A 7-year-old girl was evaluated by her pediatrician for frontal headaches, dizziness, vomiting, and pulsatile tinnitus. The workup included computed tomography (CT) and magnetic resonance imaging (MRI) of the head, which demonstrated a 6 × 6.6 × 7.1-cm left frontal lobe mass. Further imaging was negative for additional visceral or osseous lesions. She was treated with total resection, adjuvant chemotherapy, and local radiation. Histology was consistent with a dural-based leiomyosarcoma.
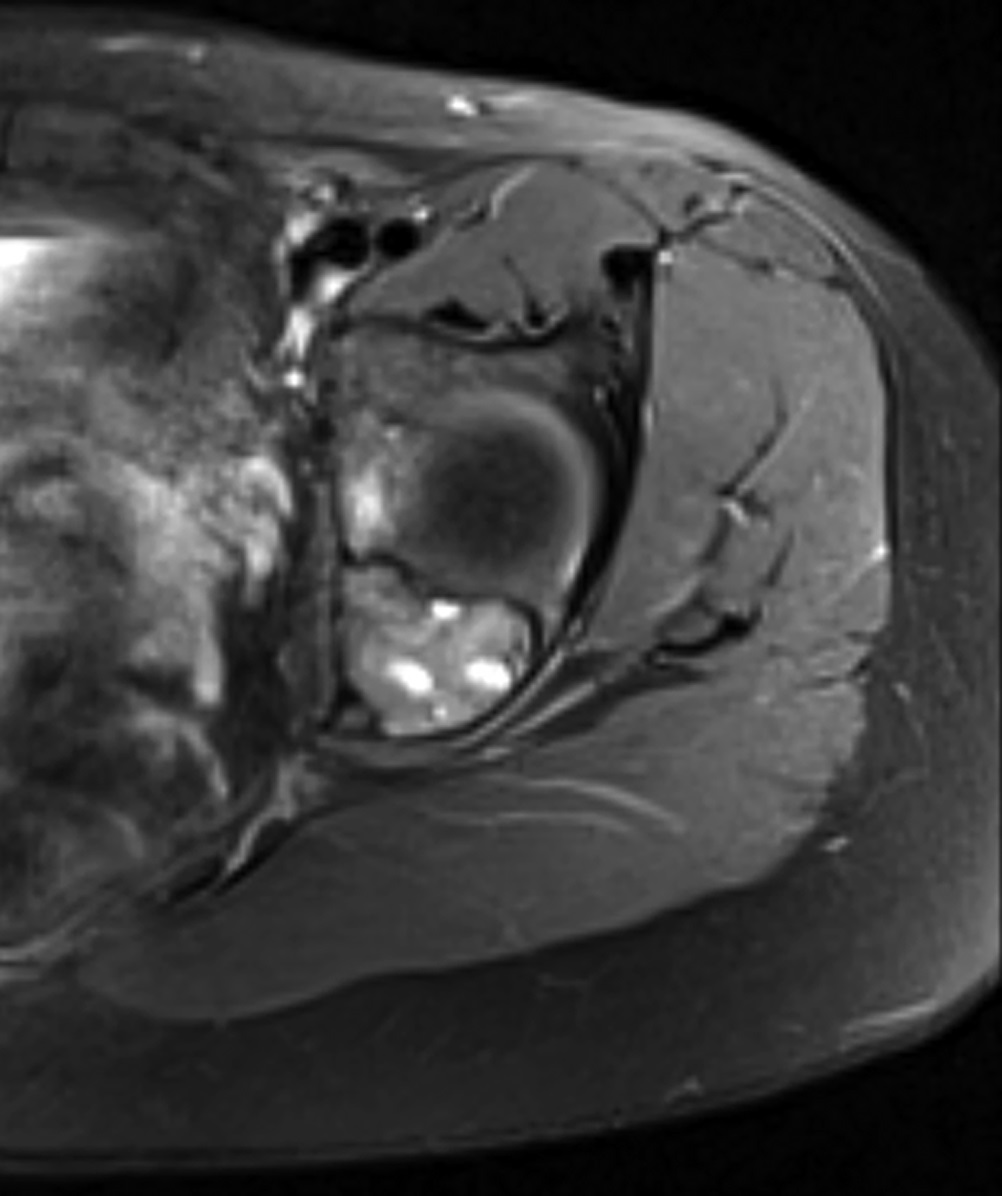
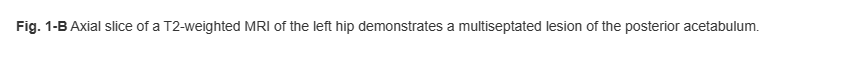
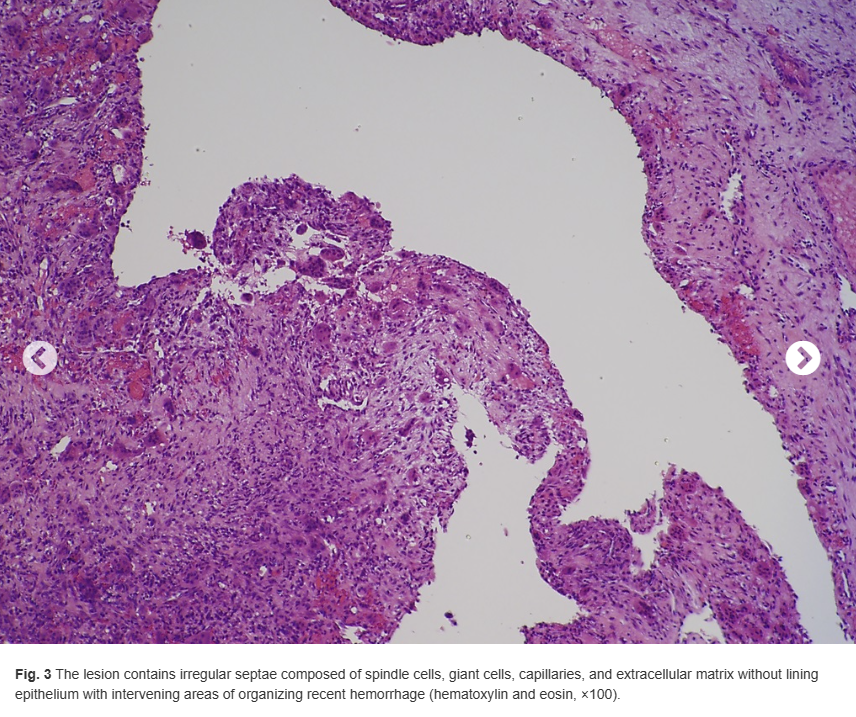
The patient first presented to our orthopaedic oncology clinic at the age of 12 years with the chief symptom of atraumatic left hip pain of 1 year in duration, causing her to limp. The initial workup included whole-body bone scan, radiograph of the pelvis (Fig. 1-A), and MRI (Figs. 1-B and 1-C) of the left hip by which a lesion of the left posterior column and ischium was identified. A CT-guided needle biopsy was obtained, and the patient underwent arterial embolization of several branches of the left obturator artery. A follow-up MRI 1 month later demonstrated an increase in cystic formation and size of the lesion. The patient subsequently underwent percutaneous CT-guided chemical ablation with doxycycline with albumin twice within 2 months. Six weeks later, an MRI of the pelvis demonstrated a decrease in the cystic component of the lesion. She had temporary alleviation of her symptoms until presenting to the hospital 3 months later with atraumatic, acute-onset left hip pain and inability to bear weight. No pathologic fractures were noted on CT. She followed up at the orthopaedic oncology clinic, and surgical intervention was recommended. The patient underwent intralesional curettage and grafting with PRO-DENSE synthetic bone graft substitute for structural support through a posterior approach (Fig. 2). Histologic findings from the intraoperative biopsy are shown in Figure 3. Recommendations were made for 2 months of non-weight-bearing followed by surveillance imaging with CT to assess the structural integrity of the pelvis and with MRI to rule out recurrence, although these studies were not completed until 9 months postoperatively. Recommendations were then made for a repeat MRI 6 months later, after which she would undergo continued surveillance with serial radiographs. The patient began bearing full weight at 1 month postoperatively and returned to sports after 10 months. At 32 months postoperatively, she had no signs of recurrence.

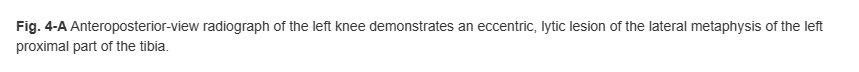
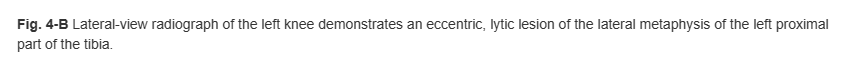
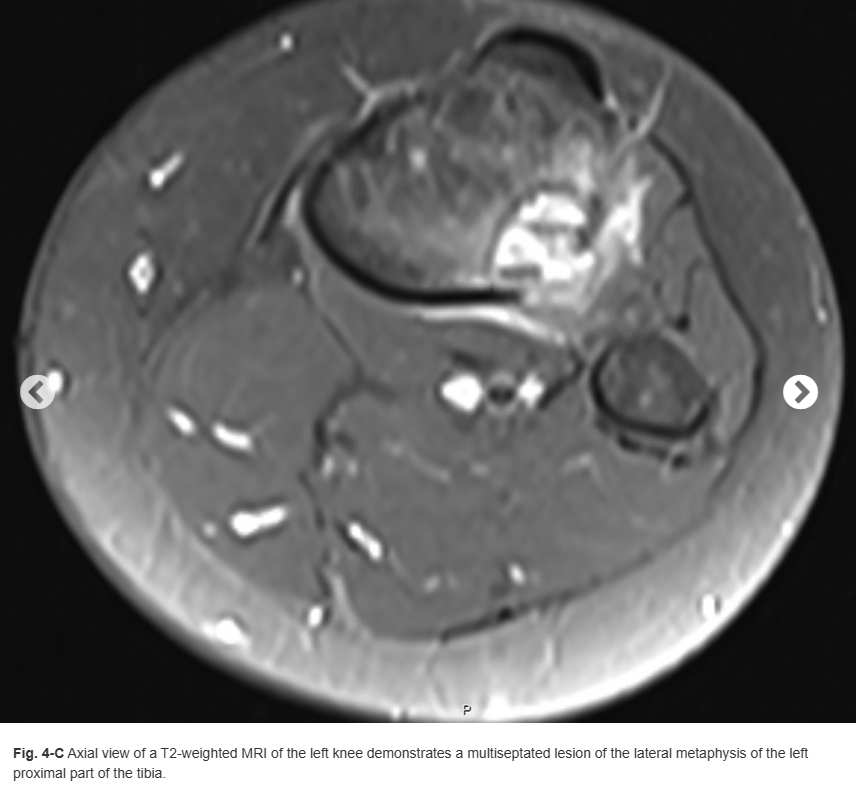
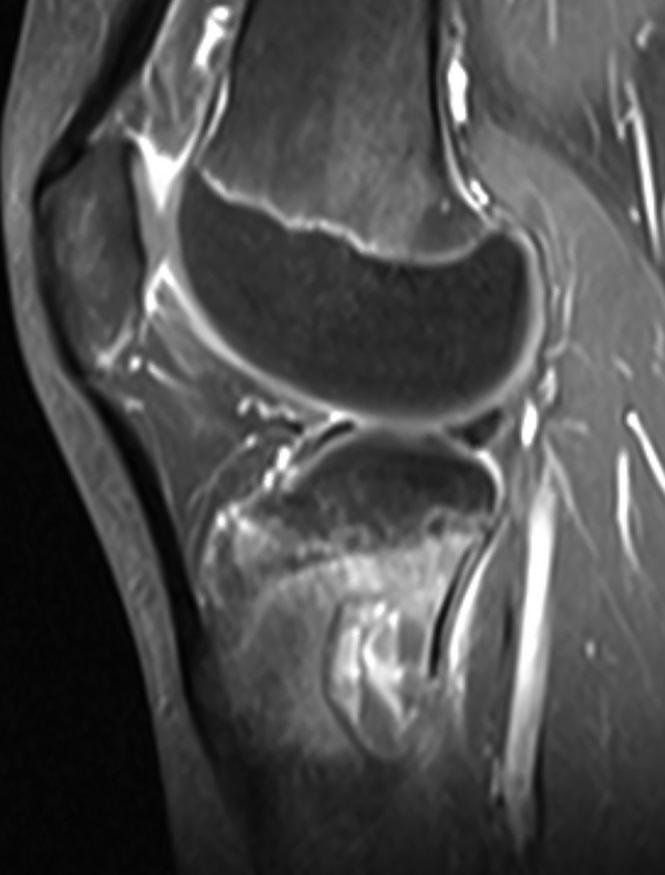
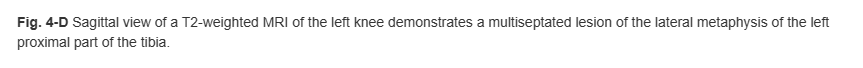
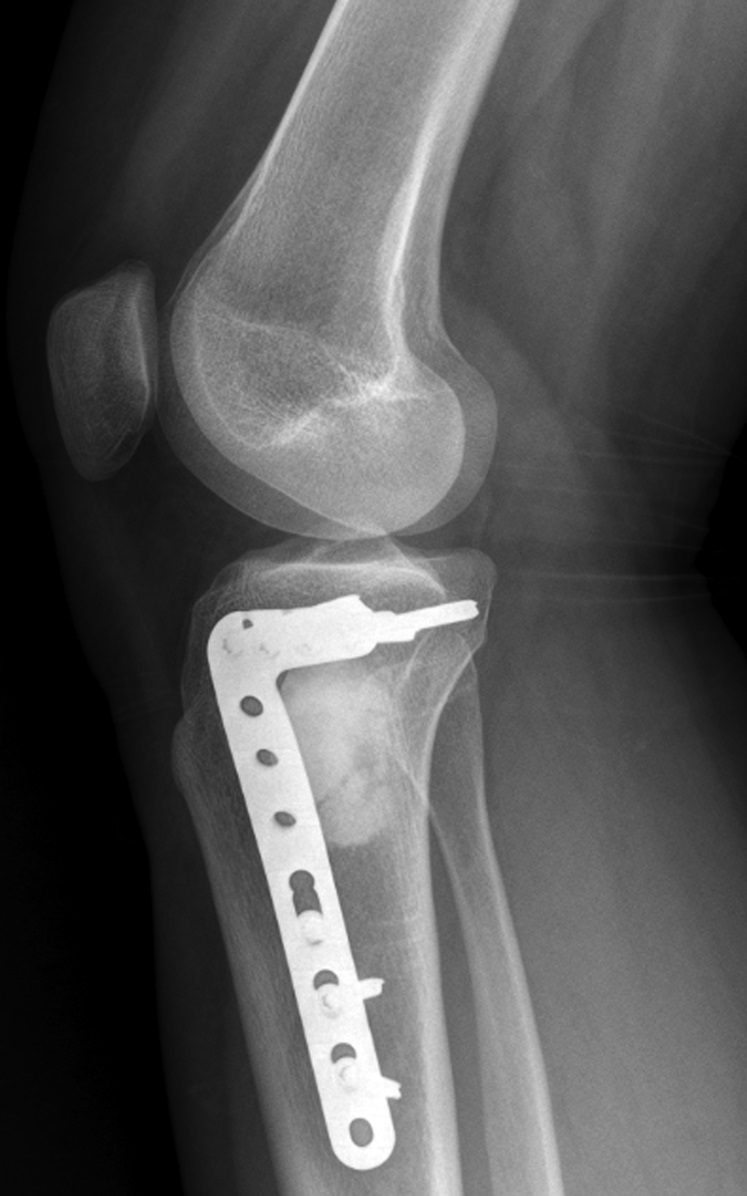
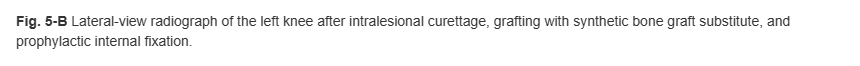
The patient again presented to the orthopaedic oncology clinic at the age of 14 years with the chief symptom of left knee pain after a minor fall. Radiographs and MRI of the knee are shown in Figures 4-A through 4-D. Bone scan demonstrated increased uptake in the left proximal part of the tibia. The patient underwent intralesional curettage, grafting with Norian synthetic bone graft substitute, and prophylactic internal fixation (Figs. 5-A and 5-B). Histology from the intraoperative biopsy is shown in Figure 6. Recommendations were made for protected weight bearing with crutches and a knee immobilizer for 2 weeks, followed by gradual weaning from crutches and knee immobilizer. The patient returned to normal daily activities after 4 weeks, and physical therapy was initiated. She was instructed to refrain from athletic activity for another month. Surveillance imaging with serial radiographs was recommended. At 12 months postoperatively, she showed no signs of recurrence.


In the event that she developed pain at an additional site, the patient was instructed to return for clinical evaluation with radiographs and possibly MRI.
What is the diagnosis?

