1. Introduction
Interventional cardiology procedures constitute a substantial source of medical radiation exposure globally, with the potential to subject patients to significant radiation levels [1]. This concern is particularly relevant for pediatric patients with congenital heart disease, as they may necessitate multiple imaging studies, such as cardiac catheterization, which can extend examination durations and elevate radiation exposure [2]. Notably, there has been a noteworthy upsurge in the prevalence of prolonged pediatric cardiac interventions, further increasing the risk of radiation exposure in this population, primarily to the skin [3].
Children are inherently more radiation-sensitive due to factors like higher cell proliferation and percentage of undifferentiated cells, which result in increased stochastic effect risk [2]. Furthermore, their longer lifespan increases the lifetime radiogenic cancer risk [1,4]. Studies reveal 2–3 times higher cancer likelihood from radiation exposure before age 15 as compared to adults [5,6,7]. Hence, optimizing radiation doses and image quality is crucial for pediatric interventional cardiology [3,8,9].
Evaluating the radiation dose rates and image quality of X-ray systems utilized in pediatric interventional procedures is of paramount importance to strike a balance between optimal image quality and appropriate doses for these patients [10]. However, the complexity of these systems, which encompass diverse models, technologies, and operational modes, can pose challenges for cardiologists when comparing and selecting the most suitable options for a given procedure and patient size [2,11]. Thoroughly characterizing X-ray systems used in pediatric interventional procedures using phantoms with tissue-equivalent attenuation characteristics and test objects is essential to optimize procedures, guide the selection of protocols and operation modes, and ensure adequate image quality while minimizing radiation exposure to the lowest reasonably achievable levels [1,2,8,11]. This physical characterization can provide valuable data to improve procedures and facilitate informed decision making when selecting protocols and operation modes [10,11].
Regarding image quality assessment, subjective and objective methods are available. Yet subjectivity can be affected by observer performance, monitor settings, and ambient lighting, causing degradation from other independent and often controllable variables. For unbiased evaluation, software capable of displaying and manipulating DICOM images can provide a means to measure averages and deviations in multiple regions of interest (ROIs). This aids acceptance tests, determining action levels, and setting reference values for consistency checks [9].
Within this framework, the image quality metrics commonly considered are signal-to-noise ratio (SNR) [1,5,12,13,14], contrast-to-noise ratio (CNR) [9,10,11,14] and high-contrast spatial resolution (HCSR) [6,8,11,12]. These metrics can help to optimize the settings of X-ray systems for different patient sizes, ensuring comparable image quality while minimizing patient radiation doses [11]. By utilizing these objective measures, healthcare professionals can make informed decisions regarding the selection of protocols and operation modes for pediatric interventional procedures, prioritizing patient safety, and achieving optimal imaging outcomes.
This systematic review aims to provide a comprehensive analysis of the current understanding of physical image quality metrics relevant to X-ray systems in pediatric interventional cardiology, considering the main factors reported in the literature that influence this outcome. The review addresses the following research questions (RQs):
- ▪
- RQ 1: What are the primary physical image quality metrics commonly utilized for characterizing X-ray systems employed in fluoroscopy-guided pediatric interventional cardiac procedures, and what are the prevalent methods employed to measure these metrics?
- ▪
- RQ 2: What factors have been examined in the literature for their impact on physical image quality metrics in characterizing X-ray systems used in fluoroscopy-guided pediatric interventional cardiac procedures?
By thoroughly analyzing the responses to these research questions, this study seeks to clarify the current understanding of physical image quality metrics applicable to X-ray systems used in pediatric interventional cardiology. The findings from this review provide significant insights that can enhance clinical practice and inform future research in this field.
2. Materials and Methods
Between March and April 2023, we conducted a systematic literature review, utilizing Scopus and Web of Science as the main sources of information. The search strategy incorporated relevant descriptors, including image quality, signal-to-noise ratio, contrast-to-noise ratio, spatial resolution, pediatric, interventional, and cardiology. The search filters were narrowed to primary articles in English and Spanish, with publication dates ranging from 2000 to 2022.
To be included in the review, articles had to meet specific criteria: they (i) evaluated image quality using physical metrics, (ii) focused on characterizing X-ray systems employed in fluoroscopy-guided cardiac interventional procedures, and (iii) involved pediatric patients. Exclusion criteria comprised irrelevant topics, descriptive articles, literature reviews, studies conducted using other imaging techniques or involving adult patients, those lacking objective evaluation of image quality, and those inaccessible in full text. The article selection process followed the guidelines outlined by the PRISMA initiative [15], and it was performed as depicted in Figure 1.
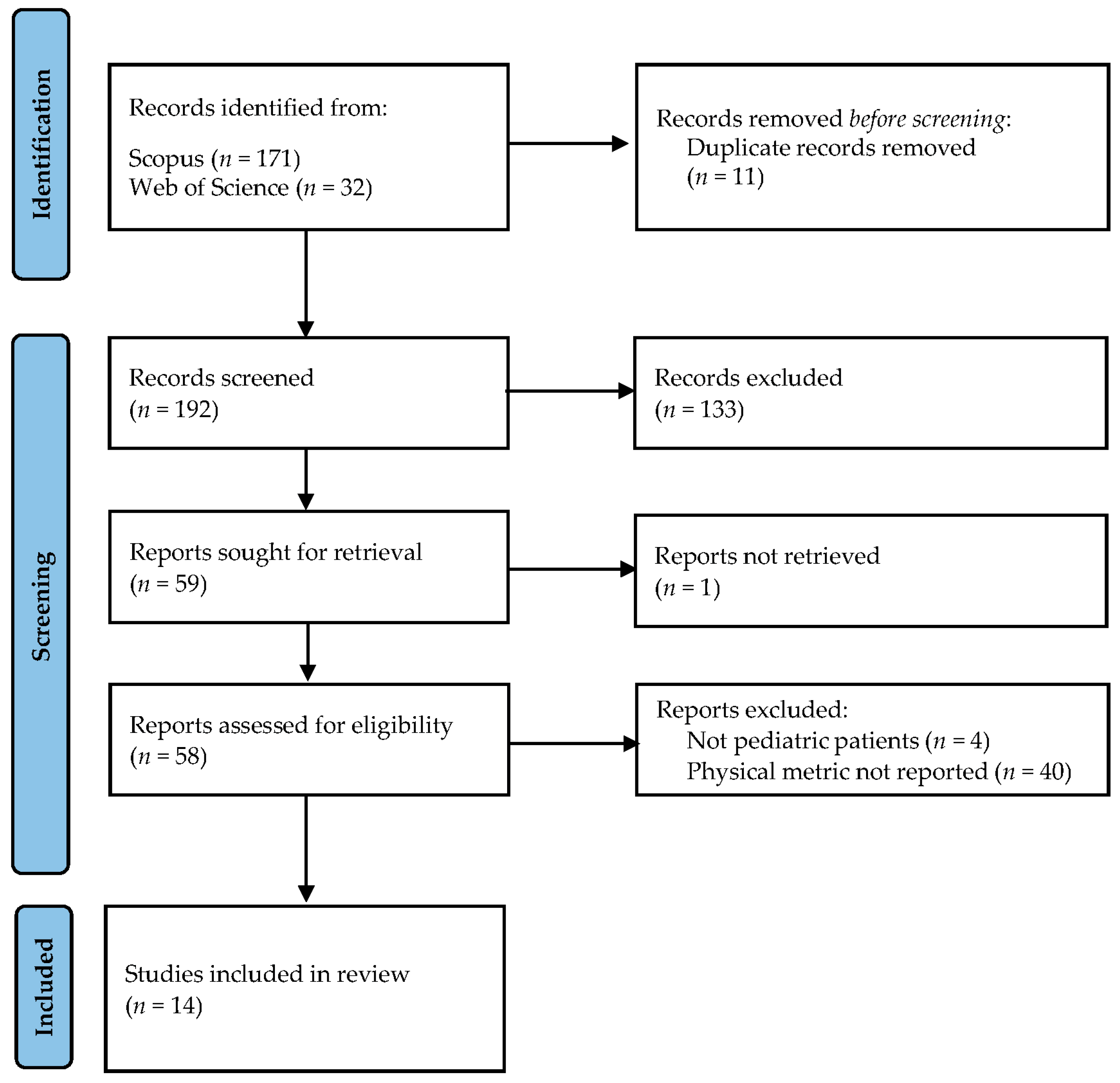
Figure 1. Flowchart of the article selection process in the current systematic review following the PRISMA initiative.
After eliminating duplicate entries, authors D.N. and K.V. conducted a comprehensive evaluation of titles and abstracts. Through collaborative discussions, both authors collectively reached conclusions. When a consensus was established, the articles proceeded to the next stage. If not, a more in-depth assessment of the work’s relevance was conducted before arriving at a final decision.
Once the two main reviewers had agreed on the articles to be included, they independently delved into the full texts. The information was systematically organized, considering the specific metric used to evaluate physical image quality, the assessment methods employed, the angiographic system utilized, factors influencing image quality, and the primary findings of each study. Subsequently, both authors compared their individual decisions regarding the selected articles. Any differences in opinion were thoroughly addressed through further dialogue. Ultimately, all three authors collaboratively determined the final inclusion, resulting in a careful selection of 14 articles for the final analysis.
Regarding the critical appraisal of the included studies, it is important to note that we did not find published tools for experimental studies. However, we deemed it appropriate to develop a specific instrument for this study, consisting of six criteria that addressed aspects of methodology, results reporting, and analysis of potential biases by the authors. Our tool was based on criteria derived from the ARRIVE guidelines 2.0 [16], as well as the Joanna Briggs Institute’s (JBI) Critical Appraisal Checklist for Randomized Controlled Trials [17] and Quasi-Experimental Studies [18]. Specifically, authors D.N. and K.V. independently conducted a manual assessment of bias for each study. Afterward, an overall risk-of-bias rating was assigned to each study. Studies meeting five or six of the evaluated criteria were categorized as having low risk of bias. Those fulfilling three or four criteria were classified as having moderate risk, whereas high risk of bias was linked to works satisfying two or fewer of the analyzed aspects.
3. Results
We conducted a systematic review of physical image quality metrics for X-ray systems used in fluoroscopy-guided pediatric interventional procedures. After screening, 14 studies (published between 2000 and 2022) met the inclusion criteria.
3.1. Physical Image Quality Assessment
displays the selected studies obtained from the search strategy. The table provides essential details, including the last name of the first author, physical image quality metric assessed, test object used, software used for objective evaluation, number of frames analyzed, matrix size, and bit depth. The most frequently reported metric was SNR (n = 10), followed by HCSR (n = 8). Additionally, C (n = 3) and CNR (n = 3) were also reported, while N and SdNR appeared in a smaller number of studies (n = 1 each).
3.2. Equations Utilized for Physical Image Quality Metrics Calculation
In this section, we present the equations utilized for calculating the physical image quality metrics.
3.3. Factors Influencing Image Quality
provides an overview of the factors and categories investigated by each selected article obtained from the employed search strategy.
3.4. Assessment of Bias Risk
Figure 2A shows an individual critical appraisal of the selected articles, based on the estimated risk of bias according to six criteria (C1 to C6). Meanwhile, the summary of information for each criterion is presented in Figure 2B. A predominance of studies with low risk of bias was observed for the three criteria evaluating the methodology used (C1–C3), with performance ranging from 71.4% to 92.9%. Among these, C1 revealed a predominance of comprehensive reporting of the materials and methods employed (78.6%), with a low proportion of studies omitting certain details. Although these details hold significance when comparing the results with those of other authors, they do not intrinsically compromise the validity of the results obtained. Criterion C2 exhibited the highest degree of compliance, indicating the use of valid test objects and computational analysis strategies that support the objectivity of the methodology for analyzing physical image quality metrics. Finally, C3 indicated a prevalence of studies carrying out statistical analyses appropriate to the purpose of the work (71.4%), followed by articles that, although they used descriptive statistics, omitted the necessary comparative measures to support the differences between the groups studied.
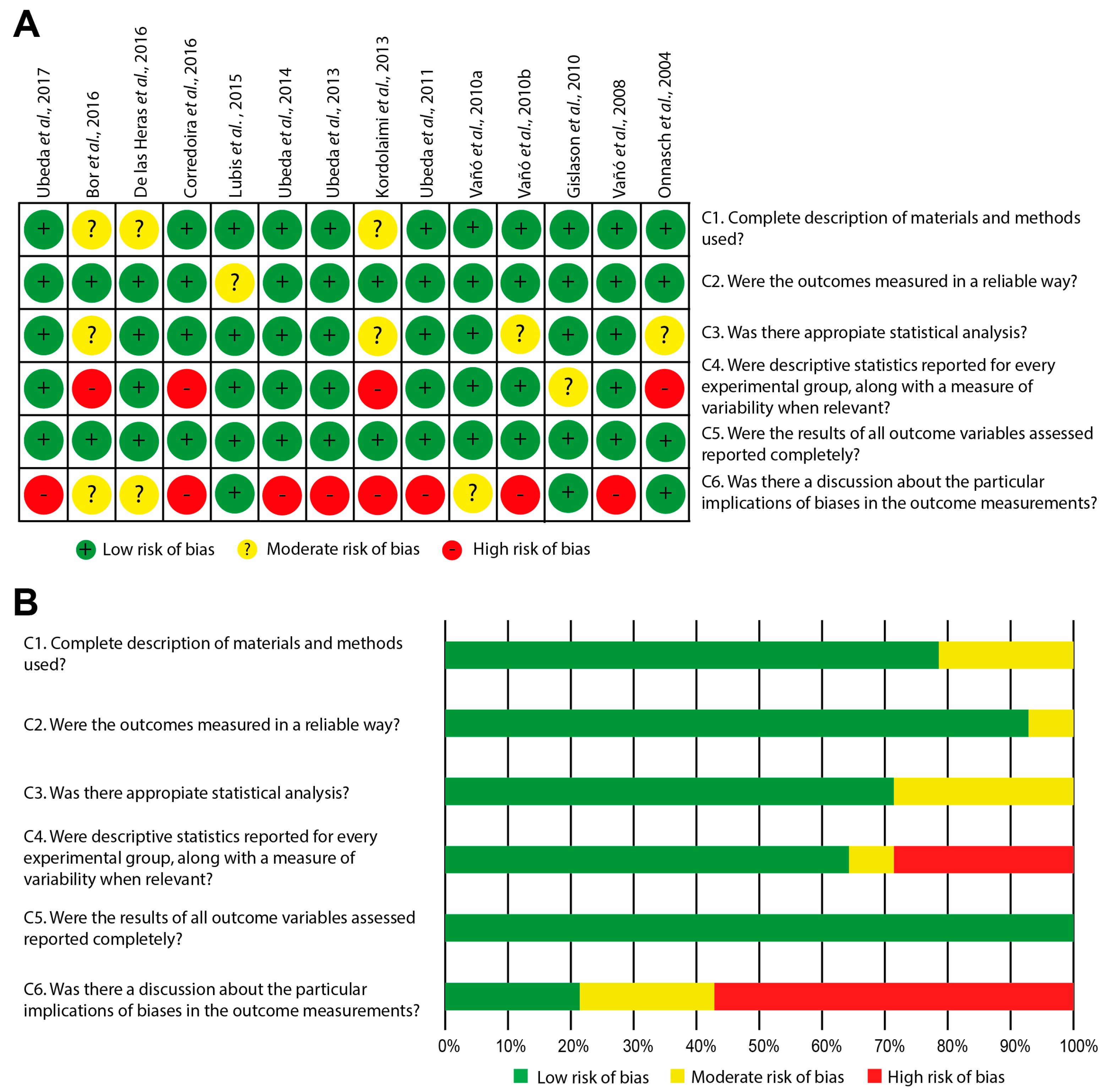
Figure 2. (A) Individual risk-of-bias assessment for the articles included in the systematic review (Ubeda et al., 2017 [1]; Bor et al., 2016 [12]; De las Heras et al., 2016 [9]; Corredoira et al., 2016 [13]; Lubis et al., 2015 [5]; Ubeda et al., 2014 [2]; Ubeda et al., 2013 [4]; Kordolaimi et al., 2013 [19]; Ubeda et al., 2011 [8]; Vañó et al., 2010a [20]; Vañó et al., 2010b [6]; Gislason et al., 2010 [10]; Vañó et al., 2008 [11]; Vañó et al., 2004 [7]). (B) Summary graph depicting the results obtained for each evaluated criterion.
Conversely, regarding the reporting of measures of outcome variability (C4), it was found that 64.3% of studies met this aspect. Concerning the completeness of reporting outcome variables (C5), it was established that all works successfully fulfilled this criterion. Lastly, the aspect showing the highest bias risk was the discussion of implications related to potential study biases, an area that was scarcely addressed by the analyzed studies (21.4%), with a significant percentage of works omitting this aspect (57.1%), as depicted in Figure 2A,B.
4. Discussion
Characterizing angiographic equipment for pediatric use is of utmost importance, given the intricacy of X-ray systems in pediatric interventional procedures [2]. This characterization entails assessing dose and image quality using diverse techniques, such as entrance surface air kerma (Ka,e) measurement and image quality assessment with test objects. Such evaluations enable cardiologists to identify optimal protocols and operation modes that strike a balance between image quality and dose, thereby minimizing potential long-term tissue damage in vulnerable pediatric patients [1,10]. Additionally, this evaluation facilitates the selection of appropriate operation modes for different procedures and patient sizes, ensuring the safe and effective use of fluoroscopy-guided pediatric cardiac interventions [11].
This article presents a comprehensive analysis of the current understanding of physical image quality metrics relevant to X-ray systems in pediatric interventional cardiology. The information gathered for this purpose is provided below, aligning with the research questions addressed in this study.
4.1. What Are the Primary Physical Image Quality Metrics Commonly Utilized for Characterizing X-ray Systems Employed in Fluoroscopy-Guided Pediatric Interventional Cardiac Procedures, and What Are the Prevalent Methods Employed to Measure These Metrics?
presents the most evaluated physical image quality metrics in the included studies, comprising N, SNR, SdNR, C, CNR, and HCSR. These metrics hold significant importance in characterizing the fluoroscopic systems used in pediatric interventional cardiology procedures and are detailed below:
4.2. What Factors Have Been Examined in the Literature for Their Impact on Physical Image Quality Metrics in Characterizing X-ray Systems Used in Fluoroscopy-Guided Pediatric Interventional Cardiac Procedures?
4.3. Final Remarks
One commonly considered parameter in articles on optimization was the Figure of Merit (FOM), which complements objective image quality information with the value of an estimated magnitude in the procedure, such as Ka,e. Therefore, this parameter aids in assessing the system’s efficiency in terms of the Ka,e used to form a radiological image and should be reported together with the evaluated metrics [1,2,5,6,8,10,13,19].
This comprehensive review highlights the importance of optimizing X-ray system configurations and dynamic FPD settings in pediatric cardiac interventional procedures, considering radiation dose levels and specific clinical needs. The utilization of image quality metrics, such as SNR, HCSR, C, and CNR, plays a pivotal role in refining imaging parameters and making informed clinical decisions, ultimately leading to improved diagnostic accuracy and enhanced patient care. These metrics not only aid in quality control and technique/system comparisons but also effectively reduce radiation exposure in pediatric patients. Personalized protocols based on image quality metrics can minimize fluoroscopy time while maintaining high image quality. Nevertheless, it is crucial to consider the specific context, as the direct applicability of these metrics may be limited for certain interventional devices. Overall, integrating image quality metrics into medical practice shows significant promise in optimizing pediatric patient dose and image quality, benefiting cardiac X-ray imaging, and advancing medical procedures in this field.
The systematic review’s findings have clinical and practical implications for pediatric healthcare and clinical practice. By understanding the most used physical image quality metrics and their impact on image characteristics, clinicians can optimize imaging protocols and balance image quality and dose for pediatric interventional procedures.
4.4. Study Limitations
The most important limitations of this systematic review were as follows. Firstly, the analysis included articles published within a 23-year period, which might have excluded more recent studies with relevant findings. Additionally, preprint studies and unpublished data were not considered, potentially leading to the omission of valuable information. Moreover, the review was limited to studies published in English and Spanish, which could introduce language bias and overlook relevant studies in other languages. The low number of eligible references was another limitation, especially given the broad range of metrics considered, some of which were scarcely reported in the literature.
One of the retrieved articles employed an in-house phantom, created by the researchers themselves, to assess the study’s variables of interest. However, this phantom lacked formal validation, meaning that the results offer trends but do not allow for direct comparisons with other studies. Another potential limitation was that some of the included studies may be dated, which could result in the inclusion of X-ray equipment that is now considered obsolete or rarely used. These systems may not have contemporary relevance in terms of their use. However, it is important to note that this factor was addressed as a fundamental aspect of the development of the concepts analyzed. Furthermore, this consideration is influenced by the parallels that exist between II- and FPD-based technologies.
In addition, some articles omitted important information, such as the program used to extract data from ROIs, number of images analyzed, size of the image matrix, and color depth, which could affect the comprehensiveness of the analysis. Likewise, within the bias analysis (Figure 2), the need to enhance results reporting becomes apparent. This entails incorporating relevant measures of variability and discussing the limitations of studies, thereby facilitating the transparency of aspects that could potentially impact the validity of the obtained results. It is worth noting that the outcomes of studies with high bias risk were only considered when they aligned with findings reported in other studies possessing lower bias risk.
Finally, for some metrics, there was no consensus on the formula to calculate image quality, resulting in different approaches between studies. Consequently, the results may provide trends but require careful interpretation and consideration before applying them to current imaging systems and protocols.
4.5. Future Research Directions
The future trends in pediatric interventional cardiology imaging research hold significant potential for enhancing the understanding of the field. Addressing the limitations identified in the systematic review, future studies should consider expanding the inclusion criteria to encompass more research and provide a more comprehensive dataset for analysis. Additionally, researchers are encouraged to validate in-house phantoms before utilization to ensure the accuracy and reliability of results. Furthermore, comprehensive reporting of study details should be considered to improve the transparency and comparability of future investigations. To foster consistency and comparability across studies, the establishment of consensus guidelines or recommendations for calculating and reporting physical image quality metrics is essential. Exploring and developing novel image quality metrics that consider the unique characteristics and imaging needs of pediatric patients could further advance the field. Future researchers should consider examining the relationship between image quality metrics and long-term patient outcomes in pediatric interventional cardiology to shed light on the impact of image optimization on patient care and safety.
5. Conclusions
The systematic review provided insight into the use of physical image quality metrics to characterize X-ray equipment in fluoroscopy-guided pediatric interventional cardiac procedures. The evaluation of N, SNR, C, CNR, and HCSR provided valuable information on the factors influencing image quality and dose in pediatric interventions. By optimizing imaging parameters based on these metrics, clinicians can improve diagnostic outcomes, improve patient safety, and minimize radiation exposure for vulnerable pediatric patients. However, it is important to recognize that these metrics may not fully capture clinical processes, as they do not account for the image visualization process and observer perception of image quality. Nevertheless, they offer a valuable approach to assessing image quality and enrich the quality assessment process, complementing human observer evaluations.
References
- Ubeda, C.; Salazar, L.; Retana, V.; Santos, F.; Salvador, L.; Sáenz, C.; Quesada, C.; Gavarrete, M.; Picado, M.; Arce, L. Characterization and Experimental Measurements of Scatter Dose at Cardiologist’s Eyes during Paediatric Interventional Cardiology Procedures in Costa Rica. Radiat. Prot. Dosim. 2017, 176, 450–455. [Google Scholar] [CrossRef] [PubMed]
- Ubeda, C.; Miranda, P.; Dalmazzo, D. Evolution of Radiation Dose and Image Quality in a Pediatric Interventional Cardiology System [Dosis de Radiación y Calidad de Imagen En Un Equipo de Cardiología Intervencionista Pediátrico]. Interciencia 2014, 39, 518–523. [Google Scholar]
- Azizmohammadi, F.; Navarro Castellanos, I.; Miró, J.; Segars, P.; Samei, E.; Duong, L. Generative Learning Approach for Radiation Dose Reduction in X-ray Guided Cardiac Interventions. Med. Phys. 2022, 49, 4071–4081. [Google Scholar] [CrossRef] [PubMed]
- Ubeda, C.; Vano, E.; Gonzalez, L.; Miranda, P. Influence of the Antiscatter Grid on Dose and Image Quality in Pediatric Interventional Cardiology X-ray Systems. Catheter. Cardiovasc. Interv. 2013, 82, 51–57. [Google Scholar] [CrossRef]
- Lubis, L.E.; Bayuadi, I.; Pawiro, S.A.; Ng, K.-H.; Bosmans, H.; Soejoko, D.S. Optimization of Dose and Image Quality of Paediatric Cardiac Catheterization Procedure. Phys. Medica 2015, 31, 659–668. [Google Scholar] [CrossRef]
- Vañó, E.; Ubeda, C.; Martinez, L.C.; Leyton, F.; Miranda, P. Paediatric Interventional Cardiology: Flat Detector versus Image Intensifier Using a Test Object. Phys. Med. Biol. 2010, 55, 7287–7297. [Google Scholar] [CrossRef]
- Onnasch, D.G.W.; Schemm, A.; Kramer, H.-H. Optimization of Radiographic Parameters for Paediatric Cardiac Angiography. Br. J. Radiol. 2004, 77, 479–487. [Google Scholar] [CrossRef]
- Ubeda, C.; Vano, E.; Miranda, P.; Leyton, F.; Martinez, L.C.; Oyarzun, C. Radiation Dose and Image Quality for Paediatric Interventional Cardiology Systems. A National Survey in Chile. Radiat. Prot. Dosim. 2011, 147, 429–438. [Google Scholar] [CrossRef]
- de las Heras, H.; Torres, R.; Fernández-Soto, J.M.; Vañó, E. Objective Criteria for Acceptability and Constancy Tests of Digital Subtraction Angiography. Phys. Medica 2016, 32, 272–276. [Google Scholar] [CrossRef]
- Gislason, A.J.; Davies, A.G.; Cowen, A.R. Dose Optimization in Pediatric Cardiac X-ray Imaging. Med. Phys. 2010, 37, 5258–5269. [Google Scholar] [CrossRef]
- Vano, E.; Ubeda, C.; Leyton, F.; Miranda, P. Radiation Dose and Image Quality for Paediatric Interventional Cardiology. Phys. Med. Biol. 2008, 53, 4049. [Google Scholar] [CrossRef] [PubMed]
- Bor, D.; Birgul, O.; Onal, U.; Olgar, T. Investigation of Grid Performance Using Simple Image Quality Tests. J. Med. Phys. 2016, 41, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Corredoira, E.; Vañó, E.; Alejo, L.; Ubeda, C.; Gutiérrez-Larraya, F.; Garayoa, J. Biplane Interventional Pediatric System with Cone-Beam CT: Dose and Image Quality Characterization for the Default Protocols. J. Appl. Clin. Med. Phys. 2016, 17, 357–376. [Google Scholar] [CrossRef]
- Vassileva, J.; Vano, E.; Ubeda, C.; Rehani, M.; Zotova, R. Impact of the X-ray System Setting on Patient Dose and Image Quality; a Case Study with Two Interventional Cardiology Systems. Radiat. Prot. Dosim. 2013, 155, 329–334. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- du Sert, N.P.; Hurst, V.; Ahluwalia, A.; Alam, S.; Avey, M.T.; Baker, M.; Browne, W.J.; Clark, A.; Cuthill, I.C.; Dirnagl, U.; et al. The ARRIVE Guidelines 2.0: Updated Guidelines for Reporting Animal Research. PLoS Biol. 2020, 18, e3000410. [Google Scholar] [CrossRef]
- Tufanaru, C.; Munn, Z.; Aromataris, E.; Campbell, J.; Hopp, L. Chapter 3: Systematic Reviews of Effectiveness. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; Joanna Brggs Institute: Adelaide, Australia, 2020. [Google Scholar]
- Tufanaru, C.; Munn, Z.; Aromataris, E.; Campbell, J.; Hopp, L. Chapter 3: Systematic Reviews of Effectiveness. In Joanna Briggs Institute Reviewer’s Manual; Aromataris, E., Munn, Z., Eds.; The Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Kordolaimi, S.D.; Salvara, A.L.N.; Antonakos, I.; Tsalafoutas, I.A.; Broutzos, E.; Efstathopoulos, E.P. Comparative Performance Evaluation of a Flat Detector and an Image Intensifier Angiographic System Both Used for Interventional Cardiology Procedures in Adult and Pediatric Patients. Phys. Medica 2013, 29, 178–187. [Google Scholar] [CrossRef] [PubMed]
- Vano, E.; Ubeda, C.; Geiger, B.; Martinez, L.C.; Balter, S. Influence of Image Metrics When Assessing Image Quality from a Test Object in Cardiac X-ray Systems. J. Digit. Imaging 2010, 24, 331–338. [Google Scholar] [CrossRef]
- Konstantinidis, A. Physical Parameters of Image Quality. In Comprehensive Biomedical Physics; Elsevier: Amsterdam, The Netherlands, 2014; pp. 49–63. [Google Scholar] [CrossRef]
- Williams, M.B.; Krupinski, E.A.; Strauss, K.J.; Breeden, W.K.; Rzeszotarski, M.S.; Applegate, K.; Wyatt, M.; Bjork, S.; Seibert, J.A. Digital Radiography Image Quality: Image Acquisition. J. Am. Coll. Radiol. 2007, 4, 371–388. [Google Scholar] [CrossRef]
- Morin, R.; Mahesh, M. Role of Noise in Medical Imaging. J. Am. Coll. Radiol. 2018, 15, 1309. [Google Scholar] [CrossRef]
- Lamers, L.J.; Morray, B.H.; Nugent, A.; Speidel, M.; Suntharos, P.; Prieto, L. Multicenter Assessment of Radiation Exposure during Pediatric Cardiac Catheterizations Using a Novel Imaging System. J. Interv. Cardiol. 2019, 2019, 7639754. [Google Scholar] [CrossRef] [PubMed]
- Huda, W.; Sajewicz, A.M.; Ogden, K.M.; Dance, D.R. Experimental Investigation of the Dose and Image Quality Characteristics of a Digital Mammography Imaging System. Med. Phys. 2003, 30, 442–448. [Google Scholar] [CrossRef] [PubMed]
- Nocetti, D.; Ubeda, C.; Calcagno, S.; Acevedo, J.; Pardo, D. Comparison of Image Quality among Three X-ray Systems for Chest Radiography: First Step in Optimisation. Radiat. Prot. Dosim. 2015, 165, 386–391. [Google Scholar] [CrossRef]
- Ekpo, E.U.; Hoban, A.C.; McEntee, M.F. Optimisation of Direct Digital Chest Radiography Using Cu Filtration. Radiography 2014, 20, 346–350. [Google Scholar] [CrossRef]
- Verdun, F.R.; Racine, D.; Ott, J.G.; Tapiovaara, M.J.; Toroi, P.; Bochud, F.O.; Veldkamp, W.J.H.; Schegerer, A.; Bouwman, R.W.; Hernandez-Giron, I.; et al. Image Quality in CT: From Physical Measurements to Model Observers. Phys. Medica 2015, 31, 823–843. [Google Scholar] [CrossRef] [PubMed]
- TOR 18FG—Leeds Test Objects. Available online: https://leedstestobjects.com/index.php/phantom/tor-18fg/ (accessed on 10 July 2023).
- Doyle, P.; Martin, C.J.; Gentle, D. Application of Contrast-to-Noise Ratio in Optimizing Beam Quality for Digital Chest Radiography: Comparison of Experimental Measurements and Theoretical Simulations. Phys. Med. Biol. 2006, 51, 2953. [Google Scholar] [CrossRef]
- Seeram, E. Dose Optimization in Digital Radiography. In Digital Radiography; Springer: Singapore, 2019; pp. 213–227. [Google Scholar] [CrossRef]
- Strauss, K.J. Pediatric Interventional Radiography Equipment: Safety Considerations. Pediatr. Radiol. 2006, 36, 126–135. [Google Scholar] [CrossRef]
- IEC 61223-3-3:1996|IEC Webstore. Available online: https://webstore.iec.ch/publication/19374 (accessed on 20 July 2023).
- Livingstone, R.S.; Chase, D.; Varghese, A.; George, P.V.; George, O.K. Transition from Image Intensifier to Flat Panel Detector in Interventional Cardiology: Impact of Radiation Dose. J. Med. Phys. 2015, 40, 24–28. [Google Scholar] [CrossRef]
- Konst, B.; Nøtthellen, J.; Bilet, E.; Båth, M. Radiographic and Fluoroscopic X-ray Systems: Quality Control of the X-ray Tube and Automatic Exposure Control Using Theoretical Spectra to Determine Air Kerma and Dose to a Homogenous Phantom. J. Appl. Clin. Med. Phys. 2021, 22, 204–218. [Google Scholar] [CrossRef]

