A 76-year-old woman presented to the emergency department reporting symptoms of left hip pain after a fall from her wheelchair.
At baseline, the patient required assistance with activities of daily living and used both a walker and a wheelchair for assistance. Her medical history was notable for atrial fibrillation, diastolic heart failure, pulmonary hypertension, type-2 diabetes, hyperlipidemia, and chronic kidney disease. She did not report substantial joint pain or swelling.
A screening dual x-ray absorptiometry (DXA) scan performed 3 days before her fall demonstrated a bone mass density (BMD) of the femoral neck as 0.631 g/cm2 (−2.0 T-score) and BMD of the left hip as 0.725 g/cm2 (−1.8 T-score). Based on these results, her 10-year risk for a major osteoporotic fracture was determined to be 13% and that for a hip fracture was determined to be 3.4%.
On examination, the patient was noted to have ecchymosis of the lateral soft tissues of the left hip and moderate tenderness to palpation over the greater trochanter and proximal part of the femur. Passive range of motion of the hip was limited, secondary to pain, but she maintained active knee flexion and extension.
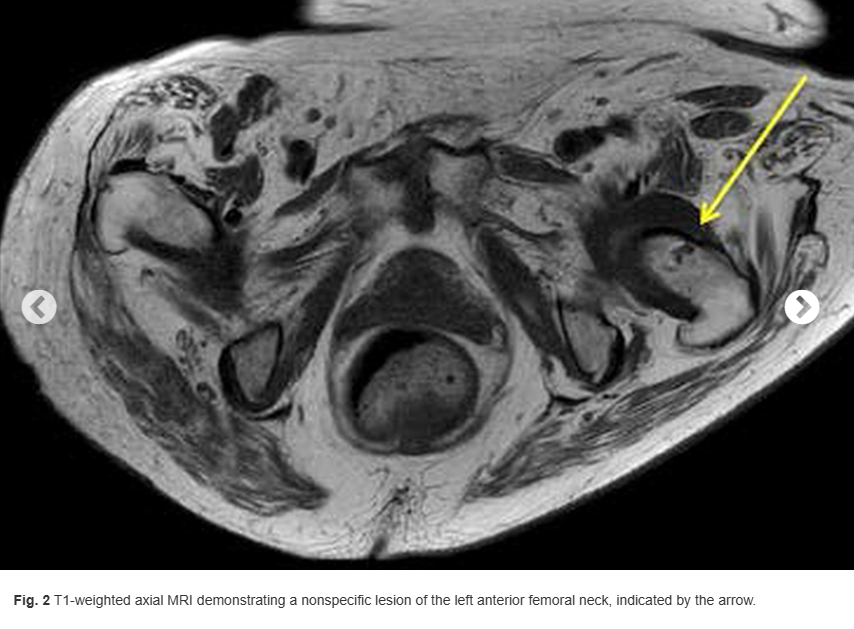
A radiograph of the left hip and pelvis demonstrated coxa profunda and Tonnis-2 osteoarthritis without evidence of fracture (Fig. 1). A computed tomography (CT) scan revealed osteopenia without evidence of a displaced fracture. Due to the relatively benign imaging and the patient’s inability to bear weight, a magnetic resonance image (MRI) was pursued to investigate an occult fracture. The MRI scans demonstrated a nondisplaced fracture of the femoral neck with an associated joint effusion (Figs. 2, 3, and 4). Laboratory evaluation revealed an elevated C-reactive protein (CRP) of 26 mg/L (<5-mg/L range) and a serum uric acid of 13.4 mg/dL (2.5 to 8.3-mg/dL range). Given her examination and associated imaging, the decision was made to proceed with an open biopsy, followed by operative fracture stabilization via cephalomedullary nailing pending biopsy results.



A lateral approach was chosen for the biopsy and cephalomedullary nail. Because the fascia was incised, light chalky-tinged fluid was encountered. On evaluation of the left femoral neck, powdery tissue with a large osseous cyst was identified. Once removed, the specimen was white in color with a chalky consistency and was sent for frozen section along with crystal and microbiologic evaluation. There was no displacement or gross instability at the fracture site with no suspicion of infection or malignancy on frozen section, so we proceeded with cephaomedullary nail fixation as planned.
In total, 4 specimens were sent for analysis: 1 from the femoral reamings and 3 from the femoral neck. Of the 3 femoral neck specimens, 2 were fixed in formalin and 1 was fixed in ethanol. The first specimen in formalin was a gray-dark green tissue measuring 1.2 × 0.9 × 0.1 cm. The second specimen in formalin was a gray-tan brown tissue measuring 1.3 × 0.5 × 0.5 cm. The third specimen was fixed in 100% ethanol. Hematoxylin and eosin (H&E)-stained sections are shown in Figure 5.
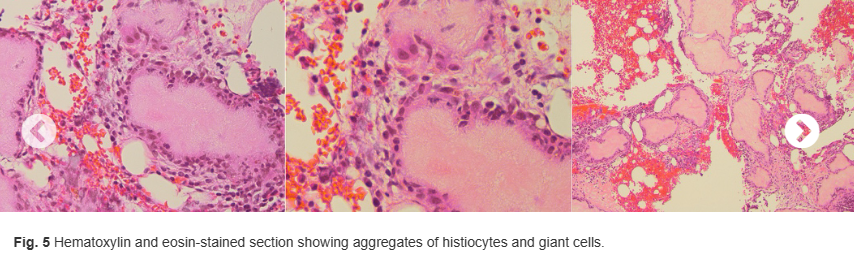
What is the diagnosis?

