A 44-year-old Venezuelan woman presented with a 2-year history of pelvic, hip, and lower-extremity aching and pain. As a child, she had persistent lower-extremity pain that was interpreted as growing pains. At the age of 18 years, she was diagnosed with dermatomyositis based on a muscle biopsy and electromyographic study. She also had a rash on the face and anterior chest that had fluctuated. The patient was treated for 3 years with 16 mg of methylprednisolone; this medication was then tapered off over a period of 2 years. She remained in remission until the age of 42 years when she developed fatigability and diplopia mainly on the left lateral gaze and 2 months later on the right lateral gaze. She was hospitalized, and extensive laboratory tests, acetylcholine receptor antibody titers, and brain imaging (computed tomography [CT], magnetic resonance imaging [MRI], and angiogram) results were unremarkable. She continued having fatigability, muscle stiffness, and weakness going up stairs or with any strenuous activity. Her medical history also included hypertension, hypercholesteremia, gastritis, migraines, and polymyositis. On presentation, she reported diplopia and dizziness, but noted that she did not have constitutional symptoms such as fever, night sweats, or recent weight loss. She was seen by numerous specialists in rheumatology, neurology, and endocrinology before being evaluated by an orthopaedic surgeon. The initial diagnosis by the orthopaedic surgeon was polyostotic disease of uncertain etiology involving the pelvis and both femora.
Family history revealed that the patient’s father had died when she was young, and her sister had similar symptoms. Also, 2 of the patient’s 3 children had begun to report bone pain. Evaluation by genetics led to her family’s participation in our research studies.
Physical examination revealed an alert, oriented woman. The cranial nerves were intact without nystagmus. The patient had full strength of all extremities with a normal gait, normal deep tendon reflexes, and no sensory deficits. Hip range of motion revealed flexion to 100° and internal rotation to 15°. Hip motion was without pain, and impingement signs were negative. A full examination of the lower extremity showed no palpable soft-tissue masses.
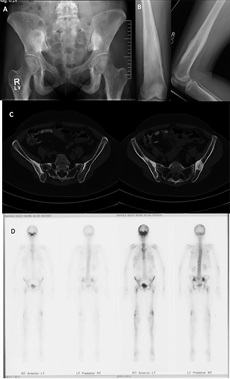
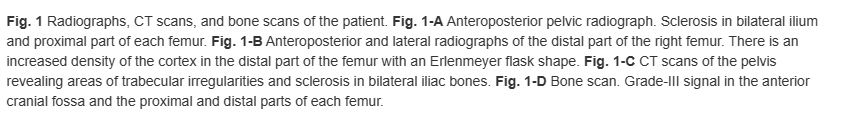
Imaging studies included radiographs of the pelvis and bilateral lower extremities, bone scan, CT scans of the pelvis and orbits, and MRI scans of the pelvis and brain (Figs. 1 and 2). Radiographs revealed hyperostosis and cortical thickening in bilateral proximal and distal parts of the femur. The distal metaphysis of each femur demonstrated an Erlenmeyer-flask shape (Figs. 1-A and 1-B). Radiographs and CT scans revealed hyperostosis and cortical thickening in bilateral posterior ilia (Figs. 1-A and 1-C). Bone scans displayed increased activity in the anterior cranial fossa, bilateral posterior ilia, and proximal and distal parts of the femora (Fig. 1-D). MRI scans of the pelvis showed marrow edema within the proximal femoral diaphysis, extending into the femoral neck at the level of the lesser trochanter with diffuse cortical thickening (Fig. 2-A). Radiographs of the hands and feet revealed thickening of proximal phalanges and metatarsal cortical thickening. The CT scans of the orbits revealed a thickened appearance of the frontal facial bone indicating hyperostosis frontalis internus and thickening of the base of the skull (Fig. 2-B). Brain MRI scans revealed normal brain architecture except for cranial base thickening. Laboratory studies revealed elevated alkaline phosphatase, liver enzymes, and cholesterol. The patient was found to have anemia and decreased vitamin D levels. Her thyroid hormones were normal, and analysis for heavy metals was negative.

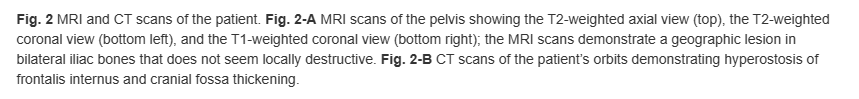
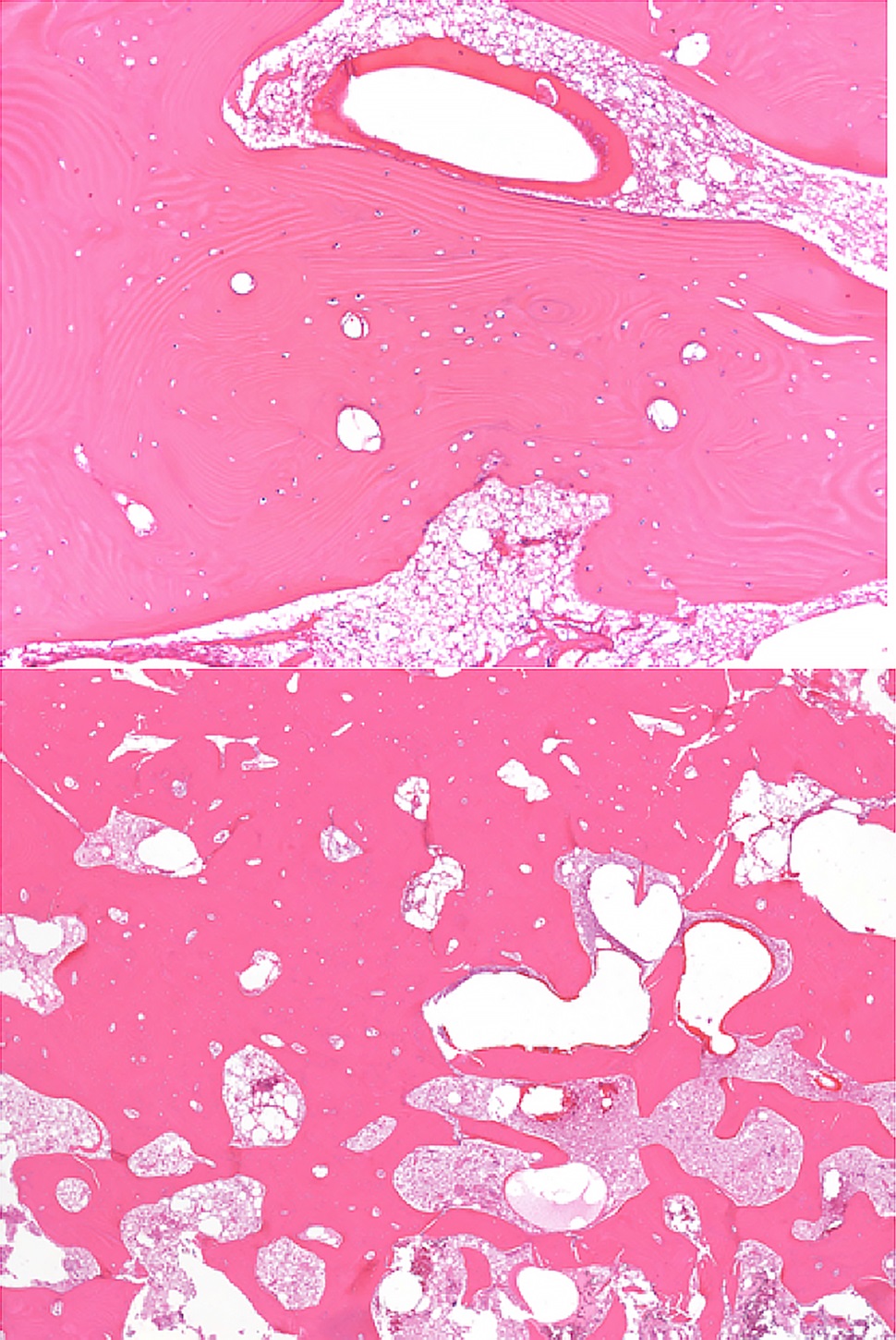
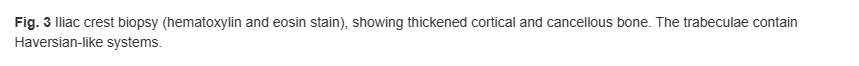
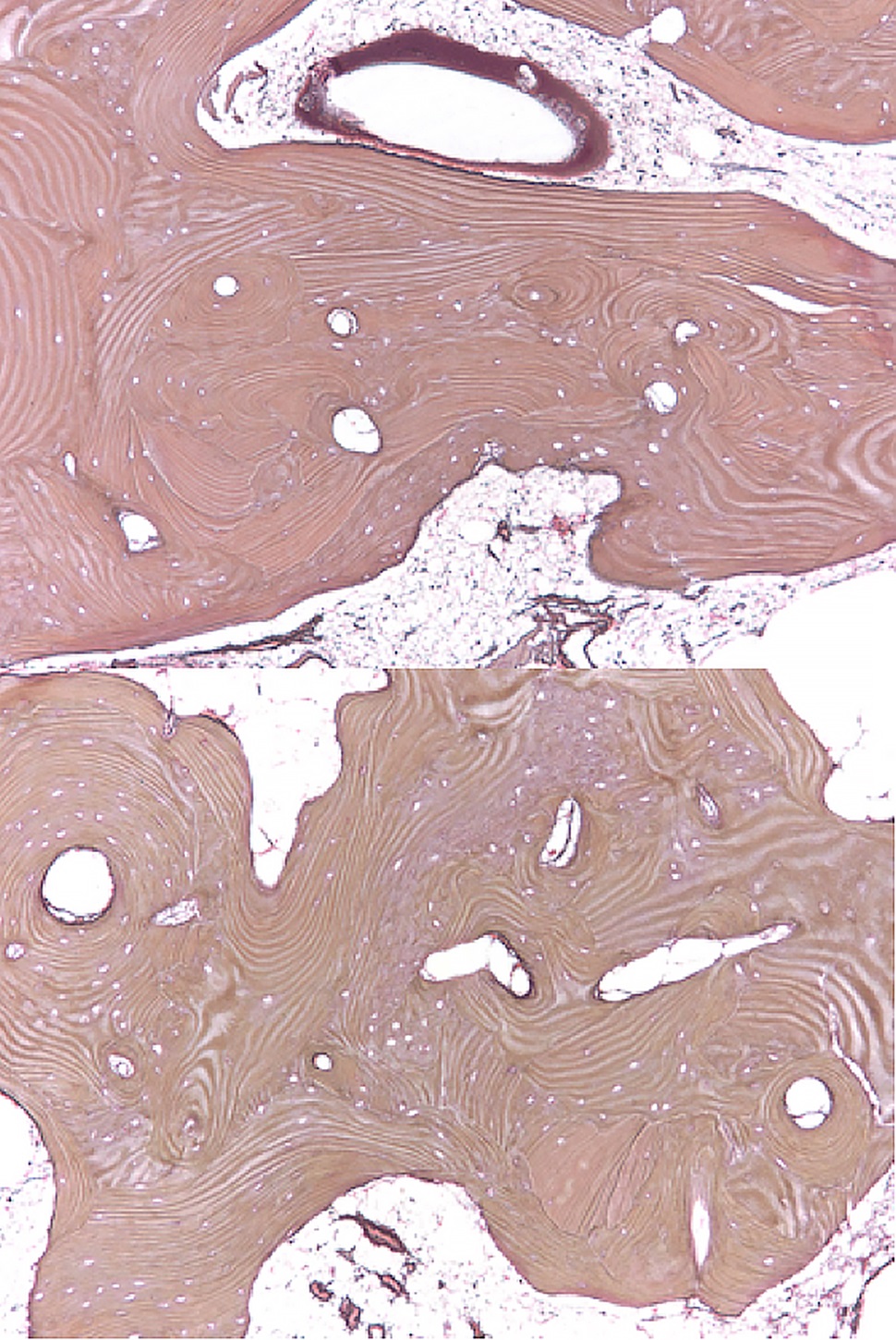
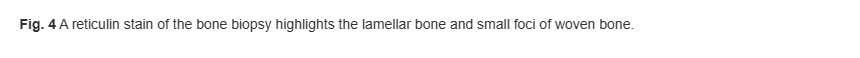
Bilateral posterior iliac crest bone biopsies were performed using a Michel needle and showed localized sclerosis of the medullary cavity with abundant lamellar and focal woven bone that had a cortical-like pattern, focal marrow fibrosis, and mild chronic inflammation (Figs. 3, 4, and 5). The initial treatment included standard doses of nonsteroidal anti-inflammatory drugs (NSAIDs) (naproxen 500 mg 2 times daily orally as required, tramadol 50 mg once daily, and 650-mg acetaminophen), 100-mg propoxyphene tablets sparingly for pain, sertraline 50 mg daily for depression, metoprolol 100 mg daily for hypertension, and standard bisphosphonates for presumed Paget disease of bone. Unfortunately, these did not provide substantial relief. The patient continued to have worsening diplopia, craniocervical pain, depression, and diffuse musculoskeletal pain in the extremities.
A sclerotic bone dysplasia workup with sequencing of the transforming growth factor beta 1 (TGFB-1) gene located on chromosome 19q13 revealed a heterozygous missense variant in exon-4.

