synergistic killing of multidrug-resistant Klebsiella pneumoniae by a bacteriophage-polymyxin combination. Comput. Struct. Biotechnol. J. 2022, 20, 485–495. [Google Scholar] [CrossRef]
- Zuo, P.; Yu, P.; Alvarez, P.J.J. Aminoglycosides Antagonize Bacteriophage Proliferation, Attenuating Phage Suppression of Bacterial Growth, Biofilm Formation, and Antibiotic Resistance. Appl. Environ. Microbiol. 2021, 87, e00468-21. [Google Scholar] [CrossRef]

